Thursday, 22. May 2025
|
06:30 – 07:15
|
SCS Morning Run
Lorenz Ineichen, Steinhausen ; Kaja Widmer, Steinhausen
|
|
|
Social Program
|
||
|
08:00 – 08:30
|
Registration & Exhibition OpeningMorning Kick-Off: Visit the exhibition, connect with sponsors, and start your day with exclusive offerings from our partners. |
|
|
Break
|
||
|
08:30 – 10:00
Room 5C
|
ARS - Free Communication
Alexandre Balaphas, Geneva; Stephanie Gros, Basel
|
|
|
Free Communication
|
||
|
08:30–08:37
Plasma fibronectin released by peritoneal macrophages promotes remote skin wound healing
Lilian Salm, Bern / Calgary
AbstractBackgroundLarge peritoneal macrophages (LPMs), located in the peritoneal cavity, are essential for local tissue repair. However, their contribution to tissue repair at distant sites remains unclear. AimsThis study investigates the role of LPM activation in skin wound healing at remote sites MethodsA novel mouse model combining peritoneal stimulation (PS) with a skin injury was used to assess LPM-mediated effects on remote skin wound healing. Dual Cre and Flippase fate-mapping tracked GATA6-expressing LPMs to evaluate their migratory behavior. Parabiosis experiments and administration of activated peritoneal fluid were conducted to identify the role of circulating factors. Proteomic and transcriptomic analyses were used to characterize LPM-secreted molecules. Fluorescently labelled fibronectin was tracked in plasma and skin wounds. ResultsActivation of LPMs trough PS significantly accelerated healing of remote skin wounds. Removing LPMs or using mice lacking LPMs abolished the beneficial effect. Adoptive transfer of LPMs but not B-cells after LPM depletion was sufficient to rescue the phenotype. Fate-mapping demonstrated that LPMs did not migrate to distant wounds after activation. Parabiosis and peritoneal fluid transfer experiments indicated the role of LPM-derived circulating signaling molecules in remote skin wound healing. Proteomic and transcriptomic analyses identified fibronectin as critical mediator, as adoptive transfer of LyzMcre Fnflox peritoneal cells failed to rescue the impaired remote wound healing phenotype in LPM deficient mice. Protein-coding fibronectin isoforms transcribed by LPMs, correspond to the soluble plasma. Fluorescently labelled fibronectin was detected in the plasma and incorporated into skin wounds following adoptive transfer of Fngfp/gfp peritoneal cells and PS. ConclusionLPMs act as a source of circulating fibronectin, facilitating extracellular matrix formation and promoting wound healing at remote sites. These findings reveal a novel endocrine role for LPMs in systemic tissue repair, and challenge the traditional perspective, that plasma fibronectin is exclusively liver-derived. |
||
|
08:40–08:47
Preoperative Enterosignatures Predict Surgical Site Infections After Abdominal Surgery
Simone Zwicky, Bern
AbstractBackgroundThe relationship between preoperative intestinal microbiota composition and the development of surgical site infections (SSIs) following abdominal surgery is not well understood. AimsThe aim of this study was to characterize the preoperative rectal microbiota using the novel concept of enterosignatures (ESs) in patients undergoing abdominal surgery and assess their association with SSIs. MethodsIn this prospective cohort study, preoperative rectal microbiota from 133 patients undergoing abdominal surgery was profiled using 16S rRNA sequencing. ESs were calculated using high-quality genus-level taxonomy, simplifying complex microbial compositions into five generalizable patterns: Bacteroides, Firmicutes, Prevotella, Bifidobacterium, or Escherichia-dominated profiles. ResultsA total of 519 bacterial species were identified within the 133 patients. The Firmicutes ES was found to be a significant risk factor for SSIs, while the Prevotella ES was associated with a reduced risk of SSIs. Combining these into the Firmicutes-to-Prevotella ES ratio (ES-Firm-Prev ratio) yielded a stronger association with SSIs (median [IQR] log ES-Firm-Prev ratio: no SSI, 0.21 [-0.43, 1.33] vs. SSI, 8.24 [2.17, 8.5]; p = 0.001). Machine learning and logistic regression models confirmed the ES-Firm-Prev ratio as a significant predictor of SSIs, independent of clinical covariates (OR, 1.39; 95% CI, 1.08-1.78; p = 0.01). ConclusionThe ES-Firm-Prev ratio is a robust, independent predictor of SSIs in patients undergoing abdominal surgery and may serve as a novel biomarker to identify high-risk patients preoperatively. |
||
|
08:50–08:57
Expression levels of GATA6 in human peritoneal macrophages
Agnes Huber, Bern
AbstractBackgroundThe important role of GATA6+ tissue macrophages in wound healing has been demonstrated by our group in the murine peritoneal cavity [2]. Investigations regarding the existence and significance of these GATA6+ macrophages in humans has been researched only modestly possibly due to limited access and published studies are controversial [3, 4]. AimsI aim to isolate peritoneal immune cells from different anatomical regions and improve the immune cell sampling process. Then on I will investigate the function of peritoneal macrophages. MethodsWe developed a robust workflow to isolate primary peritoneal cavity immune cells from the peritoneal fluid and omental biopsies obtained during laparoscopic surgeries of diverse patient cohorts. The isolated immune cells were analyzed with flow cytometry and real-time PCR to investigate the levels of GATA6 expression in these patients. Furthermore, omental biopsies were stained with H&E to identify milky spots as possible GATA6+ macrophage storage place. ResultsOur study demonstrates that factors such as neoadjuvant chemotherapy, patient sex or BMI, peritoneal fluid volume, nor the peritoneal rinsing fluid temperature correlate with the immune cell yield from the peritoneal fluid. Importantly, the analysis of GATA6 expression by flow cytometry and real-time PCR showed patient dependent expression variations. ConclusionWe observed that neither the patients' medical treatment nor their BMI significantly affected the number of immune cells isolated from the peritoneal fluid. Furthermore, we were able to show that levels of GATA6 expression are varying in the patient cohort. This study aims to provide insight into the human peritoneal immune cell composition, depicting differences from murines to humans and will significantly contribute to the understanding of the function peritoneal macrophages leading to therapeutical applications. 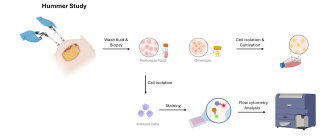
|
||
|
09:00–09:07
Characterization of liver sinusoidal endothelial cell and immune cell subpopulations during mouse liver regeneration
Carmen Gonelle-Gispert, Fribourg
AbstractBackgroundThe specialised liver sinusoidal endothelial cells (LSEC) are important in normal liver physiology, and their dysfunction has been implicated in many diseased states of the liver. Primarily, their phenotype in normal or diseased liver has been assessed by immunofluorescence studies, but their characterisation remains limited. AimsIn this study, we aim to characterise subsets of endothelial cells and immunoinflammatory populations associated with liver homeostasis using the high-dimensional flow cytometry. MethodsMethods: We established an antibody panel of 18 antibodies to identify surface antigens on endothelial cells and immune cell populations. We isolated non-parenchymal liver cells (NPLC) from wild-type Bl6/57 mice using OptiPrep™ Density gradient combined with gradient centrifugation and performed cell population analysis on a full spectral flow cytometer. First dimensionality reduction of 3 full panel-stained NPLC using the t-distributed Stochastic Neighbor Embedding (t-SNE) algorithm for visualising high-parameter single-cell data and to characterize cell populations defined by it. ResultsFirst analysis allowed us to distinguish in the Stab2+/CD31+/CD45- LSEC population, a population high for Lyve1/CD146/CD54/CD32 representing LSEC from zone 2/3 of the liver lobule as well as a population low for Lyv1/CD146/CD54 representative for the LSEC population in zone 1. Other cell clusters expressing high CD45/CD16/CD38 or high CD45/CD54 can be distinguished. Identification of the different cell populations and optimising reference controls are ongoing. ConclusionIdentification of endothelial cell populations and immune cell populations by full spectral flow cytometer in the healthy mouse is ongoing. As a second step, we will look forward to identifying new cell populations during regenerative conditions. |
||
|
09:10–09:17
Extended EVLP protocol combined normothermic and subnormothermic conditions for reconditioning and preservation of damaged rat donor lungs
Roumen Parapanov, Epalinges / Lausanne
AbstractBackgroundEx vivo lung perfusion (EVLP) has been developed to evaluate the quality of donor lungs before transplantation. EVLP may also serve as a platform, allowing administration of various therapies to the lungs. AimsWe explored whether a mixed EVLP protocol combining normothermic and subnormothermic conditions would improve the quality of damaged rat donor lungs. MethodsRats were assigned into 2 groups (n=5 per group): Normothermic EVLP (Nth) and Normothermic/Subnormothermic EVLP, (N/Sth). In both groups lungs were kept in situ for 1h at room temperature, warm ischemia, then lungs were flashed with cold Perfadex® and kept for 1h at 4°C. Heart-lung blocks were mounted on the EVLP. In the Nth group lungs were perfused under normothermic conditions at 37°C for 6h. In the group N/Sth lungs were also perfused for 6h, first 3h under normothermia, then the perfusate temperature was reduced to 22° C, as well as ventilation and perfusion rates were also slow down to the end of EVLP. At the end of EVLP perfusates and lung tissues were collected and frozen at -80°C for further analysis. ResultsLungs in the N/Sth group displayed improved compliance, and reduced edema, associated with reduced perfusate levels of lung endothelial and epithelial cell damage markers (vWF, SP-D, sPECAM-1), cytokines (IL-1β, and TNF-α) and lactate, comparing to Nth group. Moreover, increased production of cell protective proteins such as HSP70, antiapoptotic proteins (Bcl-2, Bcl-xL) and antioxidant (SOD2) was observed in N/Sth group. ConclusionCombination of normothermic and subnormothermic conditions during EVLP could be a promising experimental model providing improved cytoprotective status and preserved function of damaged donor lungs in an extended EVLP model. Our findings demonstrated that combination of normothermic and subnormothermic conditions during EVLP, allows safe extension of EVLP for possible treatments engaging prolonged perfusion time, while maintaining lungs in stable physiological state. |
||
|
09:20–09:27
Exosomal RNA Profiling Identifies GAS5 and Other Long Noncoding RNAs as Circulating Diagnostic Biomarkers for Pleural Mesothelioma
Agnieszka Kraft, Zürich / Zurich
AbstractBackgroundPleural mesothelioma (PM) is a rare but highly lethal cancer for which early, non-invasive diagnostic tools are critically lacking. RNAs secreted by tumor cells via exosomes (Exo) are detectable in plasma and have emerged as promising biomarkers for non-invasive disease diagnosis. AimsThis study aimed to compare the RNA cargo of exosomes secreted by primary PM cells with those from non-PM cells, to identify circulating biomarkers that potentially could be used as blood-based diagnostic biomarkers for PM. MethodsPrimary cell cultures were established from pleural effusions of 12 PM and 7 non-PM patients. Exosomes were isolated from cell culture supernatants using iZON qEV columns, followed by total RNA extraction using the mirVana PARIS kit and RNA sequencing. Sequencing reads were mapped to the human reference genome (GRCh38), and differential expression analysis was performed using DESeq2 to identify RNAs enriched in PM-derived exosomes. Candidate RNAs were validated in exosomes and plasma samples from PM and non-PM patients. ResultsWe identified 2,089 RNAs upregulated in PM-derived exosomes (p < 0.05, Fig. 1A), with the majority comprising long noncoding RNAs (lncRNAs) (34%), pseudogenes (30%), and protein-coding genes (27%). Enriched biological processes included proliferation, protein secretion, and epithelial-mesenchymal transition, all hallmarks of tumorigenesis (Fig. 1B). Among the lncRNAs, GAS5 - a gene previously implicated in cancer - emerged as a particularly promising candidate for PM diagnosis. Quantitative-PCR validation confirmed significantly higher GAS5 expression in exosomes from PM compared to non-PM samples (Fig. 1C). ConclusionThis study provides a comprehensive analysis of exosome-secreted RNAs in PM, identifying candidate biomarkers for blood-based diagnostic tests. Our findings underscore the critical role of the PM secretome in understanding PM biology and highlight GAS5 as a strong diagnostic candidate. We are currently validating these biomarkers in pleural effusion and plasma-derived exosomes to further establish their clinical utility. 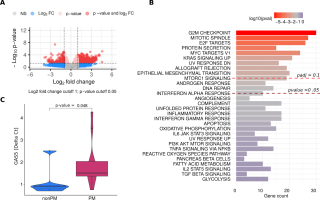
|
||
|
09:30–09:37
NeoAdjuvant or Adjuvant Use of Immune Checkpoint Inhibitors in Surgery for Hepatocellular Carcinoma
Sofia El Hajji, Genève / Geneva
AbstractBackgroundHepatocellular carcinoma (HCC) often recurs after curative hepatectomy. Immune checkpoint inhibitors (ICIs), such as anti-PD-1 therapies, show promise into diminishing recurrence, but the optimal timing for ICI administration (pre- or post-hepatectomy) remains unclear. We hypothesize that neoadjuvant ICIs may be more effective in decreasing recurrence and enhancing survival outcomes, while adjuvant treatment could be hindered by immunosuppression induced by surgery. AimsTo assess survival and recurrence rates between neoadjuvant and adjuvant regimens and evaluate their effects on tumor growth. MethodsC57BL/6 mice were injected with bioluminescent RIL-175 HCC cells into the right median lobe. In the first experiment, mice underwent curative hepatectomy and were treated with anti-PD-1 either in a neoadjuvant or adjuvant setting compared to a sham treatment with isotype antibodies. In the second experiment, hepatectomy of the left median lobe was performed, leaving the tumor in place, allowing assessment of tumor growth which was monitored using intra-vital imaging system. Immune tumor microenvironment was assessed by flow cytometry. ResultsNeoadjuvant anti-PD-1 therapy significantly reduced recurrence rates compared to sham (35% vs. 68%, p=0.041) and improved survival (p=0.0373), while adjuvant therapy showed no significant benefit (recurrence 50% vs. 68%, p=0.253). Neoadjuvant therapy slowed tumor growth compared to adjuvant therapy (p=0.016). Anti-PD-1 immunotherapy without surgery enhanced CD8+ T cell migration in the tumor and reduced exhaustion markers, while these effects were abolished post-hepatectomy (CD8+CD103+, no surgery 17% vs hepatectomy/adj_ICI 5.72%, p=0.014). ConclusionNeoadjuvant anti-PD-1 therapy improves survival, recurrence and tumor growth reduction compared to adjuvant therapy in our mouse model, suggesting that neoadjuvant treatment may be more effective. These findings support further investigation into neoadjuvant ICI strategies. |
||
|
09:40–09:47
Comparison of elastic stable intramedullary nailing versus retrograde screw fixation for pubic ramus fractures - a biomechanical study
Julian Scherer, Zurich / Cape Town
AbstractBackgroundRecently, elastic stable intramedullary nailing (ESIN) devices have been proposed as an alternative to retrograde screw fixation in the treatment of superior ramus fractures. AimsThe aim of this study was to compare the biomechanical stability of ESIN in pubic ramus fractures versus retrograde screw fixation. MethodsStandardized pubic ramus fractures (Nakatani type II) were created in fresh-frozen paired hemipelves. Fractures were either stabilized with a 6.5mm cannulated screw (n=4) or a 3.5mm Stainless Steel Elastic Nail System (n=4). Cyclic loading protocol was applied with increasing axial force (1500 cycles, 250-750 N). Outcome parameters were fracture mobility over time, fracture displacement and construct survival. Descriptive and opto-metric methods were used to describe the mode of failure. ResultsAmongst all hemipelves, no construct failure was observed. There was no significant difference in mean vertical fracture displacement between the groups (ESIN 0.07 mm, SD 0.12 versus screw 0.04 mm, SD 0.05; p=0.773). After 500 cycles at 250 N, mean vertical fracture displacement was 0.09 mm (SD 0.16) in the ESIN group and 0.03 mm (SD 0.04) in the screw group (p=0.773). After subsequent 500 cycles at 500 N in the vertical plane, mean fracture displacement increased to 0.35 mm (SD 0.31) in the ESIN group and to 0.14 mm (SD 0.17) in the screw group (p=0.281). With a maximum load of 750 N, after 500 cycles, mean fracture displacement was 0.58 mm (SD 0.51) in the ESIN group and 0.31 mm (SD 0.26) in the screw group (p=0.376). There was no difference between the implants regarding the accumulated fracture movement over time (ESIN 494 mm*cycles, SD 385 versus screw 220 mm*cycles, SD 210; p=0.259). ConclusionIn this in-vitro biomechanical study, fixation of superior ramus fracture using ESIN was not different in construct survival, relative motion to fracture, and fracture displacement when compared to retrograde screw fixation |
||
|
09:50–09:57
DNA replication stress in metabolic dysfunction-associated steatohepatitis
Ainhoa Asensio Aldave, Bern
AbstractBackgroundMASLD is an increasing health global problem characterized by the accumulation of liver-fat. MASLD patients can progress to MASH, a more severe stage of the disease characterized by liver inflammation and an oxidative stress background. These two hallmarks are believed to drive HCC formation, although the molecular mechanisms are not well understood. AimsCharacterize the molecular mechanisms that drive inflammation and oxidation stress backgrounds in MASH livers to cause HCC formation. MethodsMC4R KO mice were fed with a chow or a western diet and harvested at 33-38 weeks to develop MASLD and MASH, respectively. These mice do not feel satiation and therefore gain weight quicker. WT mice under a chow diet were used as a control healthy group. Liver samples were collected and embedded in paraffin for histology, or snap frozen for RNA/protein extraction. ResultsWe first confirmed that MASH livers, unlike control or MASLD, present high immune infiltration (histology) and upregulated inflammation response (RNAseq). MASH livers in addition have an upregulated response to oxidative stress (RNAseq) and accumulate 8-oxo-2’deoxyguanosine (histology), one of the major products of DNA oxidation, which is also observed in MASLD livers. When keeping the MASH mice for longer periods (45-68 weeks) they all develop HCC tumors (reticulin staining). DNA oxidation is likely to induce mutations when amplified, therefore we checked for replication stress: MASH livers presented significantly more Ki67 hepatocyte protein expression (histology quantification) and had an upregulation of genes involved in cell cycle (RNAseq). Moreover, genes and proteins involved in different DNA damage repair pathways were upregulated (RNAseq, WB). ConclusionMASH inflammation and oxidative stress lead to chronic proliferation, which will amplify the mutations and generate more DNA damage by replication stress, ultimately driving to HCC formation. |
||
|
08:30 – 10:00
Room 1B
|
Controversies in Colon Surgery
Antonio Nocito, Baden; Daniel Steinemann, Basel
|
|
|
Main Session
|
||
|
08:30–08:45
Diverticulitis – is it only about quality of life?
Seraina Faes, Zurich
|
||
|
08:45–09:00
Crohn’s Disease – is Kono S really the new standard?
Benjamin Weixler, Winterthur
|
||
|
09:00–09:15
T1 polyp cancer – who can, should or should not get surgery?
Emilie Liot, Geneva
|
||
|
09:15–09:30
Complete mesocolic excision – always or selectively?
Fabian Grass, Lausanne
|
||
|
09:30–09:45
Is a robot mandatory for colon cancer surgery?
Marco von Strauss, Basel
|
||
|
09:45–10:00
From ERAS to 23 hours colectomy – is the rush worthwhile?
Georgios Popeskou Sotirios, Bellinzona
|
||
|
08:30 – 10:00
Room 1C
|
Guardian of the Scalpel: Securing excellence in the management of the adolescent with blunt abdominal trauma
Nicolas Lutz, Lausanne; Tobias Zingg, Lausanne
|
|
|
Guardians of the Scalpel
|
||
|
08:30–08:45
Insight into the Swiss registries
Mylène Bourgeat, Lausanne
|
||
|
08:45–09:00
Blunt splenic trauma conservative management
Anthony Di Natale, Zurich
|
||
|
09:00–09:15
Blunt splenic trauma: take it out!
Steffen Geuss, Lucerne
|
||
|
09:15–09:30
The Interventional radiology perspective
Frédérique Gay, Lausanne
|
||
|
09:30–09:45
The adolescent perspective: age limit and sports behaviour
Lara Gamper, Zurich
|
||
|
10:45–11:00
Round Table Discussion |
||
|
08:30 – 10:00
Auditorium B
|
Guardians of the Scalpel: Securing excellence in surgical residency
Rebecca Kraus, Chur; Markus K. Müller, Frauenfeld
|
|
|
Guardians of the Scalpel
|
||
|
08:30–08:45
Mentorship
Emilie Uldry, Lausanne
|
||
|
08:45–09:00
Securing surgical exposure
Pascal Probst, Frauenfeld / Heidelberg
|
||
|
09:00–09:15
How to teach in surgery
Phaedra Müller, Winterthur
|
||
|
09:15–09:30
Is research exposure necessary for a surgeon
Lilian Salm, Bern / Calgary
|
||
|
09:30–09:45
Pre-existing personal qualities of a surgeon
Christian Toso, Geneva
|
||
|
09:45–10:00
What about work-life balance
Diana Mattiello, Schlieren
|
||
|
08:30 – 10:00
Room 4A
|
PA – The extended arms of the guardians of the scalpel : pain or gain, round two !
Michael Winiker, Lausanne; Dorothee Schregel, Winterthur
|
|
|
Main Session
|
||
|
08:30–08:45
A PAs perspective – where am I going
Sandrine Worreth, Lausanne
|
||
|
09:00–09:15
Pain or gain – what do we PAs think of it
Mirjam Roth, Winterthur; Rahel Käufeler, Zürich
|
||
|
09:30–09:45
Small pain but giant gain - implementation of PAs into the Swiss Army
Annmarie Monnard, Winterthur
|
||
|
08:30 – 10:00
Room 5B
|
Pancreas
Emmanuel Melloul, Lausanne; Beat Müller, Basel
|
|
|
Free Communication
|
||
|
08:30–08:37
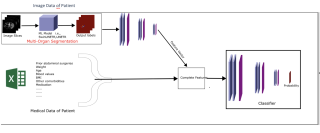
Pancreatic Resectability Evaluation through Deep Imaging with Computed Tomography in Pancreatic Cancer (PREDICT-PanC).
Vincent Ochs, Allschwil
AbstractBackgroundPancreatic ductal adenocarcinoma (PDAC) has the highest mortality rate among solid malignancies worldwide, with surgical resection as the only curative treatment. The assessment of PDAC resectability, which depends on the accurate assessment of vascular infiltration, suffers from low inter-observer reliability. AimsThis study develops a multi-modal deep learning algorithm to automate the resectability assessment of PDAC using contrast-enhanced Computed Tomography (CT) images, clinical parameters, and radiomic features, aiming to enhance accuracy and reduce subjective interpretation discrepancies. MethodsWe analyzed 173 contrast-enhanced CT scans showing various degrees of vascular infiltration. PDAC masks were generated using both manual labeling and predictions from the Monai-Label framework, validated by expert surgeons (Figure 1). Our methodology employs a multi-modal approach, integrating convolutional neural networks (CNNs) with transformer modules to enhance the extraction of dynamic texture patterns from multi-phase CT images (Figure 2). Attention mechanisms focus on significant features across the imaging and clinical data, including radiomic features extracted for their potential to indicate vascular involvement and tumor characteristics. This integrative approach aims to achieve more precise segmentation and refined predictive analysis. ResultsThe algorithm, tested via a nested 5-fold cross-validation, achieved a Dice Similarity Coefficient (DSC) of 83.2%. Specific DSC scores for the Superior Mesenteric Vein (SMV), Superior Mesenteric Artery (SMA), and tumor were 72.1%, 75.7%, and 80.4%, respectively. Additionally, it attained an F1 Score of 85% in predicting NCCN-based resectability criteria. ConclusionThe multi-modal deep learning framework has demonstrated significant potential in segmenting PDAC on CT scans and predicting surgical resectability. Future work will refine the model by incorporating more clinical parameters to improve predictions of vascular involvement and overall surgical outcomes. The anticipated next steps include further validation and preparation for widespread clinical application. 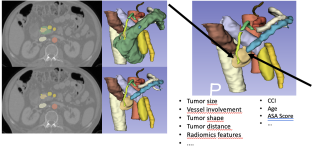
|
||
|
08:40–08:47
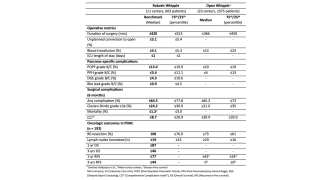
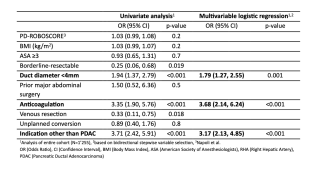
Novel Benchmarks for Robotic Whipple Surgery - A Global Multicenter Cohort Study
Matthias Pfister, Zurich
AbstractBackgroundRobotic Whipple holds the promise to overcome safety concerns associated with laparoscopy, paving the way for widespread implementation of minimal-invasive surgery in this complex procedure. However, randomized data comparing robot vs. open Whipple demonstrate more pancreas-specific complications and R1-resections in the robotic arm. Recent international consensus identified establishing benchmarks as critical to ensure safe adoption of the robot. Benchmarking is a validated quality improvement tool, enabling comparison of surgical performance. AimsThe aim was to define benchmarks for outcome parameters in robotic Whipple. MethodsWe analyzed consecutive patients undergoing robotic Whipple from January 2020 until December 2023 in 11 centers across 4 continents, with a minimum one-year follow-up. Centers had to perform ≥15 cases/year and have mounted their learning curve. Benchmark criteria included benign or resectable malignant disease without neoadjuvant therapy, arterial resection, major co-morbidities, or significant previous abdominal surgery. Medians across centers represented benchmark cutoffs. ResultsEleven centers performed 1’037 Whipple procedures, of which 603 (58%) were benchmark cases (Figure 1). One third (n=192) were pancreatic ductal adenocarcinoma (PDAC) patients. Key benchmarks at 6 months included ≤1.2% mortality, ≤24.2% major complications, and ≤ 8.7 points Comprehensive Complication Index® (Table 1). Pancreas-specific cutoffs included ≤13.0% postoperative pancreatic fistula (POPF) B/C and ≤3.4% post-pancreatectomy hemorrhage B/C, with 100% R0-resection and ≥19 harvested lymph nodes in PDAC patients. One-year actuarial overall and recurrence-free survival was 87% and 77%. In the entire cohort POPF B/C occurred in 16% (n=195). Independent POPF predictors included duct diameter ≤4mm (OR 1.79 95%CI [1.27-2.55]), anticoagulation (OR 3.68 95%CI [2.14-6.24]), and indication other than PDAC (OR 3.17, 95%CI [2.13-4.85]) (Table 2). ConclusionThis study establishes benchmarks for key outcomes in robotic Whipple, demonstrating oncologic adequacy and morbidity comparable to open surgery. Risk factors for POPF in open surgery also hold true in the robotic approach. 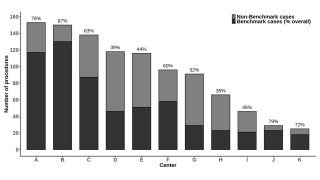
|
||
|
08:50–08:57
Defining Global Benchmarks for Total Pancreatectomy: A multicenter study from 22 International Expert Centers
Christoph Kümmerli, Basel
AbstractBackgroundTotal pancreatectomy (TP) is the preferred treatment for patients with advanced pancreatic cancer or multifocal pancreatic tumors. Furthermore, in patients with concomitant vascular resections, TP may be performed to avoid the risk of pancreatic fistula and thus improve the perioperative risk profile. AimsTo enable conclusive comparisons with other types of pancreatic resections and among different centers, international benchmark values are urgently needed. The aim of this international multicenter study was to identify the first benchmark values for TP from international expert centers. MethodsThis multicenter study analyzed outcomes from patients undergoing primary TP for malignant or benign lesions from 22 international expert centers. Patients were included from January 2017 up to November 2023 with a minimum follow-up of 1 year in each patient. Fifteen benchmark values were identified, and were compared to a cohort of TP with vascular resection and the published multi-national benchmark values for pancreatoduodenectomy (PD). Benchmark patients were without significant comorbidities, age <80 years, cardiac disease, chronic pulmonary disease and renal failure. Results553 (74%) of a total of 749 patients qualified as benchmark cases. The proportion of benchmark patients varied between 50%-100% per center. All benchmark values are disclosed in Figure 1. For example, benchmark cut-offs showed relevant 6 month- postoperative mortality (<6.8%) and major morbidity (≤44.2%). Especially benchmark values for pancreas specific morbidity such as delayed gastric emptying (≤41.2%) and postoperative hemorrhage (≤26.2%) were high. Benchmark cutoffs were further defined for operative time (≤510min), CCI at 6 months (≤27.3), and hospital stay (≤18 days). For ductal adenocarcinoma benchmark cutoffs for number of lymph nodes were ≥22 with an R0 resection rate of > 69.1%. Compared to the published PD, benchmark values for TP for overall- and pancreas specific complications were markedly higher. Furthermore the cohort of patients with TP and concomitant vascular resections displayed several outcomes outside the TP benchmarks, for example a 90-mortality rate of 8% and major morbidity rate of 54% (Figure 1). ConclusionThis benchmark analysis sets the first global reference values for TP, indicating significantly higher postoperative morbidity and mortality as compared to PD. The inferior outcomes were especially observed in TP with vascular resections. These reference values serve for quality control of pancreatic surgery in different centers, countries or surgical techniques. 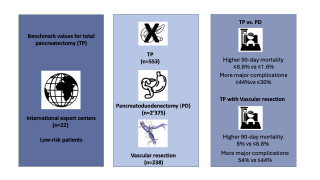
|
||
|
09:00–09:07
International Validation of the Distal Pancreatectomy Fistula Risk Score – More Than a Throw of the Dice?
Suna Erdem-Sanchez, Basel
AbstractBackgroundPostoperative pancreatic fistula (POPF) remains the most severe complication following distal pancreatectomy (DP). The preoperative distal fistula risk score (D-FRS) was recently introduced to predict the POPF risk. AimsThe aim of this study was to externally validate the D-FRS in an international expert center cohort. MethodsThis international, multicenter, retrospective cohort study included open and minimally invasive DP for benign and malignant lesions performed from 01/2014 until 12/2023 in 12 centres from 6 countries, that each performed more than 50 pancreatectomies annually. The D-FRS was calculated from pancreatic thickness and duct size. Predicted and actual POPF were compared using sensitivity, specificity and area under the curve (AUC). ResultsA total of 778 patients underwent DP of whom 284 (39%) underwent robotic, 278 (38%) open and 165 (23%) laparoscopic DP. The rate of POPF was 32%. In the POPF group, the D-FRS was 0.21 (0.13-0.33), while in the no-POPF group it was 0.23 (0.15-0.36). The sensitivity, specificity and AUC of the D-FRS for the overall cohort was 32%, 63% and 48% (95% CI 44-51), respectively. The AUC for open, laparoscopic and robotic DP was 54% (48-60), 47% (39-55) and 45% (39-50), respectively. On multivariate analysis POPF was associated with BMI (odds ratio 1.04 (95% CI 1.01-1.07)), protective factors were neoadjuvant therapy (OR 0.54 (0.22-0.94)) and robotic approach (OR 0.64 (0.42-0.97)). ConclusionThe preoperative D-FRS showed insufficient discrimination to identify patients who develop POPF after DP irrespective of the surgical approach. Novel preoperative POPF risk scores are needed, taking into account the standard robotic approach and the widespread application of a no-drain policy. |
||
|
09:10–09:17
Early enteral vs. oral postoperative nutrition after pancreatoduodenectomy: an international multicentric randomized controlled trial (NUTRIWHI trial)
Gaëtan-Romain Joliat, Lausanne / Bern
AbstractBackgroundThe best nutrition route (oral, enteral, or parenteral) after pancreatoduodenectomy (PD) remains controversial. AimsThis study aimed to compare early enteral nutrition (EEN) to oral nutrition after PD in malnourished patients in terms of postoperative morbidity. MethodsThis study was a multicentric (3 centers) randomized controlled trial. Patients with nutritional risk screening >2 were randomized 1:1 into the EEN or oral nutrition group. Patients in the EEN group received enteral nutrition from the operation night via a nasojejunal tube placed intraoperatively and were allowed to have oral food based on the same protocol as the other group. Patients in the oral group were not allowed to have enteral nutrition during hospitalization. In both groups, parenteral nutrition need was standardized. Complications were measured at 90 days postoperatively using the Clavien classification and Comprehensive Complication Index (CCI). ResultsA total of 144 patients were included and randomized. Twenty-five patients dropped out (17%), leaving 119 patients for analysis (60 EEN group and 59 control group). At 90 days, morbidity rates were 45/60 and 54/59 in the EEN and oral nutrition groups (p=0.016), while no difference was found between both groups regarding specific complications (delayed gastric emptying, pancreatic fistula, postoperative hemorrhage, and surgical-site infection). Patients with EEN had a lower mean 90-day CCI compared to patients with oral nutrition (24±19vs. 38±24, p<0.001). In the EEN group, 13 patients involuntarily removed their nasojejunal tube. ConclusionIn malnourished patients, EEN after PD permitted to decrease the burden and incidence of postoperative complications compared to oral nutrition. |
||
|
09:20–09:27
Risk Factors and Consequences for Conversion in Robotic Distal Pancreatectomy – an International Multicenter Study
Christoph Kümmerli, Basel
AbstractBackgroundRobotic distal pancreatectomy (RDP) has gained popularity because of its lower conversion rates and potential advantages over laparoscopic distal pancreatectomy (LDP), particularly in challenging patients. AimsThe aim of this study is to identify and analyze the risk variables associated with RDP conversion to open surgery, with an emphasis on surgical outcomes and patient safety. MethodsThis international multicenter study analyzed retrospective data from 2403 patients who had RDP. Patient demographic information, intraoperative measurements, and postoperative outcomes were all included. Statistical analysis was utilized to determine variables for conversion to open surgery and their association with conversion rates. ResultsThe overall conversion rate was 2.6 percent. Older age and greater lesion sizes were significant risk variables for conversion. Converted patients had higher rates of postoperative complications, including major complications (Clavien-Dindo ≥ IIIa) and pancreatic-specific difficulties such as postoperative pancreatic fistulas (POPF) and delayed stomach emptying (DGE). ConclusionThe conversion rate was compared to literature very low but had a significant impact on the further outcome of the patient. In case of conversion, the total amount of complications as well as the severity and the regarding need for further intervention was higher. Lesion size or the age of the patient seem to be associated with conversion. Addressing the identified risk factors can lead to improved surgical outcomes and reduced complication rates, further establishing RDP as a safe and effective option. |
||
|
09:30–09:37
Survival in Locally Advanced Pancreatic Cancer: Surgery vs Radiation after Neoadjuvant Chemotherapy
Suna Erdem-Sanchez, Basel
AbstractBackgroundLocally advanced pancreatic cancer (LAPC), defined by local progression and invasion of major vessels, has traditionally been considered unresectable. Advances in neoadjuvant chemotherapy and surgical techniques have improved resection rates, but reliance solely on post-neoadjuvant imaging may misclassify resectability, potentially denying curative surgery to eligible patients. AimsThis study evaluates survival outcomes of surgical resection versus radiotherapy after neoadjuvant chemotherapy in LAPC. MethodsThis retrospective study reviewed patients diagnosed with histologically confirmed pancreatic ductal adenocarcinoma (PDAC) from 2016 to 2024, meeting the National Comprehensive Cancer Network (NCCN) criteria for LAPC. Patients received either FOLFIRINOX or Gemcitabine-based chemotherapy, followed by surgery or radio(chemo)therapy (RCT). Survival outcomes were assessed using Kaplan-Meier curves and Cox regression analysis. ResultsAmong 42 patients treated with neoadjuvant FOLFIRINOX or Gemcitabine/nab-Paclitaxel, 20 underwent surgery and 22 received RCT. Re-staging after neoadjuvant chemotherapy showed no disease progression or metastasis in any patient. Pre-treatment CA 19.9 levels were 223.5 U/ml in the surgery group and 244 U/ml in the RCT group, decreasing to 38.65 U/ml and 85 U/ml post-treatment, respectively. R0 resection was achieved in 19 of 20 surgery patients (95%). Kaplan-Meier analysis demonstrated significantly better overall survival in the surgery group (log-rank p = 0.0009). At 12, 24, and 36 months post-treatment, survival rates were higher in the surgery group (19, 13, and 10 alive) compared to the RCT group (17, 9, and 3 alive). Multivariable Cox regression showed RCT was associated with significantly higher mortality risk compared to surgery (HR = 0.2539, 95% CI: 0.1129–0.5710, p < 0.001). ConclusionThis study demonstrates that surgical resection after neoadjuvant chemotherapy significantly improves survival compared to RCT. Surgical resection should be attempted in patients without progress after neoadjuvant therapy since surgery achieves superior survival. 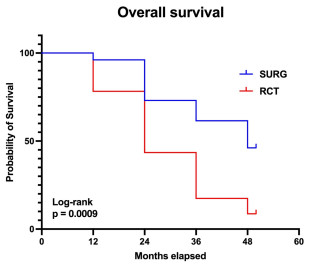
|
||
|
09:40–09:47
Corticosteroids in pancreatic surgery to prevent complications
Katarzyna Czuj, Münsterlingen
AbstractBackgroundMultiple studies have shown a decrease in complications after pancreatic surgery through the perioperative use of corticosteroids. This is in part due to their ability to influence the postoperative systemic response. AimsThe aim of this systematic review was to investigate the impact of perioperative corticosteroids in major pancreatic resections. MethodsA literature search was done in CENTRAL, Medline, and Web of Science. All randomised controlled trials (RCTs) with adult patients undergoing pancreatic surgery and receiving perioperative corticosteroid treatment were included. The outcomes investigated included mortality, complications, postoperative pancreatic fistula (POPF), delayed gastric emptying (DGE), postpancreatectomy hemmorhage (PPH), fluid collection/abscess, and length of hospital stay. Outcomes were analysed as odds ratios (OR) or mean differences (MD) in a random-effects model. ResultsFive RCTs were included. Partial pancreatoduodenectomy as well as distal pancreatectomy were evaluated. There was no difference regarding mortality in 3 RCTs (OR 0,65, 95%-CI: 0.17 to 2,45, p= 0.52). However, complications were lower in the corticosteroids group (OR 0.53, 95%-CI: 0.3 to 0.91, p= 0.02). Specifically, there were fewer fluid collections in the corticosteroids group (OR 0.47, 95%-CI: 0.25 to 0.89, p= 0.2). POPF, DGE, and PPH did not differ between the groups. Furthermore, patients treated with corticosteroids had a shorter length of hospital stay (MD -0.87 days, 95%-CI: -5.23 to -2.51, p= 0.01). ConclusionThe perioperative use of corticosteroids in pancreatic surgery appears to reduce overall complications, particularly fluid collections, and is associated with a shorter length of hospital stay. These findings suggest that corticosteroids may provide a benefit in reducing postoperative morbidity, warranting further investigation into their role in optimising outcomes after major pancreatic resections. |
||
|
09:50–09:57
Rethinking Abdominal Drainage After Distal Pancreatectomy – The PANDRA II Trial
Pascal Probst, Frauenfeld / Heidelberg
AbstractBackgroundProphylactic intraabdominal drainage following distal pancreatectomy (DP) has been a longstanding practice to mitigate postoperative complications, particularly postoperative pancreatic fistulas (POPF). Recent studies challenge the necessity of routine drainage, suggesting potential benefits in omitting drains. AimsThe aim of this trial was to evaluate postoperative complications after DP with or without prophylactic drain placement. MethodsThe PANDRA II trial was a randomized controlled non-inferiority study conducted at a university hospital between 2017 and 2023, comparing outcomes between patients undergoing open or minimally-invasive DP with and without prophylactic abdominal drainage. Primary endpoint was postoperative morbidity assessed by the Comprehensive Complication Index (CCI). ResultsA total of 246 patients were included in the intention-to-treat analysis (125 with drainage, 121 without drainage). The no-drain group demonstrated non-inferiority to the drain group in terms of CCI (13.90 ± 16.51 vs. 19.43 ± 16.92, p<0.001). Moreover, the no-drain group had lower overall complication rates (50.41% vs. 78.40%, p<0.001). Specific complications such as POPF (14.88% vs. 20.8%, p=0.226) and postpancreatectomy hemorrhage (4.96% vs. 4.80%, p>0.999) did not differ significantly between groups. ConclusionThe PANDRA II trial adds to mounting evidence suggesting that routine abdominal drainage may not be necessary following DP. Omitting drains was associated with favorable outcomes in terms of postoperative morbidity, without increasing severe complications requiring intervention. Selective use of drains based on patient risk factors and surgeon expertise is crucial, emphasizing individualized care in pancreatic surgery. |
||
|
08:30 – 10:00
Room 1A
|
SGG - Free Communication 1
Emmanouil Psathas, Fribourg; Lukas Briner, Neuchâtel
|
|
|
Free Communication
|
||
|
08:30–08:38
Prevalence, Phenotypes, and Long-Term Outcomes of Cardiac Complications After Arterial Vascular Surgery
Vanessa Thommen, Basel
AbstractBackgroundVascular surgery patients are at particular high-risk for cardiac complications after surgery. AimsTo determine the incidence and phenotypes of cardiac complications after arterial vascular surgery and to assess long-term mortality and major adverse cardiac events according to different phenotypes of these cardiac complications. MethodsConsecutive high-risk patients undergoing arterial vascular surgery between 2014 and 2019 were included. The incidence of perioperative myocardial infarction/injury (PMI) was determined, and its aetiology was centrally adjudicated by two independent physicians. PMI aetiologies were hierarchically classified into “extra-cardiac” if caused by a primarily extra-cardiac disease such as severe sepsis or pulmonary embolism; and “cardiac”, further subtyped into type 1 myocardial infarction (T1MI), tachyarrhythmia, postoperative acute heart failure (pAHF), or likely type 2 myocardial infarction (lT2MI). All-cause death as well as major adverse cardiac events (MACEs) including acute myocardial infarction, pAHF (both only from day 3 to avoid inclusion bias), life-threatening arrhythmia, and cardiovascular death were assessed during 1-year follow-up. ResultsAmong 2’265 patients (median age 71 years, 73% male), PMI occurred in 423 (18.7%) with the incidence strongly dependent on the type of arterial vascular surgery. 267/2’265 patients died (11.8%) and at least one MACE occurred in 325/2’265 patients (14.3%) within 1 year. Outcomes differed substantially according to aetiology: in patients with extra-cardiac PMI, T1MI, tachyarrhythmia, pAHF, and lT2MI, 67%, 24%, 45%, 47%, and 18% died and 63%, 50%, 73%, 73%, and 20%, patients had MACE within 1 year, respectively, in comparison to 8% and 10% in patients without PMI (Figure 1, Graphical Abstract). ConclusionThe incidence of PMI after arterial vascular surgery is high and related to high rates of mortality and MACE, with extra-cardiac, tachyarrhythmias, and pAHF being associated with worse prognosis. 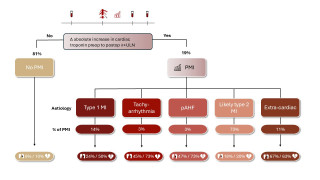
|
||
|
08:43–08:51
"Endovenectomy” of a chronically thrombosed femoral vein for arterial reconstruction in a patient with IV drug use and recurrent bovine pericardial graft infection
Matteo Giardini, Basel
AbstractBackgroundA 53-year-old male with a history of intravenous drug use underwent replacement of the common femoral artery with a bovine pericardial graft due to an infected pseudoaneurysm in 2020. In 2024 he presented with reinfection and bleeding. Part of the graft was replaced, again with a graft from bovine pericardium. The patient was known to have bilateral chronic thrombosis of the femoral and saphenous veins. AimsTo describe the use of a chronically thrombosed femoral vein as an arterial conduit in the treatment of infected bovine pericardial grafts, particularly in a patient with a history of intravenous drug use and chronic vein thrombosis. MethodsIn 2025, following recurrent reinfection and a ruptured pseudoaneurysm, approximately 15 cm of the ipsilateral thrombosed femoral vein was harvested. An “endovenectomy” was performed by eversion of the entire vein segment (Figure 1-3). The vein was anastomosed to the distal external iliac and superficial femoral artery, with the deep femoral artery reintegrated into the vein graft. ResultsA postoperative CT scan demonstrated a regular lumen of the vein graft with a diameter of 8–9 mm. No morbidity related to vein harvesting was observed, as the venous outflow of the leg was unaffected due to the pre-existing thrombosis. ConclusionTo our knowledge this is the first description of the use of a chronically thrombosed femoral vein as an arterial conduit. Our strategy may be the only way to achieve a reconstruction with a fully biological graft, particularly in intravenous drug users with limited venous options due to chronic thrombosis of the femoral and saphenous veins. A further advantage lies in the fact that no morbidity from harvesting the femoral vein is incurred, as the venous outflow of the leg is not affected by resecting a thrombosed vein. The case also highlights the challenge of reinfection in arterial reconstructions involving bovine pericardium and underscores the need for alternative strategies in complex scenarios. Long-term durability remains to be assessed. 


|
||
|
08:56–09:04
Isolated femoral endarterectomy and profundoplasty without revascularization of a femoropopliteal occlusion in patients with chronic limb threatening ischemia
Felix Moehle, Basel
AbstractBackgroundThere is a widely accepted dogma that patients with CLTI and peripheral ulcers need a continuous vascular pathway down to the foot for successful wound healing. Nevertheless, in patients with concomitant common femoral / profunda artery stenosis and femoro-popliteal occlusion it is sometimes decided to leave the femoropopliteal occlusion untreated and only perform profundoplasty +/- iliac artery stenting. AimsThe aim of this study was to evaluate the outcome in these patients. MethodsRetrospective analysis of consecutive patients. ResultsBetween 2014 and 2023 33 limbs in 30 patients with CLTI received femoral endarterectomy, profundoplasty (+/- iliac stenting) without treatment of a femoropopliteal occlusion. The decision not to treat the femoropopliteal occlusion was the lack of an adequate vein for bypass surgery in 5, patient morbidity in 7, small lesion not justifying extensive surgery in 7, very good collateralization from the profunda artery in 3, unsuccessful attempt of femoropopliteal recanalization in 3 and in 9 patient no clear reason for the decision could be discerned. Nearly all patients were in WIfI stage 3. No patient was lost to follow-up. 12 limbs (36%) needed femoropopliteal revascularization because of wound progression (8 bypass surgery, 4 endovascular) and 1 patient (3%) had major amputation. The strategy to not treat the femoro-popliteal occlusion thus failed in 13 (39%) of limbs. In all 20 limbs that did not require femoropopliteal revascularization, complete wound healing was documented. 16 patients (53%) died during follow-up. One year after profundoplasty 4/12 patients with femoro-popliteal revascularization but only 2/18 patients without femoro-popliteal revascularization had died. (Figure 1) ConclusionIn approx. two thirds of our patients with limited wounds the strategy to only perform profundoplasty and leave a femoro-popliteal occlusion untreated was successful. Our data do not allow us to identify risk factors for success or failure of the strategy chosen. The patients who required secondary bypass surgery or endovascular revascularization had a higher mortality. 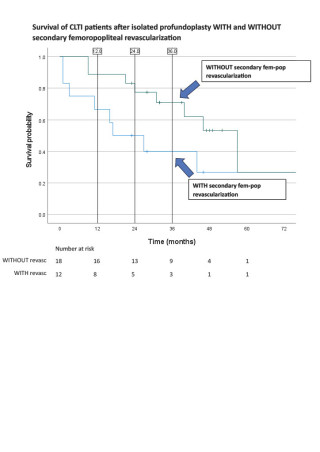
|
||
|
09:09–09:17
Incidence and Risk Factors of Surgical Site Infections in Vascular Surgical Procedures of the Groin
Sarah Steiner, Basel
AbstractBackgroundThe reported incidence of surgical site infections (SSI) in vascular surgery procedures in the groin varies from 8% to a staggering 30%. SSI represent a major burden in postoperative care, cause hospital readmissions and reoperations and generate costs. In the presence of prosthetic grafts, SSI are even more problematic. AimsTo investigate the incidence of SSI following unselected open vascular surgery procedures in the groin in a real-world setting and to explore potential factors associated with SSI MethodsRetrospective analysis of consecutive patients undergoing any arterial surgery in the groin in two teaching hospitals between 2011 and 2022. Primary endpoint is SSI at 30 days for all patients and occurrence of SSI at 90 days for those patients with implants. To identify factors associated with SSI within 30 days, univariable and multivariable logistic regression analyses were performed using prespecified variables. ResultsMean age was 70.7 (11.5) years and 1993 patients (67.1%) were male. While 1094 patients (36.9%) received a patch and 1195 (40.3%) underwent endarterectomy, 1514 (51%) had concomitant bypass surgery. Out of 2967 patients, 180 (6.1%) experienced SSI at 30 days and 27 (0.9%) had SSI at 90 days. On univariable logistic regression, diabetes (OR 1.923, 95%CI 1.411-2.611, p=0.001), patch reconstruction (OR 1.848, 95%CI 1.329-2.56 for bovine pericardial patch and OR 1.915, 95%CI 1.095-3.18 for autologous vein patch p=0.004), endarterectomy (p=0.005) lymphatic complications (OR 3.515, 95%CI 2.385-5.094, p<0.001) were associated with significantly increased odds of experiencing SSI. Duration of surgery (p=0.631) and concomitant bypass surgery (p=0.325) were not associated with the odds of having SSI. On multivariable analysis, only diabetes (OR 1.67, 95%CI 1.18-2.33, p=0.004) and lymphatic complications (OR 3.03, 95%CI 1.98-4.53, p<0.001) remained significantly associated with the odds of having SSI. ConclusionIn this series, the SSI rate was lower than expected and some otherwise accepted risk factors could not be confirmed. |
||
|
09:22–09:30
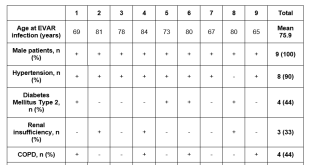
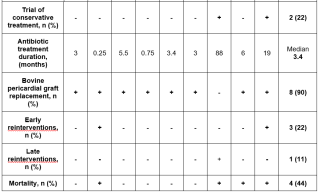
From EVAR to Open Repair: Addressing Endograft Infections in Abdominal Aortic Aneurysm Patients since 20 years
Camilla Schürmann, Bern
AbstractBackgroundEndovascular aortic repair (EVAR) is the preferred treatment for abdominal aortic aneurysms but can lead to rare, life-threatening infections requiring open surgical repair with endograft explantation. Bovine pericardial tube grafts offer an effective solution for in situ reconstruction in aortic infections. We report outcomes of patients undergoing open conversion after EVAR infection. AimsTo present our experience using Bovine pericardial bifurcated grafts to treat infected EVARs. MethodsThis retrospective single-center study from 2004 to 2023 assesses EVAR patients who underwent endograft explantation for infection. Symptoms included fever and pain, with diagnosis confirmed by imaging and microbiology. Endpoints were recurrent infection, reinterventions, graft complications, and mortality. ResultsDuring this period, nine underwent endograft explantation due to infection, of which eight were replaced with bovine pericardial graft and one with silver impregnated graft. Patient demographics are detailed in Table 1. The mean time to infection diagnosis was 15±18 months post-EVAR and follow-up period was 19±32 months, with no cases of recurrent aortic infection observed during this time. Two patients had early reintervention: one for acute limb ischemia caused by occluded graft limb followed by graft thrombectomy and one for relevant bleeding with retroperitoneal hematoma requiring urgent evacuation. Late reinfection occurred in one patient, requiring reintervention 12 years after the initial endograft explantation, originally replaced with a silver impregnated graft. In total four patients died during follow-up, two of them aortic-related. ConclusionThis review highlights the low re-infection rates and minimal complications with physician-made bovine pericardial grafts for EVAR infections. No recurrent infection nor aneurysm ruptures were observed. Long-term follow-up is crucial for early detection and management of these rare but serious infections. Bovine pericardial grafts are an excellent choice for in situ reconstruction. Further research is needed to develop preventive strategies and rapid treatments. 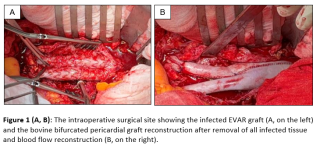
|
||
|
09:35–09:43
Systematic Evaluation on Occupational Staff Health in Interventional Environments with Chronic Low Dose Exposure (SHIELD Study)
Alina Reeg, Lucerne
AbstractBackgroundRadiation exposure for operating room personnel, particularly those performing complex endovascular procedures, has increased considerably over recent years. Those high dose X-ray applications require high resolution imaging quality. The detrimental effects of radiation on a physical and cellular level have been well documented. However, to what extent this translates into clinical manifest disease remains unclear. AimsThis systematic review aims to comprehensively analyze the available literature on radiation induced health implications in endovascular surgery, interventional cardiology, and orthopedic surgery. MethodsMEDLINE (via PubMed) and Embase were searched using keywords, medical subject heading (MeSH)-terms and Entree-terms “occupational health”, “vascular surgery”, “dose” and “radiation” to identify relevant peer-reviewed studies in English published between 2013-2024. For other specialties than vascular surgery, the term was replaced with “cardiology” and “orthopedics”. ResultsIn vascular surgery literature, of 221 screened articles one met the inclusion criteria, demonstrating increased expression of DNA damage and repair markers in surgeons performing endovascular aortic repairs. For interventional cardiology, the search yielded 335 articles, with 9 studies eligible for inclusion addressing lens opacities and DNA damage as documented health outcomes. Regarding orthopedic surgery, 41 studies were screened, with one eligible study elaborating on increased breast cancer risk in female orthopedic surgeons. ConclusionRelevant evidence exists regarding chronic low-dose exposure leading to early cataracts, DNA damages, increased carotid atherosclerosis and increased cancer risk. While radiation-induced lens opacities can potentially occur at relatively low doses, the rate of progression into a vision-impairing cataract is debated. Similarly, potential health impacts of radiation-induced DNA damage have been extensively studied, but clear links to specific adverse health outcomes and quantifiable risk increases are lacking. Considering the increase in endovascular procedures, large-scale cohort studies are necessary to assess clinical endpoints over long period of time. |
||
|
09:48–09:56
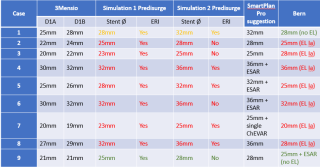
Preoperative simulation with AI-assisted software could identify the risk of postoperative type Ia endoleak after EVAR in hostile neck anatomy
Martin Marxer, Bern
AbstractBackgroundType Ia endoleak (Ia EL) is a major complication of endovascular aortic repair (EVAR), associated with treatment failure and increased risk of late rupture. Hostile neck anatomy significantly elevates the risk of type Ia EL, necessitating meticulous preoperative planning and adjunctive measures such as endoanchors. This study investigates the utility of AI-assisted preoperative simulation for predicting and preventing type Ia EL in patients with hostile neck anatomy undergoing EVAR. AimsAn AI-assisted tool may predict EL1a after EVAR and may be a promising step in preventing early or late preventable complications mostly due to graft size discrepancies. MethodsTen cases treated with Endurant (Medtronic) between 2011 and 2024, with known follow-up outcomes, were analyzed. Preoperative CT scans were sent to Medtronic’s core lab, and two suggested main body sizes were evaluated using AI-assisted simulation software (PlanOP™ Endoleak Risk Index, Predisurge). Both Predisurge and Medtronic were blinded to the implanted main body size and patient outcomes. Simulation predictions were compared to postoperative results. ResultsThe AI-assisted simulation predicted type Ia EL in nine of the ten patients. By June 30, 2024, eight patients developed type Ia EL during follow-up (mean interval 44±36 months), requiring either proximal extension with fenestrated/branched grafts or open surgical conversion. Two patients without type Ia EL had shorter follow-up durations of 6 and 2 months. The simulation demonstrated a sensitivity of 90%. Notably, five main body implantations matched core lab recommendations, while four were undersized, and one patient was excluded due to severe angulation (>60°). ConclusionThe AI-assisted simulation showed high sensitivity and predicted all type Ia EL. In one patient with short follow-up the simulation had false positive prediction, reflecting one of the simulation disadvantages concerning the time frame, in which a type Ia EL could be expected. The AI-assisted software could become an excellent instrument for predicting and preventing type Ia EL after EVAR. 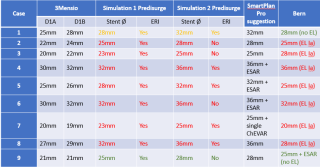
|
||
|
08:30 – 10:00
Room 5A
|
SGT - Free Communication 1
Wolfram Karenovics, Geneva; Zeljko Djakovic, Basel
|
|
|
Free Communication
|
||
|
08:30–08:37
Piloting Lung Cancer Screening: Tumor detection rate, psychological distress and incidental findings
Edoardo Sostero, Zurich
AbstractBackgroundLung cancer constitutes the leading cause of cancer-related deaths in Switzerland. Since 2019, a pilot study evaluating the feasibility and efficacy of low-dose CT lung cancer screening (LCS) program in Switzerland is ongoing. AimsThis analysis summarizes the findings and obstacles of a screening program. Methods307 participants (178 males, median age: 62 years) smokers (200 active) or ex-smokers were included in the lung cancer screening consisting of an interview and a low-dose CT. In a subset of 140 participants (62 females) psychological distress was assessed using a visual analog scale (Range: 0-10). Furthermore, to assess coronary artery calcification (CAC) as incidental finding, the SHEMESH score was utilized. Imaging was scored by two experienced radiologists using a score ranging from 0 to 12. Results11 cancers have been detected (3.58%), 9 lung cancers (2.93%) in stage AIS (1), stage I (3), stage IIIA (3, all incidental N2), stage IV (2), 1 thymoma, 1 thyroid cancer. Most of the participants experienced only minor psychological distress, however some instances of significant stress were reported (Figure 1A). There was a trend for higher reports of psychological distress in females compared to males (p = 0.053). 22.8% participants had a SHEMESH score between 4 and 12 (Figure 1B), of which 28.6% (20 participants) described symptoms potentially indicating CAC. Participants with a SHEMESH scores above 4 were advised to consult a specialist. ConclusionEmploying low-dose CT scans as a screening modality led not only to detection of multiple malignancies; it was also seen that careful consideration of incidental finding and their implication is important within screening programs. Overall, only minimal psychological distress was reported. 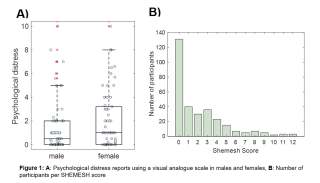
|
||
|
08:40–08:47
Real time imaging of the non-small cell lung cancer immune microenvironment modulation by low dose photodynamic therapy.
Damien Marie, Lausanne
AbstractBackgroundImmune checkpoint inhibitors (ICIs) have significantly improved the outcome of non-small cell lung cancers (NSCLCs). However, cancer response to ICIs occurs in a fraction of patients and correlates with tumor-infiltrating lymphocytes (TILs) presence. Thus, methods to increase TILs within lung cancer are urgently needed. Previously, in a murine model of malignant pleural mesothelioma, we described a mechanism by which low dose photodynamic therapy (L-PDT) enhanced vascular expression of E-selectin, favoring TILs recruitment, and improving tumor control. AimsHere, we hypothesized that a similar mechanism existed in NSCLC and could be further potentiated by ICIs. MethodsWe developed a murine model with a chest window allowing real time imaging by two-photon microscopy of lung adenocarcinoma (LUAD, 344-SQ-GFP, KrasG12D; p53R172HΔG mutant) growing in C57BL/6-CD2-dsRed transgenic mice. We determined the impact of L-PDT±E-selectin blocking antibodies (EBA) on CD2+TILs recruitment over 30 days. In a separate experiment, we assessed the impact of L-PDT±EBA on tumor growth, survival, and spontaneous metastasis development. Finally, we characterized the LUAD immune microenvironment and TILs immune checkpoint expression 1 and 5 days after L-PDT by flow cytometry. ResultsL-PDT significantly enhanced CD2+TILs recruitment, with an increase observed at 1 day that lasted up to 20 days post-treatment compared to controls. L-PDT was significantly associated with improved tumor control (-42%), reduction in metastasis development (-50%) and increased animal survival (+26%) compared to the control group. Interestingly, this phenotype was abrogated to control levels when L-PDT was combined with EAB. Further analysis of the tumor immune microenvironment confirmed the recruitment of CD8+T lymphocytes 1- and 5-days following L-PDT with increased PD-1 expression day 5 post-treatment. ConclusionL-PDT triggers, through vascular E-Selectin, durable infiltration of NSCLCs by TILs which improve tumor control, impair metastasis development, and enhance animal survival. The increased PD-1 levels on CD8-T cells following L-PDT suggest a favorable combination with PD1/PDL1 inhibitors. |
||
|
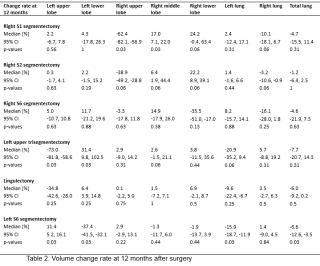
08:50–08:57
Post-Operative Volume Changes in Residual Lung Lobes After Thoracoscopic Segmentectomy for Early Stage Non-Small Cell Lung Cancer
Antoine Dewarrat, Lausanne
AbstractBackgroundPulmonary segmentectomy is a valid alternative to lobectomy in early-stage non-small cell lung cancer (NSCLC), however little is known about post-operative compensatory volume changes. AimsWe aim to investigate overall trends in volume changes of residual lung lobes over time after segmentectomy. MethodsWe retrospectively reviewed patients who underwent pulmonary segmentectomy for early-stage NSCLC in our institution from 2017 to 2022. Pre-operative lung lobe volumes were computed from 3D lung models (Materialize®) and compared to residual lung lobes at 6 and 12 months post-operatively. ResultsThirty patients (median age: 66 (62-73), sex ratio M/F: 14/16) underwent VATS segmentectomy with systematic lymphadenectomy (Table 1). On the right side, median loss of volume of lobes was -62.4% (p-value = 0.03) for S1 segmentectomy (n=6), -38.9% (p-value > 0.05) for S2 (n=5) and -35.5% (p-value > 0.05) for S6 (n=4) at 12 months. Compensatory expansion was predominant in lower lobes for upper segmentectomy, respectively +24.2% (p-value > 0.05) for S1 and +22.2% (p-value > 0.05) for S2, whereas compensation in middle lobe was present for S1 segmentectomy (+17%, p-value = 0.03) and for S6 (+14.9%, p-value > 0.05). For the left side, median loss of volume was -73.0% (p-value = 0.03) after upper trisegmentectomy (n=6), -34.8% (p-value > 0.05) after lingulectomy (n=3) and -37.4% (p-value = 0.03) after S6 segmentectomies (n=6). Compensatory expansion was predominant in lower lobes for upper left segmentectomies (+31.4%, p-value = 0.03), whereas compensation of median upper lobe volume was +11.4% (p-value = 0.03) for lower left segmentectomy at 12 months. Median total lung volume was not significantly different for among type of segmentectomies at 12 months, except for left S6 (-6.6%, p-value = 0.03) (Table 2). ConclusionVolume compensation mechanism occurs after segmentectomy. Reduction in volume may be more affected during upper lobe segmentectomy compared to lower lobe segmentectomy. 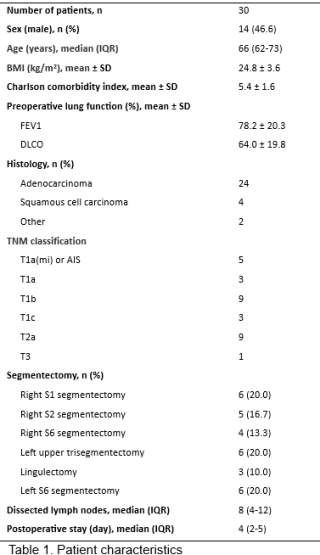
|
||
|
09:00–09:07
Lung volume reduction surgery reduces pulmonary hypertension in selected patients with emphysema
Bianca Battilana, Zurich
AbstractBackgroundLung volume reduction surgery (LVRS) provides benefit in survival, lung function, gas exchange and quality of life in patients with emphysema. Pulmonary hypertension (PH) is a late and serious complication in patients suffering from emphysema. Given the high-risk profile, LVRS remains controversial in this patient subgroup. AimsWe aim to present our institutional experience in performing LVRS in emphysema patients with PH. MethodsData was retrospectively collected from October 2002 until September 2024. We included patients with pre-and postoperative transthoracic echocardiogram (TTE) and/or right heart catheterization (RHC). We defined pulmonary hypertension (PH) as sPAP >35mmHg (TTE), mPAP ≥20mmHg (RHC) or other signs of pulmonary hypertension in TTE. We compared pre-and postoperative sPAP and forced expiratory volume in 1 second (FEV1) and analyzed the outcome. Results158 patients with COPD and PH underwent LVRS from October 2002–September 2024. Our cohort consists of 68 (43%) female patients with a median age of 67 [IQR 62-73]. 50 (32%) patients had homogeneous, 104 (66%) heterogeneous and 4 (2%) intermediately heterogeneous patterns of emphysema. 72 (46%) patients had an estimated sPAP >35mmHg in the preoperative TTE, 46 (29%) patients presented with mPAP ≥20mmHg during RHC, 40 (25%) patients showed signs of PH in the TTE. The sPAP (TTE) decreased significantly from 43.5mmHg [IQR 39-50] preoperatively to 39.5mmHg [IQR 35-44.25, p=0.0138] postoperatively, independent of emphysema type. These patients also had an improvement in FEV1 from 710ml [IQR 560-860ml] preoperatively to 845ml [IQR 687.5-1160ml, p<0.0001] postoperatively. The 30-day mortality was 2 (1%), and the median overall survival was 37.44 months [IQR 17.49-64.89]. ConclusionLVRS can lead to significant reduction of PH and improvement in lung function for patients with all emphysema types. Therefore, PH should not be an exclusion criterion per se and patients being equally assessed in a specialized institution. 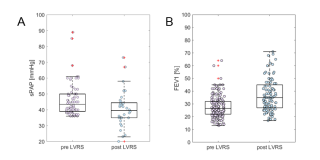
|
||
|
09:10–09:17
The Value of PET-CT in Predicting the Response of Stage III N2 Non-Small Cell Lung Cancer Managed by Neoadjuvant Chemo-Immunotherapy.
Louis-Emmanuel Chriqui, Lausanne
AbstractBackgroundNeoadjuvant chemo-immunotherapy has become a standard for management of resectable stage III non-small cell lung cancer (NSCLC) patients with improved overall survival. Post-induction radiological re-staging, commonly performed with CT scan, is crucial in surgical planning. AimsThis study evaluates the predictive value of PET-CT scan after neo-adjuvant chemo-immunotherapy to predict tumor response and patient survival. MethodsWe analyzed, in our prospectively collected database, 68 resectables stage III N2 NSCLC patients treated by neoadjuvant chemo-immunotherapy followed by surgery between 2017 and 2023. Forty patients underwent PET-CT both pre- and post-induction. Surgical resections, histopathological assessments and survival follow-up, were recorded. We measured changes (ΔSUV) in mean and maximum SUV of tumors and tumor involved lymph nodes before and after induction therapy. We computed ΔSUV related to pathological response and survival using receiver operating characteristic and Kaplan-Meier analysis respectively. ResultsOver 40 patients, 23 were women and 17 men. Mean patient age was 63.5±8.0 years. Surgeries consisted in lobectomy (88%), bilobectomy (10%) and segmentectomy (2%). 38% were minimal invasive approaches. R0 and R1 resection occurred in 93% and 7% (lymph node capsular effraction) patients respectively. Complete pathological response (pCR) occurred in 27% patients. Mean and max tumor ΔSUV predicted pCR (Mean: AUC=0.8013, p=0.004; Max: AUC=0.7980, p=0.004 Fig 1A). ΔSUV of lymph nodes provided stronger predictive value (Mean: AUC=0.9028, p=0.006; Max: AUC=0.8848, p=0.006, Fig 1B). Statistical analysis of tumor and node ΔSUV showed that a mean lymph node ΔSUV of -70% was the best predictor of pCR with a sensitivity of 88.89% and a specificity of 87.50% (Fig 1B). This -70% in mean lymph node ΔSUV change correlated with overall survival in our cohort (Fig 1C). ConclusionMean ΔSUV of lymph nodes on PET-CT between pre and post chemo-immunotherapy of stage III N2 NSCLC predicts pCR and overall survival with good sensitivity and specificity. 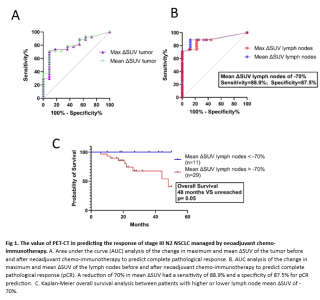
|
||
|
09:20–09:27
Repeated Anatomical Pulmonary Resection for Second Primary Non-Small Cell Lung Cancer: Safety, Feasibility and Short-Term Outcomes
Céline Forster, Sion
AbstractBackgroundAdvances in non-small cell lung cancer (NSCLC) management have extended survival rates, contributing to a higher incidence of second primary NSCLC (2-20%). Repeated anatomical pulmonary resection in these cases poses significant technical challenges and functional limitations due to previous surgery. AimsThis study evaluates the feasibility and short-term outcomes of repeated anatomical pulmonary resections for second primary NSCLC. MethodsWe retrospectively reviewed all consecutive cases of repeated anatomical pulmonary resections for second primary NSCLC performed in our institution from January 2014 to December 2023. Clinical-pathological characteristics, postoperative complications, and oncological outcomes were analyzed. ResultsA total of 55 patients (median age 68 years [IQR: 61.5-72]) underwent repeated anatomical pulmonary resections for second primary NSCLC (figure 1). Adenocarcinoma predominated in both primary (78.2%) and secondary (76.4%) cases. Video-Assisted Thoracoscopy (VATS) approach was used in 94.5% and 96.4% after first and repeated resection, respectively (p=0.647). The extent of pulmonary resection differed between first and second resection, with a predominance of lobectomy during first resection (56.4%) and segmentectomy during second resection (85.5%, p<0.001). We did not observe any significant difference in postoperative overall morbidity after first and second resection (23.6% vs. 40%, p=0.065). However, there was a significant increased incidence of cardiac complications (16.4% vs. 0%, p=0.007) and prolonged air leak (>5 days) after second resection (14.5% vs. 0%, p=0.014). The median length of hospital stay was similar after first and repeated resection (5 vs. 5 days, p=0.089) and the duration of chest drainage was marginally increased after the second surgery (2 vs. 1 day, p=0.065). Three-year overall survival after primary resection was 89%. Recurrence was documented in one patient (1.8%) after first resection and two patients (3.6%) after second resection (p=0.558). ConclusionOur series demonstrated that second primary NSCLC can be safely managed by VATS segmentectomy, yielding favorable short-term survival and low recurrence rate. 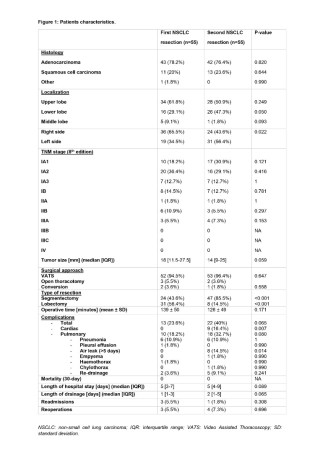
|
||
|
09:30–09:37
Salvage Surgery after Nonoperative Treatment of initially UnresectableStage IIIB-IV Non-Small Cell Lung Cancer
Raphael S. Werner, Zurich
AbstractBackgroundDespite the current advancements in systemic treatment, cancer persistence, progression or recurrence remain common after nonoperative treatment of unresectable non-small cell lung cancer (NSCLC). In this situation, lung resection frequently remains among the last options to achieve local cancer control. AimsWe aimed to assess the outcomes of salvage lung resection in patients with stage IIIB-IV NSCLC. MethodsPatients with stage IIIB-IV NSCLC who underwent anatomical lung resection between 2003 and 2024 after initial nonoperative treatment were identified from a prospectively maintained database. Results42 patients were included in the analysis. Median age was 61.5 (IQR 51.8 – 67.5) years and 57.1% were male. The cohort included 9 UICC stage IIIB/C patients and 33 stage IV patients. Nonoperative treatment included definitive chemoradiotherapy in 19 cases (45.2%), immuno- or chemoimmunotherapy in 21 cases (50%) and targeted therapy in 10 cases (23.8%). The indication for lung resection was local recurrence in 4 (9.5%) patients, (oligo) progression under active treatment in 9 (21.4%) patients and (oligo)persistence under active treatment in 29 (69%) patients. Resections included 1 segmentectomy, 14 standard lobectomies, 15 extended lobectomies, 2 bilobectomies and 10 (extended) pneumonectomies. 66.7% (n=28) of all resections were performed by thoracotomy, 16.7% (n=7) by VATS and 16.7% (n=7) by RATS. Median overall survival was 27.0 months (IQR 11.0-69.5 months). R0-resection was achieved in 88.1% of all cases. Overall survival was significantly improved if R0-resection was achieved (median OS 71.0 [40.0-131.0] months versus 11.0 [10.0-14.0] months, p<0.001). ConclusionSalvage surgery remains a valuable option for patients with advanced NSCLC and cancer persistence, progression or recurrence after initial nonoperative treatment and can provide a substantially prolonged long-term survival. In this heavily pretreated population, extended resections with high surgical complexity are common. The achievement of R0-resection is essential as further treatment options are often not available. 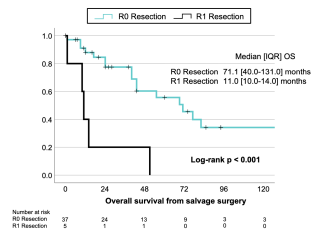
|
||
|
09:40–09:47
Return to Intended Oncologic Treatment (RIOT) After Surgical Resection of Oligometastatic Non-Small Cell Lung Cancer.
Raphael S. Werner, Zurich
AbstractBackgroundIn oligometastatic Non-Small Cell Lung Cancer (NSCLC) combining systemic and local ablative treatments, including lung resection or radiotherapy, has been shown to improve survival. Maintaining continuity in systemic therapy is crucial in metastatic disease, making the time to Return to Intended Oncologic Treatment (RIOT) after surgery a promising oncologic outcome parameter, which has not yet been investigated in oligometastatic NSCLC. AimsWe aimed to assess whether an early RIOT after anatomical lung resection is associated with improved survival. MethodsWe retrospectively analyzed patients with synchronous oligometastatic NSCLC (≤5 metastases in ≤3 organs) diagnosed between 2004 and 2024 who underwent anatomical resection of the primary tumor and were planned for adjuvant oncologic treatment. RIOT was defined as the interval between surgery and the first dose of adjuvant treatment. Predictors of overall survival (OS) and recurrence-free survival (RFS) were assessed by multivariate Cox regression. ResultsThirty-six patients were analyzed; 58% were female and the median age was 60.0 [53.0–67.0] years. Despite stage IV disease, 61% of lung resections were performed minimally invasive (42% VATS, 19% RATS). Median RIOT was 36.0 [27.0–56.3] days and ROC analysis identified 41.5 days as the cut-off to discriminate recurrence. Patients returning to oncologic treatment within 42 days had significantly improved RFS compared to those with delayed RIOT (44.0 [18.0–101.0] vs. 14.0 [5.0–31.0] months, p=0.012) (Figure 1). In the multivariate Cox regression model, RIOT was identified as an independent predictor of RFS (HR 2.55, 95% CI 1.04–6.27, p=0.042). ConclusionRIOT appears to be a valuable predictor for RFS in patients with synchronous oligometastatic NSCLC who undergo anatomical lung resection as part of the multimodality treatment approach. These findings emphasize the importance of minimally invasive surgery and the implementation of enhanced recovery after thoracic surgery (ERATS) protocols to facilitate a timely RIOT in this patient population. 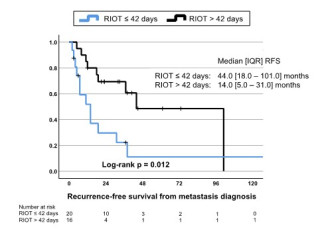
|
||
|
09:50–09:57
Complex Chest Wall Defect Coverage – Challenge for Thoracic and Plastic Surgery- A Case Presentation
Jovan Vujic, Basel
AbstractBackgroundSuccessful thoracic wall reconstruction aims to restore interior thoracic integrity, maintain and protect pulmonary mechanics, and reduce deformities. Muscle flaps are used to cover defects and promote healing. However, issues like seroma formation and muscle atrophy remain. A multidisciplinary approach is sometimes crucial for effective management. We present a very complex case of a 67-year-old female patient and the extensive treatment that the patient received; an example of the importance of interdisciplinary surgical collaboration.
Case presentationA 67-year-old female patient with neuroendocrine carcinoma underwent a complex treatment course involving oncological, infectious, and challenging anatomical complications. The patient developed empyema and bronchus stump insufficiency multiple times, leading to multiple stump revisions and thoracotomies. Thoracic wall reconstruction was performed several times with multiple coverage materials: pericardial patch, Gore-Tex Mesh, left latissimus dorsi muscle, VRAM-Plastic (vertical rectus abdominis musculocutaneous flap). Also, left latissimus dorsi muscle, omentum majus flap, left pectoralis major muscle were used for stump coverage. The patient also had an ipsilateral lymph node tumor recurrence and lastly chemo-radio therapy. The patient had concomitant comorbidities: malnutrition, polymicrobial empyema, neoadjuvant chemotherapy, radio-chemotherapy for tumor recurrence and multiple ischemic cerebral insults. Despite many surgeries, muscle flaps were successfully strategically used to close the thoracic wall, especially in presence of intrathoracic infection. Patient survived to date four months after surgery. We utilized several muscle flaps for thoracic wall closure and, with intrathoracic infection aside, they presented by each revision as viable and preserved. Cross-disciplinary cooperation resulted in successful salvage of the patient. ConclusionAn interdisciplinary collaboration requires joint planning and execution. This ensures correct function and healing, leading to improved patient satisfaction and recovery in the challenges of thoracic wall reconstruction with soft tissues. 
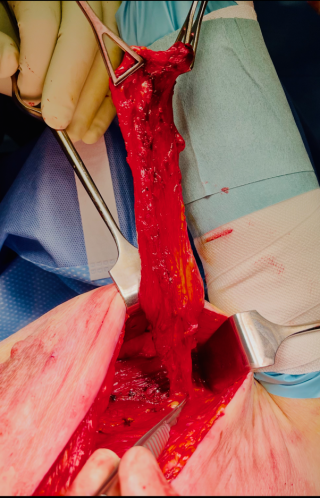

|
||
|
08:30 – 10:00
Room 4BC
|
Update Thorax trauma
Frank J.P. Beeres, Lucerne; Fabrizio Minervini, Lucerne
|
|
|
Main Session
|
||
|
08:30–08:45
Flail chest: when to fix, how to fix?
Fabrizio Minervini, Lucerne
|
||
|
08:45–09:00
Multiple rib fractures: what to do?
Bryan van de Wall, Lucerne
|
||
|
09:00–09:15
Thoracoscopy: when is it indicated?
Aljaz Hojski, Basel
|
||
|
09:15–09:30
Drain management up to date
Michel Gonzalez, Lausanne
|
||
|
09:30–09:45
Does the shoulder girdle influence the thoracic cage?
Christian Michelitsch, Chur
|
||
|
10:00 – 10:30
|
Coffee Break |
|
|
Break
|
||
|
10:30 – 12:00
Room 5C
|
ARS Innovations in surgery : Pigs, Robots or humans?
Deborah Stroka, Bern; Leo Buhler, Fribourg
|
|
|
Main Session
|
||
|
10:30–10:50
Innovations in the management of Inflammatory Bowel Disease
Michel Adamina, Fribourg
|
||
|
10:50–11:10
Xenotransplantation - State of the Art and Lessons for Future Clinical Trials
Raphael Meier, Baltimore US
|
||
|
11:10–11:30
Strategies to increase access to kidney transplantation
Alban Longchamp, Boston US
|
||
|
11:30–11:50
Robotic surgery for colorectal cancer : the new gold standard?
Jeremy Meyer, Geneva
|
||
|
10:30 – 12:00
Room 4BC
|
Geriatric Ankle Fractures
Steffen W. Pfarr, Schwyz; Christoph Meier, Winterthur
|
|
|
Main Session
|
||
|
10:30–10:50
Why are geriatric ankle fractures different and how does it affect the treatments strategies?
David Fässler, Winterthur
|
||
|
10:55–11:15
The fibula: plating vs. nailing
Lizzy Weigelt, Lucerne
|
||
|
11:20–11:40
The tibia: posterior malleolus and (postero-)medial malleolus: how and when to fix it in geriatric ankle?
Primoz Potocnik, Chur
|
||
|
11:45–12:05
Primary arthrodesis: indications, options and techniques
Melanie Leimbacher, Zurich
|
||
|
10:30 – 12:00
Room 1A
|
Guardians of the Scalpel: Securing excellence in complex aortic disease treatment
Drosos Kotelis, Bern; Thomas Wyss, Winterthur
|
|
|
Guardians of the Scalpel
|
||
|
10:30–10:40
Open surgeryAortic trauma : is there still a place for open surgery ?
Nicolas Murith, Geneva
|
||
|
10:40–10:50
Open SurgeryHow to teach open surgery for aortic graft infection?
Thomas Wolff, Basel
|
||
|
10:50–11:00
Open SurgeryDiscussion |
||
|
11:00–11:10
EndovascularUpdate in the treatment of acute uncomplicated aortic type B dissection?
Maani Hakimi, Luzern
|
||
|
11:10–11:20
EndovascularManagement of LSA in thoracic aortic disease
Benedikt Reutersberg, Zürich
|
||
|
11:20–11:30
EndovascularDiscussion |
||
|
11:30–11:37
Debate: Complex AAA treatment in emergency in stable situationsFor open surgery
Alessandro Robaldo, Lugano
|
||
|
11:37–11:44
Debate: Complex AAA treatment in emergency in stable situationsFor PMEG
Vladimir Makaloski, Bern
|
||
|
11:44–11:51
Debate: Complex AAA treatment in emergency in stable situationsFor Off-the-shelf device
Sébastien Déglise, Lausanne
|
||
|
11:51–12:00
Debate: Complex AAA treatment in emergency in stable situationsDiscussion |
||
|
10:30 – 12:00
Room 5A
|
Guardians of the Scalpel: Securing Excellence in the Treatment of Stage III Non Small Cell Lung Cancer - Main Session 1
Thorsten Krueger, Lausanne; Peter Kestenholz, Lucerne
|
|
|
Guardians of the Scalpel
|
||
|
10:30–10:50
Surgery plays a key role in the treatment of stage III non-small cell lung cancer
Jonathan D. Spicer, Montréal CA
|
||
|
10:50–11:10
The role of Radiotherapy in stage III NSCLC: shifting paradigms
Sara Ramella, Rome IT
|
||
|
11:25–11:45
Completeness of Resection: From Visualization to Navigation
Philipp Feodorovici, Bonn DE
|
||
|
10:30 – 12:00
Room 4A
|
HPB & Transplant
Christian Toso, Geneva; Vanessa Banz, Bern
|
|
|
Free Communication
|
||
|
10:30–10:37
Obesity Hinders Access to Kidney Transplantation in Patients on Chronic Kidney Replacement Therapy - A Swiss National Registry-Based Study Between 2010-2024
Maurus Steigmeier, Zurich/Muri / Zurich / Muri
AbstractBackgroundThe global rise in obesity has a major impact on patients with end-stage renal disease (ESRD). Kidney transplantation (KT) is the best available treatment for ESRD, offering superior survival and quality of life compared to chronic dialysis. Obesity is not an absolute contraindication to KT, however its impact on access to KT in Switzerland has not been investigated so far. AimsThe aim of this study was to assess the impact of BMI on mortality and on the chances of receiving KT in patients with ESRD in Switzerland. The overarching goal was to provide real-world data to guide clinical decision-making in patients with concomitant obesity and ESRD, and to explore the eventual need for optimization of the existing care pathways for this patient subgroup. MethodsWe performed a retrospective national registry-based study including all patients on chronic dialysis, who were captured in the mandatory prospective Swiss Renal Registry and Quality Assessment Program and started dialysis between 01/2010 and 12/2020, with last follow-up until 12/2023. After a stepwise exclusion of cases with contraindications to metabolic bariatric surgery (MBS) and/or to KT, we compared demographic data, mortality, and rate of KT between patients with BMI< vs. ≥30 kg/m2. Results2777 patients were identified, among whom n=730 had BMI≥30 (median BMI between the subgroups: 24.1 kg/m2 vs. 34.9 kg/m2). All-cause mortality was higher in patients with obesity (30.0% vs. 25.9%; p=0.038) and their rate of KT was also significantly lower (38.4% vs. 49.0%; p<0.001; OR 0.65). ConclusionObesity was found to be associated with higher mortality rate and decreased chances for accessing KT in patients on chronic dialysis. Consequently, in potential KT candidates with obesity, current standards of care could be enhanced with the broader implementation of robotically assisted KT and/or with the consideration of referral to MBS in the course of ESRD. 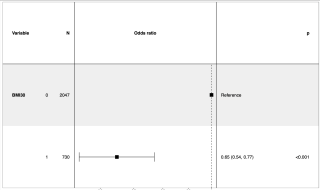
|
||
|
10:40–10:47
Five Decades of Pancreas Transplantation at the University Hospital of Zurich – A Story of Continuous Improvement and Success
Michael Frey, Zurich
AbstractBackgroundPancreas transplantation (PT) is the treatment of choice for patients presenting with type I diabetes and end stage kidney disease. The history of PT at the University Hospital of Zurich (USZ) started in 1973 with the first PT ever performed in Europe. AimsTo describe the evolution of PT at the USZ from 1973 to 2023, and to analyze differences in patient and graft survival within different eras of surgical technique. MethodsWe retrospectively analyzed all PTs performed at the USZ between 1973 and 2023. Due to the evolution in surgical techniques, we divided all PT into 5 different eras: The initial Experience with PT (era 1, n=4), Experimental Duct Management (era 2, n=13) with open or ligated pancreas duct, External/Transcutaneous Duct Drainage (era 3, n=56), Bladder Drainage (era 4, n=41) and Enteric Drainage (era 5, n=166). ResultsOverall, 280 primary PT were performed at the University Hospital Zürich. Between era 1 and 5 CCI at discharge and 90 days decreased from 100 and 100, to 20.9 and 33.6 (p<0.001), respectively. Overall survival at 1-, 5-, and 10- years improved from 73.5%, 51%, 44.9% in era 3, to 69.7%, 60.6%, 51.5% in era 4, and 95.8%, 95.4%, 82.1% in era 5, respectively (p<0.001). Insulin-free survival after 1-, 5-, and 10- years was 34.5%, 25.5%, 16.4% in era 3, 41.5%, 34.1%, 31.7% in era 4, and reached 85.5%, 78%, 64.5% in era 5 (p<0.001), respectively. ConclusionDuring the last five decades, enhanced surgical techniques and improvements in immunosuppression helped to overcome many obstacles that hampered the early days of PT. Initial results were in stark contrast to the excellent results achieved within the current era. With significantly fewer complications, patient- and graft survival improved remarkably over time, evolving PT into a safe and highly efficient procedure. 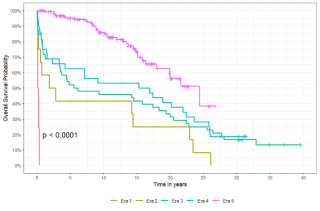
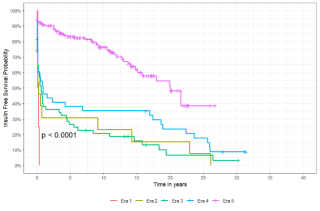
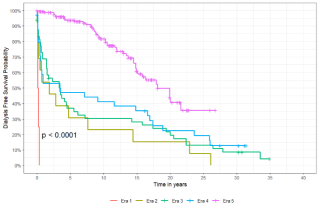
|
||
|
10:50–10:57
Robotic-assisted Laparoscopic Kidney Transplantation
Lorenzo Viggiani D'avalos, Bern / Zurich
AbstractBackgroundRobotic-assisted laparoscopic kidney transplantation has emerged as an innovative surgical procedure in the field of transplantation and is nowadays routinely performed in our institution. It offers various benefits, mainly in terms of reduced wound complications in obese recipients. AimsThe goal of our video was to present the key steps of this technique in a clear, instructive, and illustrative way, making it accessible to surgeons at all levels of training in the field of kidney transplantation. MethodsWe produced an educational video that highlights each step of this procedure, from positioning the patient, to vascular preparation of the iliac axis and anastomotic techniques. We use the da Vinci Surgical System (Intuitive Surgical®, Mountain View, CA). ResultsThis video clearly and comprehensively demonstrates each step of the robotic-assisted laparoscopic kidney transplantation. It provides a concise overview of patient and da Vinci positioning, trocar placement, surgical preparation, and anatomical landmarks associated with each step. ConclusionRobotic-assisted laparoscopic kidney transplantation is safe and feasible. It can facilitate surgical access, vascular preparation and anastomotic sutures in obese patients. This educational video can greatly assist in learning and understanding the various steps of this procedure. This video emphasizes the value of the robotic technique in kidney transplantation. |
||
|
11:00–11:07
Machine Perfusion in Deceased Donor Kidney Transplantation: A Multi-National Analysis of Long-Term Outcomes
Fabian Kalt, Zurich / Baden
AbstractBackgroundMachine perfusion (MP) is increasingly utilized for organ preservation in kidney transplantation, particularly for donation after circulatory death (DCD) donors. AimsThis study investigates the impact of MP on long-term graft and patient survival compared to static cold storage (SCS) using a large multi-national dataset. MethodsThis retrospective cohort study analyzes patient-level data from three national registries: Swiss Cohort Study, the United Network for Organ Sharing (UNOS), and the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA), encompassing over 500,000 kidney transplant recipients. The primary endpoint is 5-year graft survival. Secondary endpoints include delayed graft function (DGF). Three groups are compared: DCD kidneys preserved with MP, DCD kidneys preserved with SCS, and kidneys from donation after brain death (DBD) donors. ResultsPreliminary analysis of UNOS data demonstrates no significant difference in 5-year graft survival between DCD kidneys preserved with MP (median graft survival of 9.4 years) and SCS (median graft survival of 8.9 years), p=0.5. Importantly, 5-year graft survival in DCD kidneys preserved with SCS was comparable to that observed in DBD kidney transplants. However, MP was associated with a lower incidence of DGF (40%) compared to SCS (45%), p<0.01. ConclusionIn this large multi-national study, MP reduced the rate of DGF in DCD kidney transplantation but did not confer a long-term benefit in terms of graft survival. |
||
|
11:10–11:17
Nephrectomy in Future Renal Transplant Patients with Autosomal Dominant Polycystic Kidney Disease
Nadia Atitallah, Lausanne
AbstractBackgroundAutosomal Dominant Polycystic Kidney Disease (ADPKD) is a major hereditary cause of end-stage renal disease (ESRD). Native kidneys in ADPKD patients often cause complications like chronic pain, infections, or hemorrhagic cysts due to their large size. Nephrectomy is frequently required, but the timing (pre-, peri-, or post-transplantation) and approach (unilateral or bilateral) remain debated, with significant variability among transplant centers complicating strategies. AimsThis study evaluates the indications, complications, and outcomes of nephrectomy (bilateral vs. unilateral) in ADPKD patients undergoing kidney transplantation, aiming to develop a decision tree to standardize practices. MethodsA retrospective analysis was conducted on 110 ADPKD patients transplanted between 1999 and 2021 at one center, with 77 undergoing nephrectomy (84% bilateral, 12% unilateral). Indications included space constraints, chronic pain, infections, and hemorrhagic cysts. Complications such as transfusions, hernias, and infections were analyzed. Histopathological findings from 119 resected kidneys were examined. Questionnaires were sent to national centers to compare nephrectomy practices and timing. Data from recent European literature complemented the analysis. ResultsAt the study center, bilateral nephrectomy, performed pre-transplant in 84% of cases, was mainly indicated for space constraints (64%), chronic pain (49%), and infections (47%). It resulted in fewer complications, such as infections (7%) and hernias (16%), than unilateral approaches. Questionnaires showed other centers favor unilateral nephrectomy, mainly pre-transplant but occasionally post-transplant, depending on local protocols and patient cases. European literature supports this trend, highlighting flexible timing based on practice. Histological findings showed serous cysts (84%), fibrosis (55%), hemorrhagic cysts (67%), and tumors (2%). ConclusionThis study highlights the benefits of bilateral nephrectomy in reducing complications and improving outcomes. Addressing gaps in comparative evaluations, it provides actionable insights for transplant centers. A standardized decision-making framework could harmonize practices, reduce variability, and enhance care. |
||
|
11:20–11:27
Robotic-Assisted Laparoscopic Nephrectomy and Autologous Kidney Transplantation – A Step by Step Video Guide
Franca Bergfelder, Zurich
AbstractBackgroundRobotic-assisted kidney transplantation (KT) and -live-donor nephrectomy are routinely performed and offer various benefits, mainly regarding wound complications in obese patients. A combination of both surgeries can be performed using the same incisions. We present a case of a 57-year-old female patient, where laparoscopic hysterectomy with lymphadenectomy for ovarian carcinoma resulted in a long-segment injury to the left ureter, leaving about 2 cm of proximal ureter. Initial treatment was with nephrostomy, complicated by recurrent infections and resulting in an overall reduced kidney function. Scintigraphy showed that the left kidney still provided about 50% of total function. Ureter reconstruction techniques using the bladder or intestinal interposition was deemed unfeasible. Consequently, the decision was made to proceed with ipsilateral autologous KT to achieve uretero-cystostomy. AimsAim of this video is to provide a step-by-step instruction for robotic-assisted laparoscopic left nephrectomy and subsequent autologous KT into the ipsilateral fossa iliaca, This technique is a viable alternative to ureteral reconstruction techniques for large substance defects following ureteral lesions, offering the advantages of MIS. MethodsSurgery was performed at the Department of Surgery and Transplantation at the USZ in 2024.Nephrectomy and transplantation were performed robotic-assisted via transabdominal approach. ResultsThis video provides detailed instructions for each step of the surgery, together with written descriptions of the procedure. The first part shows the left-sided nephrectomy, the second part the vascular preparation of the left iliac axis and the subsequent auto-transplantation. The last part shows the modified implantation of the short ureter stump into the bladder. ConclusionThis high-quality video provides a step-by-step guide to robotic-assisted laparoscopic autologous nephrectomy and KT, highlighting the critical steps. This video is aimed at transplant surgeons who are interested in the latest developments in robotic-assisted surgery in transplantation and would like to implement these techniques into clinical routine. |
||
|
11:30–11:37
Integrating machine learning and mathematical modeling to predict hepatocellular carcinoma recurrence and optimize outcomes after liver transplantation
Daniel Sanchez-Taltavull, Bern
AbstractBackgroundCancer recurrence remains the leading cause of death following liver transplantation (LT) for hepatocellular carcinoma (HCC). Although various models have been developed to predict recurrence, the application of machine learning and advanced mathematical modelling in this area is still limited. AimsWe therefore aimed to develop a machine learning derived model to predict HCC recurrence after transplantation and show its potential to maximize patient survival. MethodsWe developed several machine learning classifiers using clinical data from the Swiss Transplant Cohort Study (STCS) of patients transplanted for HCC (n = 505) to predict recurrence. To estimate the clinical impact of our model, we integrated this classifier with a mechanistic mathematical model to optimize survival outcomes. Integrating the classifier into a Monte Carlo simulation approach, we evaluated personalized treatment strategies, quantifying their potential to enhance long-term survival. ResultsThe overall HCC recurrence rate after HCC transplantation in the STCS cohort was 14%, the median time to recurrence was 22 months, the mean follow-up time was 42.7 months. The dataset was used to train different machine learning classifiers and Random Forest showed the best performance in predicting HCC recurrence. The following variables were identified to be associated with recurrence: Alpha-Fetoprotein (AFP) before LT, ALAT before LT, Cold Ischemia time, ALBI score before LT, Bilirubin before LT, Donor Age, MELD score, Albumin before LT and Vascular Invasion. Finally, the Monte Carlo simulations suggest that the predictive information from the Random Forest could optimize existing liver transplantation protocols, therefore improving overall survival outcomes. ConclusionOur results demonstrate that combining predictive analytics with mechanistic modeling enables a data-driven, individualized HCC recurrence risk prediction. While this approach underscores the potential of advanced modeling techniques to improve patient prognosis in liver transplant oncology, future work involves validating the model in additional datasets. |
||
|
11:40–11:47
Metabolic Duties Govern the Regenerative Competencies of the Growing Liver
Dominique Lisa Birrer, Zurich
AbstractBackgroundThe liver has remarkable but limited regenerative abilities. Metabolic duties may play a crucial role in defining the proliferative behaviour of hepatocytes. During regeneration, metabolic activity and cell proliferation are spatially separated, suggesting that metabolic functions may constrain space for growth. AimsWe used mouse models of the two-stage hepatectomy ALPPS (surgery known for its rapid regeneration) to investigate whether metabolic demands influence the regenerative potential of the growing remnant. MethodsMice were subjected to either sham or ALPPS surgery, resulting in a fast-regenerating future liver remnant (FLR) paired with portally ligated lobes (LLs), which do not grow but retain intact arterial supply. Regenerative activity, metabolic function, and their interplay were evaluated using proliferative parameters and Omics analyses combined with functional surgery approaches. Liver samples from patients undergoing ALPPS surgery were analysed to validate our findings. ResultsMetabolomic profiling of the FLR and adjacent LLs revealed similar metabolite signatures, which however completely diverged during the FLR’s rapid growth phase. Combined transcriptomics-metabolomics analyses underscored a confinement of proliferation to the FLR, while LLs were enriched in metabolic functions as confirmed on histology. In functional ALPPS variants with different ligated volumes, FLR growth strictly correlated with the amount of ligated volume, revealing the dependency of regeneration on metabolic function. Notably, FLRs of slow-growing variants exhibited upregulated metabolic processes, suggesting an adaptive response to increased metabolic demand with smaller ligated volumes. Transcriptomics demonstrated similar functional partitioning in human ALPPS regeneration. ConclusionIn ALPPS, LLs function as metabolic support structures, allowing the FLR to concentrate on regeneration. Our findings demonstrate the need for 'division of labour' and highlight the importance of functional specialization during liver regeneration, where metabolic needs are critical in shaping the organ's regenerative capacity. |
||
|
11:50–11:57
Macroscopic Characterization of Hepatocellular Carcinoma
Stéphanie Gonvers, Lausanne
AbstractBackgroundFollowing the genotype-to-phenotype paradigm, gross findings of hepatocellular carcinoma (HCC) presumably recapitulate histological and molecular traits of HCC. Macroscopy may thus be an invaluable source of prognostic factors in HCC. AimsTo provide an in-depth analysis of macroscopic characteristics of hepatocellular carcinoma and their prognostic value. MethodsInternational multicentric retrospective analysis of patients undergoing partial hepatectomy (PH) for treatment-naïve HCC, between 2010 and 2020. A comprehensive list of 32 macroscopic items was established for a thorough characterization. Pictures of the specimens, either fresh or formalin-fixed were used to characterize HCC gross findings. Other demographical, clinical, biological and histological variables were also collected and analyzed. Multivariable cox regression analysis was performed to identify prognostic factors of overall survival (OS). ResultsA total of 213 HCC patients were included, with 53 women (24.9%), a median age of 60 years [53-68] and 191 BCLC-A stage (90.1%). PH included 93 (57.4%) and 69 (42.6%) minor and major PH, respectively. Median OS was 59 months [25-121]. On multivariable analysis, ECOG performance status (HR, 2.21; 95% CI, 1.13-4.32; p=0.021), microvascular invasion (HR, 2.37; 95% CI, 1.09-5.19; p=0.03), number of nodules (HR, 1.84; 95% CI, 1.09-3.10; p=0.022) and satellites (HR, 2.81; 95% CI, 1.01-7.77; p=0.047) were identified as independent prognostic factors of OS after PH for HCC. ConclusionThese results confirmed the prognostic value of macroscopic factors such as satellites and the number of HCC nodules. Future studies exploring prognostic scores or nomograms deriving from macroscopy are warranted. |
||
|
10:30 – 12:00
Auditorium B
|
My worst nightmare and my coping strategies
Minoa Karin Jung, Geneva; Seraina Faes, Zurich
|
|
|
Main Session
|
||
|
10:30–10:45
My worst polytrauma
Valentin Neuhaus, Zurich
|
||
|
10:48–11:03
My worst colorectal case
Frédéric Ris, Geneva
|
||
|
11:06–11:21
My most difficult patient
Guido Beldi, Bern
|
||
|
11:24–11:39
My overloaded work schedule, how to prevent burnout and handle professional sacrifices
Beat Müller, Basel
|
||
|
11:42–11:57
How to cope with the emotional weight of surgery, complications and high responsibility
Michel Adamina, Fribourg
|
||
|
10:30 – 12:00
Room 1C
|
Prix NaCHwuchs
Anthony de Buys Roessingh, Lausanne; Stephanie Gros, Basel
|
|
|
Free Communication
|
||
|
10:30–10:42
Incidence and predictive factors of perforated appendicitis in children and adolescents before, during and after the COVID-19 pandemic and long-term complications after appendectomy
Niko Keller, St. Gallen
AbstractBackgroundThe COVID-19 pandemic disrupted healthcare systems globally, potentially delaying medical care for conditions like appendicitis. It is known that depending on the duration of symptoms perforated appendicitis may lead to serious peri- and postoperative complications. This may lead to an impaired long-term quality of life. AimsThe aim of this study is to assess whether the COVID-19 pandemic and related health care restrictions had an influence on the incidence of perforated appendicitis in our region. Furthermore, we aimed to investigate predictive parameters for perforated appendicitis and gain knowledge to use this for amelioration of the management of this potentially life-threatening disease. MethodsA retrospective, single center cohort analysis was conducted on children and adolescents under the age of 18 who underwent appendectomy for appendicitis between 1st January 2016 and 31st December 2022. 506 Patients were stratified into three periods: pre-pandemic, pandemic, and post-pandemic. Data on demographics, pathology, clinical presentation, laboratory values, time of symptoms, readmission on emergency room (ER) before treatment, hospital length of stay and complications were analyzed. ResultsPerforation rate was not significantly higher during the pandemic (22.5%) compared to pre-pandemic (23.6%) and post-pandemic (29.0%) periods (p = 0.331). Duration of symptoms was significantly shorter (38.24h) compared to pre- and post-pandemic (49.64h) periods (p < 0.05). There was no difference in complication rates compared to the non-pandemic periods. Predictive parameters for perforation are CRP (Cutoff 46.5mg/l), relative neutrophile count (Cutoff 79,4%) and duration of symptoms (Cutoff 30h). ConclusionIn our region the COVID-19 pandemic did not lead to an increased incidence of perforation and therefore more complications. It even showed a reduction due to significantly reduced duration of symptoms, possibly due to less waiting time in the ER. We found predictive parameters for perforation. This guides clinicians to a more accurate management with better selection of operation technique and reduction of complication rates. |
||
|
10:45–10:57
Balanitis and lichen sclerosus: a case series
Alexandre Dontschev, Fribourg
AbstractBackgroundAcquired phimosis and its complications are among the most common indications for a surgical referral in children. Aetiology is based on chronic inflammation with an auto-immune component. Differential diagnosis includes, post-traumatic scar tissue, balanoposthitis and lichen sclerosus (LS). Treatment options include first a conservative approach with topical corticosteroids followed by circumcision if conservative management fails. AimsTo report a series of 8 cases of LS in male children. Methods8 male children were included in this study, each presenting a history including persisting phimosis, foreskin ballooning during micturition, balanoposthitis, dysuria, use of abdominal musculature during micturition or prior generalized viral infection with genital involvement. Clinical examination showed an atrophic, hypopigmented foreskin and meatal narrowing with a pathological uroflowmetry. No extragenital lesions were found. ResultsConservative treatment was attempted in all 8 cases, to no avail. Circumcision was performed in all cases, with meatoplasty in 3/8 children. Complete clinical response at 6 weeks post-operatively was observed in 7/8 patients. In one case, post-operative topical corticosteroids were necessary, given an obstructive pattern on post-operative uroflowmetry. Histological examination confirmed the clinical LS suspicion. Follow-up consisted of repeated clinical examination and in some cases uroflowmetry. There was no recurrence at 1-year follow-up. ConclusionLS can lead to urethral narrowing and ultimately bladder dysfunction if not treated appropriately. Careful physical examination, close follow-up and appropriate medical and surgical management is important in order to optimize outcomes. This case series illustrates the clinical aspects of LS, the need for a histopathological diagnosis in order to optimally tailor management and the important role of circumcision as a definitive solution. Furthermore, there exists no paediatric randomized controlled trials examining the exact type and duration of topical corticosteroids used to treat LS conservatively. |
||
|
11:00–11:12
Prospective evaluation and follow-up of testicular torsion by TWIST score in children
Nora Manz, Basel
AbstractBackgroundTo enable prompt surgical treatment in high suspicion of testicular torsion and guidance for the use of sonography for intermediate risk scores only, the TWIST score was established in 2013 by Barbosa et al and has been implemented in our institution in 2022. AimsOur aim was to evaluate current use of the TWIST score at our institution, adherence to our institution’s recommendations and perform a survey-based clinical follow-up. MethodsSingle center prospective observational cohort study on children with acute testicular pain based on a follow-up questionnaire and patient’s clinical data. Patients were labeled by our emergency staff and contacted by our study doctor first by mail, including consent form and a 13 question survey regarding recovery, and later also by phone call to clear questions. If consent was given, the patients clinical data was collected from our patient information system. Data was entered into REDcap and analyzed using R Studio. ResultsOf 100 eligible patients, 40 male patients with median age of 11 years (IQR 8;13) participated. TWIST score was considered low risk (0-1 points) in 30% (12/40), intermediate (2-4 points) in 55% (22/40) and high risk (5-7 points) in 15% (6/40) of patients. Surgery was performed in 11 of 40 patients (27.5 %) of which 9 (82%) had testicular torsion and 2 (18%) had hydatida torsion. Patients with high risk scores all had intraoperatively confirmed testicular torsion. Based on our follow-up questionnaire and clinical database, no testicular torsion was missed. ConclusionThe TWIST score provides a triage tool for patients with testicular pain and enables a more objective assessment of clinical findings. All patients with high risk scores were operated due to testicular torsion and no testicular torsion was missed in patients with low and intermediate TWIST score. |
||
|
11:15–11:27
Establishment of a 3D-Immunofluorescence Spatiotemporal Imaging Approach Utilizing Supervised Machine Learning Segmentation
Julian L. Muff, Basel
AbstractBackgroundShort bowel syndrome is a malabsorptive disorder, characterized by a lack of functional small intestine commonly seen after major intestinal resections. A potent treatment approach involves promoting crypt fission, which facilitates the growth of new tissue. Studies employing helminth infections in mice have demonstrated an augmented rate of crypt fission in the small intestine. AimsOur objective is to characterize methods (e.g. helminth infections) aiming to increase the surface area of the small intestine (i.e. promote crypt fission) in mice and humans. MethodsWe utilized an immunofluorescence staining for vasculature, lymphatics and stem-cells. Whole tissue segments of mouse and human small intestine were assessed using a novel three-dimensional spatiotemporal imaging approach. Subsequent analysis of 3D images was performed exploiting supervised machine learning segmentation and classification into vasculature, lymphatics and small intestinal stem-cells. ResultsWe were able to establish a protocol for a spatiotemporal imaging approach in the small intestine utilizing supervised machine learning segmentation. Preliminary results in helminth infected mice indicate that the fissioning rate of crypts increases from 8.5% at steady state to 26.1% upon infection with H. polygyrus at day 14, representing a method for inducing small intestinal growth. Our protocol has been adapted to and piloted in human small intestinal samples. ConclusionThree-dimensional spatiotemporal imaging of mouse and human small intestine with subsequent machine learning segmentation and classification is feasible and introduces a novel approach for studying various human disease and treatment methods. |
||
|
11:30–11:42
A Preliminary Decision Score for Limb-Sparing Surgery vs. Amputation in Pediatric Osteosarcoma
Marc Georges, Lausanne
AbstractBackgroundDecisions regarding surgical strategies for limb osteosarcoma in children and adolescents are complex. While limb-sparing surgery is the primary goal, amputation may be required in cases of extensive local invasion or advanced disease. These decisions are heavy for both surgeons and patients, yet they often rely on clinical judgment rather than systematic, evidence-based tools. AimsThis study aims to propose and preliminarily validate a preoperative score to identify patients at higher risk of requiring amputation, offering a more objective framework for surgical planning. MethodsA scoring system was developed based on literature review and clinical observations, incorporating demographic, clinical, anatomical, radiological, and histological parameters. Major criteria were weighted at 10 points, while minor criteria added 5 points. This retrospective, single-center study included 20 pediatric patients treated at a tertiary hospital between 1994 and 2018. Patients were divided into two groups based on treatment outcomes: (A) “successful limb-sparing surgery” (no recurrence or surgical revision within five years) and (B) “amputation” (primary or secondary and failed limb-sparing surgery within five years). The score was calculated for all patients at diagnosis. ResultsThe amputation group showed significantly lower scores for local recurrence (Median = 5.0 vs. 15.0; p=0.030) and surgical revision (Median = 2.0 vs. 10.0; p=0.037). Five-year mortality (p=0.028) and metastasis development (p=0.022) were also significantly different. The scoring system demonstrated moderate inter-rater reliability (κ=0.696). ConclusionThis preliminary score shows promise as a decision-making tool not only for guiding initial surgical strategies and improving outcomes, but also for reducing family psychological distress with early strategy awareness and adjusted expectations. Lower scores appear to be correlated with more severe disease, underscoring its potential to identify high-risk patients systematically. Further validation with larger cohorts is needed. |
||
|
11:45–11:57
Outcomes of Colonic and Gastric Tube Transplants after Caustic Esophageal Burn in Children: A 33-Year Review
Michaël de Sousa Amaral, Lausanne
AbstractBackgroundAccidental caustic burns of the esophagus in children represent a significant global health challenge, often necessitating esophageal reconstruction. AimsThis study aims to compare the efficacy and morbidity related to esophagus replacement with colonic and gastric tube transplants in a pediatric population followed for caustic stenosis. MethodsThis retrospective study was conducted at a tertiary pediatric surgery unit. Children were treated from January 1989 to December 2022. We compared colonic and gastric tube esophageal replacement. Short-term (within 30 days) and mid-term outcomes and complications were reviewed. Chi-square test for categorical data analysis. ResultsA total of 124 children with caustic esophageal burns were included. Among them, 23 (18.5%) had a gastric tube transplant for esophagus replacement and 101 (81.5%) a colonic transplant. During surgical intervention, we found a significantly higher risk of complications when using a colonic transplant (34%, p < 0.001). For postoperative short-term and mid-term complications, there was no significant statistical difference comparing the two techniques. 26% of children required a reoperation, with a higher risk in the gastric tube transplant group (p < 0.001). For endoscopic dilatation after surgery, there was also a significantly higher number of children with a gastric tube transplant (p = 0.005). Overall, 97.6% recovered full normal oral feeding. ConclusionIn our study, colonic and gastric tube replacement are both good options for pediatric esophageal replacement after a caustic injury, with effectiveness in the long term. Gastric tube transplants showed a slightly higher risk of reoperations and higher number of dilatations post-surgery, but our groups are not really comparable due to the much higher number of colonic transplants. However, both surgical options have to be considered during surgery, depending on the surgical anatomy of the patient. Our future research will focus on assessing long-term quality of life and potential risk of neoplastic complications. |
||
|
10:30 – 12:00
Room 1B
|
SCS Guest Society 2025 : Swiss Plastic SurgeryExcellence through collaboration. Case-based discussion.
Mihai Constantinescu, Bern; Matthias-Kurt Widmer, Wabern
|
|
|
Main Session
|
||
|
10:30–10:50
Flaps 1.0. What residents need to know!
Dirk Schaefer, Basel
|
||
|
10:50–11:05
Case presentation Vascular Surgery (Tandem talk)
Vladimir Makaloski, Bern; Mihai Constantinescu, Bern
|
||
|
11:05–11:20
Case presentation Visceral surgery (Tandem talk)
Samuel Käser, Solothurn; Jan Plock, Aarau
|
||
|
11:20–11:35
Case presentation Trauma (Tandem talk)
Daniel Kalbermatten, Geneva; Axel Gamulin, Geneva
|
||
|
11:35–11:50
Case presentation Thoracic surgery (Tandem talk)
Thorsten Krueger, Lausanne; Yves Harder, Lausanne
|
||
|
10:30 – 12:00
Room 5B
|
State of the Art in Trauma Surgery - Tips and Tricks
Samuel Haupt, Samedan; Tobias Zingg, Lausanne
|
|
|
Main Session
|
||
|
10:30–10:45
Malleolar Fracture
Hans-Curd Frei, Davos
|
||
|
10:45–11:00
Hip fracture
Niklaus Meyer, Winterthur
|
||
|
11:00–11:15
Distal radius fracture
Birgit Oberreiter, Basel
|
||
|
11:15–11:30
Abdominal Trauma Surgery
Beat Schnüriger, Bern
|
||
|
11:30–11:45
External Fixator
Christian Michelitsch, Chur
|
||
|
11:45–12:00
Chest Tube Placement
Loreta Korotcenko, Fribourg
|
||
|
12:00 – 13:00
Room 5C
|
General Assembly – ARS |
|
|
Assembly
|
||
|
12:00 – 13:30
|
Lunch |
|
|
Break
|
||
|
12:00 – 13:30
Room 4BC
|
STS Board Meeting |
|
|
Assembly
|
||
|
12:15 – 13:15
Room 1C
|
Forum SGKC |
|
|
Main Session
|
||
|
12:15 – 13:15
Room 4A
|
General Assembly - Swiss-MIS |
|
|
Assembly
|
||
|
12:15 – 13:15
Room 1B
|
Industry Innovation Session - Distalmotion |
|
|
Industry Innovation Session
|
Sponsors
|
|
|
12:15–13:15
Visceral Surgery in Evolution – Advancements in Robotics with an Expert Panel on the Role of Robotics in Outpatient Surgery
Stefan Breitenstein, Winterthur; Michaela Ehrler, Bern ; Danny Mann, Bern ; Thomas Bührer, Bern ; Marc-Olivier Sauvain, Neuchâtel
|
||
|
12:15 – 13:15
Room 1A
|
Meeting of the Swiss Pediatric Trauma Working Group |
|
|
Assembly
|
||
|
12:30 – 13:00
Booth 108
|
Short Stitch Technique – Is it worth the extra effort? (German session)Sharing expertise with experts and hands-on training |
|
|
Industry Innovation Session
|
Sponsors
|
|
|
13:30 – 14:30
Room 1C
|
Continuing Education in Pediatric Surgery
Stefan Holland-Cunz, Basel; Adrian Marty, Zurich
|
|
|
Main Session
|
||
|
13:30–13:40
Specialised pediatric surgery – How can I get it?
Ulrike Subotic, Basel
|
||
|
13:40–14:00
Competency-based Medical Education and EPAs - Yes, but how?
Adrian Marty, Zurich
|
||
|
14:00–14:10
EPA`s in pediatric Surgery Switzerland
Ulrike Subotic, Basel
presented by the EPA-Group Swiss Society for Pediatric Surgery |
||
|
14:10–14:20
Faculty development in pediatric Surgery Switzerland
Cécile Balmer, Basel
|
||
|
14:20–14:30
Discussion |
||
|
13:30 – 15:00
Room 4A
|
Focus: Personnel du bloc opératoireLes robots s’installent au bloc: Opportunités et Nouveaux Défis pour les Équipes Médicales
Hugo Teixeira Farinha, Lausanne; Lukas Widmer, Fribourg
|
|
|
Course
|
The Swiss Society for Surgery (SGC) is proud to offer a workshop-like session specially tailored to the personnel working in the operating theatre. This 2x90 minutes session is open (for free) to all congress participants. For the OR staff the registration for this congress day and these two sessions is offered by the SGC. The language of the session is French. |
Language(s)
|
|
13:30–13:50
Comment le robot modifie notre quotidien et comment former les futures instrumentistes
Patricia Ferreira, Lausanne
|
||
|
13:50–14:10
Pourquoi j’opère avec le robot et comment nous formons nos futurs chirurgiens
Minoa Karin Jung, Geneva
|
||
|
14:10–14:30
Défis liés à l'utilisation du robot pour la préparation du patient et le rôle de l'anesthésiste pendant l'intervention
Arnaud Rey, Lausanne
|
||
|
14:30–15:00
Discussion |
||
|
13:30 – 15:00
Auditorium B
|
SCS - Guardians of the Scalpel: securing excellence - When technology complements surgery
Dieter Hahnloser, Lausanne; Stéphanie Lacour, Lausanne
|
|
|
Main Session
|
||
|
13:30–13:50
Microengineered ultraflexible endovascular instruments (https://www.epfl.ch/labs/microbs/)
Selman Sakar, Lausanne
|
||
|
13:50–14:10
Exploring the Potential of Robotics in Surgical and Endovascular Interventions (https://www.epfl.ch/labs/biorob/rehassist/)
Mohamed Bouri, Lausanne
|
||
|
14:10–14:30
Quantitative Assessment of Skills and Acquisition in Microsurgical Anastomosis (https://www.epfl.ch/labs/lasa/)
Soheil Gholami, Lausanne
|
||
|
14:30–14:50
Mechanics of Surgical Knots (https://www.epfl.ch/labs/flexlab/)
Javier Sabater Gazulla, Lausanne
|
||
|
14:50–15:00
Endoscopy for Determining Tumor Margins in Cancer Surgery (https://www.epfl.ch/labs/lo/)
Victoria Fay, Lausanne
|
||
|
13:30 – 15:00
Room 5A
|
SGT - Free Communication 2
Ilhan Inci, Zurich; Aljaz Hojski, Basel
|
|
|
Free Communication
|
||
|
13:30–13:37
3D RECONSTRUCTION COULD HELP IDENTIFY PATIENTS WHO MAY BENEFIT FROM LUNG RESECTION
Aljaz Hojski, Basel
AbstractBackgroundThe guidelines for surgical planning are based on research data from open lobar resections. The loss of functional lung volume can range from 0 to 10% per segment, sometimes we see a benefit in pulmonary function. The degree of variation in postoperative pulmonary function depends on numerous factors. The aim of this pilot study was to examine the correlation between 3-D simulations (Fig.1) of preoperative functional lung volume and the measured postoperative pulmonary functions. AimsDoes the simulation of post-operative functional lung volume reduction with the three-dimensional (3D) reconstruction software Visible PatientTM (VP) allow to better identify patients suitable for anatomical lung resection than conventional methods? MethodsThis single-centre pilot study included 20 patients (10 females; age 68 ± 10 years) who underwent VATS resection of the right upper lobe between October 2020 and October 2022. Software based 3-D simulations of preoperative lung volume based on HRCT-scans were correlated with the measured pre- and post-operative pulmonary function and compared with results of the 5% per segment rule, and the model proposed by Brunelli et al in 2005. ResultsPatients (8/20) with increased postoperative FEV1[l] 2.40 (0.56) from 2.30 (0.55) compared to decreased FEV1 2.30 (0.52) from 2.60 (0.63) showed a lower proportion of healthy tissue in preoperative VP simulations 76 (18) % vs. 89 (10) %, p=0.045. Fig2&3. Predictions using conventional methods underestimate the actual measured postoperative FEV1. Calculations using the 5% rule 2.04 (0.47) vs. 2.26 (0.58) correlated better than the Brunelli model 1.74 (0.32) vs. 1.85 (0.40). The measured postoperative DLCO [mmol/(min*kPa)] remained constant 6.34 (2.28) from 6.32 (2.51) in the FEV1 increase group. ConclusionThis pilot study indicates that the 3D reconstruction software VP has the potential to better identify patients who could benefit from surgery than conventional methods. However, further multicentric studies are required to confirm our initial results. 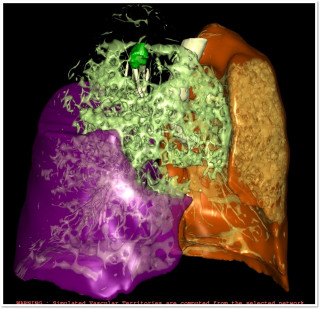
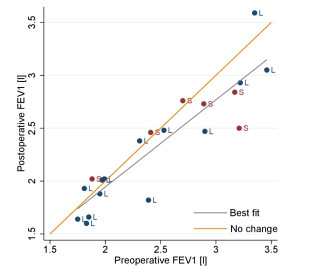
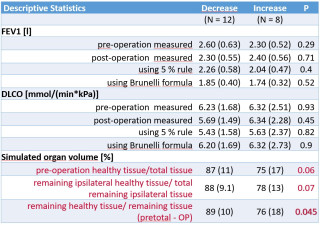
|
||
|
13:40–13:47
Activation of cGAS-dependent necroptosis during cold static preservation of lungs relies on calcium.
Jérôme Lugrin, Epalinges / Lausanne
AbstractBackgroundProlonged cold static preservation (CSP) of lungs has been previously described to engage a type of cell death termed necroptosis. cGAS/STING is an innate immune sensor system for the presence of double-stranded (ds)DNA within the cytosol. We identified that intracellular calcium and mitochondrial (mt)DNA release in the cytosol are potential triggers of cGAS/STING which subsequently activate necroptosis. AimsThis investigation aims at understanding the role played by the cGAS/STING system, notably in the activation of necroptosis, using a cellular in vitro model of CSP. MethodsL2 rat lung epithelial cells were maintained at 4°C with 50% O₂ to mimic CSP. Activation of cGAS/STING/TBK1 pathway was assessed via phosphorylated TBK1 (p-TBK1). Necroptosis was evaluated by detecting phosphorylated MLKL (p-MLKL) and LDH activity. Cytosolic mtDNA was detected by qPCR of cytochrome b (CytB) mitochondrial gene on DNA isolated from cytosolic fractions of cells. mtDNA localization and mtROS production were monitored by confocal microscopy. Preservation with a Ca2+-free solution and the calcium chelator BAPTA-AM were respectively used to study the role of extra and intracellular calcium. Various drugs were employed during CSP to test the mechanisms of mtDNA release. Inhibitors of cGAS, STING and RIPK1 have been used as controls for inhibition of cGAS/STING and necroptosis. ResultscGAS/STING activation is key in triggering necroptosis during CSP. Inhibiting cGAS/STING blocked necroptosis; inhibiting necroptosis did not reduce p-TBK1. CSP-exposed cells showed increased cytosolic mtDNA and mtROS. Calcium depletion in the preservation solution or intracellular calcium chelation significantly reduced pTBK1 and totally blocked necroptosis. Inhibiting known mtDNA release mechanisms did not block cGAS activation or necroptosis. ConclusionCalcium influx and mtDNA release trigger cGAS-dependent necroptosis during CSP. Understanding mtDNA release mechanisms may lead to strategies - like reducing calcium or adding cGAS/STING inhibitors - to improve organ viability in transplantation. |
||
|
13:50–13:57
The Impact of Abdominal Normothermic Regional Perfusion on Short-term Outcomes of Lung Transplantation after Donation after Circulatory Death
Ilker Iskender, Zurich
AbstractBackgroundNormotermic regional perfusion of abdominal organs (aNRP) has been introduced to improve the outcomes of abdominal transplants from donation after circulatory death (DCD) donors. However, the lungs are susceptible to additional warm ischemic injuries during aNRP, which is a well-known risk factor for the development of primary graft dysfunction (PGD) in lung transplantation (LTx). AimsIn the present analysis we wanted to assess the impact of aNRP on the early outcomes of DCD-LTx. MethodsUsing a prospectively maintained database, we compared the short-term outcomes of patients receiving DCD lungs obtained after aNRP versus the standard rapid recovery technique from the initiation of the aNRP program as of 2020 at a single center. PGD3 within the first 72h was the primary outcome measure followed by hospital stay and graft survival. ResultsThe cohort consisted of 41 DCD LTx (33 standard and 9 aNRP) between 01/2020 and 06/2024. Baseline recipient and donor characteristics, recipient comorbidities, and diagnosis, and EVLP rate did not differ significantly between both groups. Expectedly, functional warm ischemic time, from hypotension (MAP<50mmHg) until pulmonary flush, was markedly longer in the aNRP group (71±12 min) than in the standard (34±17 min), p<0.001 (Figure A). PGD3 within 72h was 28% in the standard DCD versus 0% in the aNRP group (p= 0.08). ICU (16 vs 7 days, p=0.2) and hospital stay (40 vs. 29 days, p=0.5) were comparable between the standard and aNRP groups. Kaplan-Meier survival curves did also not differ significantly between two groups, p=0.8 (Figure B). ConclusionIn this initial experience after introduction of aNRP, procurement of donor lungs after initiation of aNRP did not negatively affect short-term outcomes of DCD-LTx. 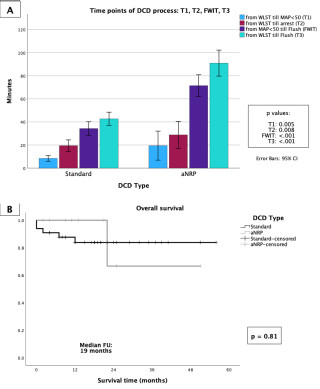
|
||
|
14:00–14:07
Inflammatory markers as risk factors for prolonged ICU stay and hospitalization in patients with chronic thromboembolic pulmonary hypertension undergoing pulmonary endarterectomy
Bianca Battilana, Zurich
AbstractBackgroundChronic thromboembolic pulmonary hypertension (CTEPH) is a potentially fatal disease often associated with preceding acute pulmonary embolisms. Pulmonary endarterectomy (PEA) is the gold standard treatment for surgically accessible CTEPH. AimsGiven the complex nature of PEA, and its mostly elective setting, we aim to identify predictive markers for increased perioperative risk. MethodsCTEPH patients undergoing PEA between January 2015 and August 2024 were retrospectively analyzed. The cohort was divided into two groups: patients with postoperative lung reperfusion edema (RPE) and without. ICU stay and hospitalization were analyzed. Preoperative blood values (leucocytes, lymphocytes, CRP, triglycerides, cholesterol, HDL-, Non-HDL- and LDL cholesterol) were evaluated. A linear mixed model was employed to identify risk factors associated with prolonged ICU stay and hospitalization for patients with and without RPE. A p-value of <0.05 was considered significant. Results130 patients with CTEPH underwent PEA from 2015–2024. Our cohort consists of 53 (40.7%) female patients. Median age was 62 years (IQR 50-72). 71 (54%) patients had NYHA class III and 39 (30%) class II. Figure 1 shows a significant difference in CRP in the patients with RPE and the ones without (p=0.0072). There was a significant correlation between the preoperative CRP levels and hospitalization time (p=0.017) and preoperative CRP levels and ICU duration (p=0.00038) for the group with postoperative RPE[Opi1] . We did not record any significant correlation between any of the other previously mentioned preoperative blood values and the ICU stay or hospitalization in either group. ConclusionElevated preoperative CRP levels are associated with longer ICU stays and hospitalization in patients with RPE. This finding underscores the critical importance of optimizing preoperative inflammatory status to reduce postoperative RPE and recovery times. 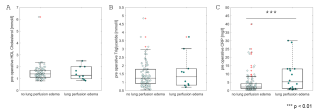
|
||
|
14:10–14:17
PULS (Pulmonary artery sarcoma) – an international collaboration for the assessment of pulmonary artery sarcoma patients’ outcome
Bianca Battilana, Zurich
AbstractBackgroundPulmonary artery sarcomas (PAS) are rare with a poor prognosis and limited curative therapeutic options. This scarcity of evidence poses significant challenges. AimsThis study aims to enhance the understanding of clinical characteristics and current management of PAS. MethodsAn international working group (PULS) was launched. Patients with PAS treated at participating institutions between 1994-2024 were included. Six centers collected data from patients diagnosed with PAS retrospectively. ResultsAmong 49 patients with PAS, the median age was 54.0 years (range: 27.0–82.0), including 24 females (49.0%). Chest pain, dyspnea, and cough were present in 24.5% (n=12), 42.9% (n=21), and 24.5% (n=12), respectively. Initial diagnosis included PAS in 26.5% (n=13) and embolism in 24.5% (n=12). PAS was confirmed by surgery in 40.8% (n=20), imaging in 16.3% (n=8), and biopsy in 12.2% (n=6) and this information is missing in 30.6% (n=15). 33 (67.3%) patients underwent surgery. Tumor endarterectomy was most common, (n=20, 40%), including 1 (2%) patient undergoing additional lobectomy, and two (4.1%) patients additional pneumonectomy. 9 (18.3%) patients underwent pneumonectomy only and 4 (8.2%) debulking surgery only. 10 (20.4%) patients underwent multimodal treatment. One (2%) patient received neoadjuvant systemic therapy. Postoperative adjuvant systemic therapy (Doxorubicin/Ifosfamide) was given to 7 patients (14.3%) and 6 patients (12.2%) underwent radiotherapy. The 1-,2- and 5-year survival was n=20 (40%), n=14 (28.5%), and n=1 (2%) respectively. The subgroup of patients undergoing multimodal treatment had a better overall survival (p=0.05, Figure 1). Relapse of PAS occurred in 32.7% (n=16). ConclusionTo date this is one of the largest reported multi-center cohort of patients with PAS. Our findings highlight the clinical variability in PAS presentation, challenges in achieving a timely diagnosis, and poor prognosis. Outcomes are most promising if patients undergo surgery embedded in multimodality treatment compared to patients undergoing surgery alone. 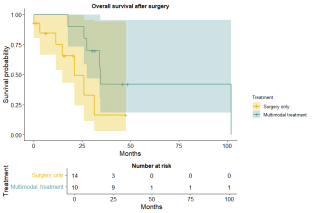
|
||
|
14:20–14:27
Impact of Continuous Negative External Pressure on respiratory function and hemodynamics in post-lung resection and rib fracture patients
Benoît Bédat, Genève
AbstractBackgroundContinuous Negative External Pressure (CNEP) is a non-invasive therapy that applies consistent negative pressure to the chest, enhancing lung expansion and providing respiratory support. AimsTo evaluate, for the first time, the impact of CNEP therapy on patients following anatomical lung resections and on those with rib fractures. MethodsA retrospective study was conducted to assess the effects of a 60-minute CNEP therapy session in two patient groups: (1) those who underwent anatomical lung resection for lung cancer and presented with oxygen saturation (SpO₂) <95% on room air, and (2) patients with rib fractures hospitalized for pain management without surgical intervention. Ventilation distributions were measured using Electrical Impedance Tomography (EIT), and non-invasive hemodynamic monitoring assessed heart rate (HR), cardiac output (CO), tidal volume (TV), oxygen saturation (SpO2), respiratory rate (RR) and shunt fraction. Pre- and post-intervention data were analyzed using paired t-tests or non-parametric tests. ResultsThe study included 15 patients who underwent anatomical lung resections and 14 patients with rib fractures. In lung resection patients, SpO₂ increased from 92.7% (±1.3) to 95.3% (±0.6) (p < 0.001), and RR decreased from 17.6 to 15.4 breaths/min (p < 0.001). Pulmonary ventilation in postero-basal lung zones improved significantly (p < 0.001) (Figure 1). CO increased from 4.9 L/min (±0.8) to 5.2 L/min (±0.8) (p < 0.001), while HR decreased from 75.3 bpm (±5.8) to 72.9 bpm (±4.8) (p = 0.042). Rib fracture patients showed similar trends, with improvements in SpO₂, RR, lung expansion, CO. Pain scores improved significantly after CNEP (p < 0.001). Shunt fraction decreased significantly in both groups (p < 0.001) (Figure 2). ConclusionThis pilot study shows that CNEP significantly enhances lung expansion and hemodynamic stability in patients who underwent anatomical resections and after rib fractures. Further studies are necessary to confirm its broader clinical benefits. 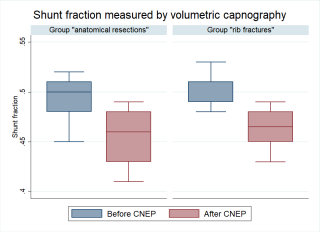
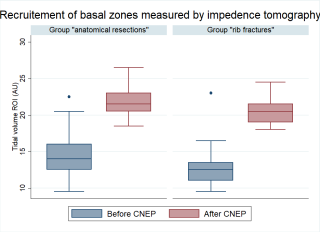
|
||
|
14:30–14:37
Implant Irritation and Removal Rates in Operatively Treated Multiple Rib Fractures: A 49-Month Follow-Up Study.
Florian Smayra, Lucerne
AbstractBackgroundLittle is known about the prevalence, impact and change of the symptoms after implant removal due to irritation in multiple rib fractures. AimsThis study aims to explore these aspects to improve treatment decision-making. MethodsData was collected from two hospitals in the Netherlands and Switzerland. The study included only adults with operatively treated multiple rib fractures, regardless of whether the fractures were flail or non-flail. The primary outcome was the incidence of implant removal due to irritation. Secondary outcomes included implant irritation not leading to removal, other postoperative complications, and remission rates after implant removal. These outcomes were assessed during a follow-up phone call using a standardized questionnaire. ResultsHundred-twenty patients were identified, with 83 (69.2%) completing the final follow-up after a median of 49 months (IQR 40-59). Twenty-five (30.1%) patients experienced implant irritation, of whom four (4.8%) got their implant removed. Two (2.4%) reported significant improvement, one (1.2%) moderate, and one (1.2%) no improvement of symptoms. ConclusionImplant irritation in patients with multiple rib fractures is a common problem, even years after surgery, without guaranteed symptom improvement post-removal. These results provide an additional argument to be more selective in offering rib fixation to patients with multiple rib fractures in the first place. |
||
|
14:40–14:47
Precursor T-cell Exhaustion Characterizes Improved Survival in Non-Immunotherapy Treated Oligometastatic Lung Adenocarcinoma with Brain Metastases
Raphael S. Werner, Zurich
AbstractBackgroundT cell exhaustion describes a hypofunctional state characterized by progressive loss of T cell effector functions and is considered a pathway of resistance for cellular immunotherapies. However, little is known about the prognostic value of T cell exhaustion in patient who do not receive immunotherapy. AimsWe aimed to investigate the prognostic significance of T-cell exhaustion in non-immunotherapy treated oligometastatic LUAC with brain metastases. MethodsPatients with synchronous or metachronous oligometastatic LUAC and brain metastases (BM) who underwent local ablative treatment including surgical resection of the primary tumor were retrospectively identified. No immunotherapy was given as first line treatment. Digital gene expression analysis was performed on extracted RNA using the NanoString nCounter platform. To assess status of T-cell exhaustion, CD83 and CXCL13 were used as markers for precursor exhausted T cells (TPEX). ResultsDigital gene expression analysis was performed on 36 patients with oligometastatic LUAC and BM. Median overall survival (OS) from BM diagnosis was 46 months (IQR 22-67). In the CD83 high group (cutoff 1463), median OS was significantly longer with 103 (95% CI 34 - NR) months in comparison to 36 (95% CI 34 - 63) months in the CD83 low group (HR 4.04 (95% CI: 1.55 – 10.5), p=0.002). Similarly, median OS was longer in the CXCL13 high group with 81 months (95% CI 36 - NR) months in contrast to the CXCL13 low group with 32 months (95% CI 14 – NR), (HR 2.89 (95% CI: 1.21 – 6.92), p=0.013). ConclusionThe findings of this study suggest that also in non-immunotherapy-treated patients with oligometastatic LUAC, precursor T cell exhaustion may be a prognostic parameter, supporting the evidence from other cancer entities that T cell exhaustion reflects poor cancer control. Approaches to mitigate terminal T cell exhaustion by targeting the CXCL13/CXCR5-axis and downstream molecules may be promising. 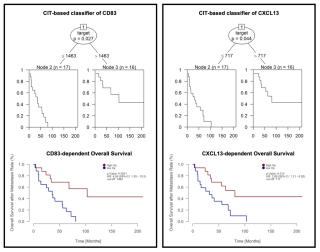
|
||
|
14:50–14:57
Is Attrition to Surgery even less in a Real-World Setting of Neoadjuvant and Perioperative Immune Checkpoint Inhibition for Non-Small Cell Lung Cancer
Raphael S. Werner, Zurich
AbstractBackgroundNeoadjuvant and perioperative immune checkpoint inhibition (ICI) has been shown to provide excellent outcomes within recently published phase III trials on resectable non-small cell lung cancer (NSCLC). However, high preoperative attrition rates of up to 20% after neoadjuvant ICI remain a central challenge and real-world data that support the treatment protocols are scarce. AimsWe aimed to report real-world data after neoadjuvant and perioperative ICI. MethodsBy review of the prospectively maintained clinical NSCLC database, we identified patients with resectable UICC stage II-III NSCLC who underwent 3-4 cycles of induction ICI (all agents) within a neoadjuvant or perioperative regimen with intended surgical resection. Patients treated within ongoing or blinded clinical trials were excluded. ResultsThe analyzed cohort of 25 patients included 3 clinical stage IIB, 18 stage IIIA and 4 stage IIIB cases. Attrition to surgery occurred in 12% (progressive disease in 2, cardiac failure in 1 case). 22 patients underwent surgical resection including 14 lobectomies, 3 bilobectomies and 5 pneumonectomies. Surgery was performed minimally invasive in 46% (6 RATS and 4 VATS cases). R0 resection was achieved in 100% and pathological complete response (pCR) was found in 27%. Among 10 patients with clinical N2 disease who underwent surgery, nodal downstaging to ypN0 occurred in 4 patients (40%). In patients who underwent surgical resection, median EFS was 37 months and median OS was 50 months. Median OS was significantly longer in patients who underwent resection when compared to non-resected patients (50.0 [33.6–72.5] vs. NR [1.2–NR] months; p=0.007). ConclusionOur single-center experience, confirms the findings from the phase III trials in a real-world setting and demonstrates R0-resection in 100% of the patients, as well as excellent pCR rates and long-term survival. In our limited sample size, the attrition rate of 12% is lower than the reported rates in clinical trials, nevertheless highlighting the importance of precise patient selection. 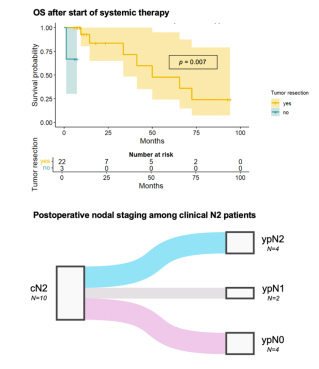
|
||
|
13:30 – 15:00
Room 4BC
|
STS - Free Communication
Severin Meili, Schaffhausen; Michael Dietrich, Zurich
|
|
|
Free Communication
|
||
|
13:30–13:37
Comparative Biomechanical Analysis of Radial Neck Plate versus Tripod Fixation in Mason Type III Radial Fractures: A Human Cadaveric Study
Moritz Kraus, Zurich / Davos
AbstractBackgroundProximal radius fractures, particularly Mason Type III, represent a challenge in elbow surgery due to their complexity and impact on joint function. Using the conventional radial-neck plate is a reliable treatment option, that can cause soft tissue irritation and restricted range of motion. A novel tripod fixation approach, using three crossed screws, should minimize such complications and preserve range of motion. AimsThis study aims to compare the biomechanical competence of conventional radial neck plating versus tripod fixation in a Mason Type III fracture model MethodsSixteen paired human cadaveric radii underwent a standardized osteotomy to simulate a transverse neck fracture with an additional 50:50 head split component and split into two groups – Group 1 fixed with a conventional radial-neck plate with two additional canulated headless compression screws (HCS) and Group 2 stabilized with tripod fixation (three cruciated 40 mm HCS) and two additional HCS. Biomechanical tests assessed stiffness in anteroposterior and mediolateral bending, axial compression, pronation, and supination. ResultsNo significant differences were found in stiffness across the comparisons: mediolateral bending: tripod:195±132N/mm, plate: 91±47 N/mm (p=0.067), anteroposterior bending: plate: 168±105N/mm tripod: 145±108N/mm (p=0.670), axial compression: plate: 643±337N/mm vs. tripod: 642±188N/mm (p=0.998), pronation: plate 0.15±0.10Nm/°, tripod: 0.23±0.23Nm/°(p=0.336), and supination: plate: 0.17Nm/°, Tripod: 0.25±0.21Nm/° (p = 0.351). Cycles to failure under axial compression were recorded with the plate group showing 4078±3173 cycles and the tripod group 4763±5288 cycles, p≥0.4. Load-to-failure was noted at 586±222N for plate and 789±337N for tripod, p≥0.4. ConclusionFrom a biomechanical perspective the tripod technique with two additional HCS showed comparable performance compared to plate fixation with two additional HCS in transverse radial neck fractures with an additional head split component. With potentially less soft tissue irritation and necessary secondary hardware removal the tripod technique seems to be a valid alternative to conventionally used plate osteosynthesis techniques. |
||
|
13:40–13:47
Precontoured low-profile single plates vs conventional plates for midshaft clavicle osteosynthesis: A retrospective comparison
Dominik Brun, Luzern
AbstractBackgroundImplant related irritation and thus re-operation for implant removal are one of the main disadvantages of clavicle plate osteosynthesis. Preshaped low-profile clavicle plates were introduced in recent years, with the aim to improve fit and reduce plate prominence. AimsThis study aims to show whether modern low-profile implants can decrease implant-related irritation and thus reduce re-operations. MethodsAll patients that underwent single-plate osteosynthesis for midshaft clavicle fractures between between 2019 and 2024 at one trauma-center were included. Patients were categorized into two treatment groups: Synthes 3.5mm LCP plates or Synthes 2.7mm VA-LCP low-profile clavicle plates. Treatment groups were compared regarding healing, complications, and removal rate. Results113 patients were included, 60 with a 2.7 VA-LCP, and 53 with a 3.5mm LCP. There were no significant differences in reintervention rate (56.8% versus 52.2%, p = 0.66), infection (3.8% versus 0%, p = 0.22), and non-union (0% versus 4.9%, p = 0.24). Hardware irritation accounted for 88% versus 87% of reinterventions respectively. ConclusionLow-profile clavicle single plating shows similar results in terms of complication and healing rates compared to conventional plating. Despite the design aiming for reduced plate-prominence, it does not demonstrate a significant reduction in removal rates. This suggests that low-profile designs do not sufficiently address the problem of implant-related irritation in clavicle osteosynthesis. Further design improvements and alternative fixation techniques may be considered. |
||
|
13:50–13:57
Addressing Surgical Workforce Challenges in Switzerland: Mentorship and Innovative Solutions
Nina Miesgang, Samedan; Samuel Haupt, Samedan
AbstractBackgroundSwitzerland faces a critical shortage of medical professionals, especially in surgical fields, due to an aging workforce, increasing demand for part-time work, and complex training requirements. The growing gap between retiring specialists and newly trained surgeons is exacerbated by bureaucratic hurdles and insufficient attraction of young talent to surgical disciplines. AimsTo explore innovative strategies for mitigating the workforce shortage, with a focus on mentorship programs involving retired surgical experts to improve clinical education and patient care quality in regional hospitals. MethodsA mentorship project was initiated at Spital Oberengadin, where retired chief surgeons collaborated with junior doctors in the emergency department. This involved interactive patient assessments, hands-on training, and supervised procedures such as wound management and joint reductions. Feedback was collected from participants to evaluate stress levels, learning outcomes, and overall satisfaction. ResultsThe mentorship program significantly enhanced the clinical reasoning and practical skills of young doctors while improving operational efficiency. The initiative was widely appreciated, earning recognition from the Swiss Institute for Continuing Medical Education (SIWF). Additionally, applications for surgical assistant positions in Samedan increased, demonstrating a renewed interest in surgical careers among medical graduates. ConclusionMentorship programs leveraging the expertise of retired surgeons offer a viable solution to the surgical workforce crisis in Switzerland. Expanding such initiatives across regional hospitals could address training gaps, retain talent, and ensure the sustainability of high-quality surgical care. |
||
|
14:00–14:07
Ortho-Geriatric Co-Management - Is There a Return on Investment?
Manuel Känel, Zurich
AbstractBackgroundThe global number of operatively treated proximal femoral fractures is steadily growing. This clinical condition profoundly impacts not only patients' health but also the costs of the global healthcare systems. Models of care based on orthogeriatric co-management (OGCM) have suggested promising clinical outcomes compared to the standard of care (SOC) model in the treatment of frail elderly patients. AimsThe goal of this study was to evaluate the clinical benefits of OGCM in relation to the expected increased daily costs due to the interdisciplinary and interprofessional approach, involving highly specialized and costly personnel. MethodsA retrospective cohort study investigating clinical outcomes in two comparable cohorts of patients aged 75 and older, who underwent surgical treatment for proximal femoral fractures in 2023 was conducted. The two cohorts differed in their perioperative care protocols: one followed an OGCM (n = 143), while the other adhered to a SOC protocol (n = 141). Main outcome measures were readmission, revision, morbidity and mortality rates at 30 days and one-year post-surgery, as well as in-hospital costs. ResultsFindings revealed a positive impact for patients treated under the OGCM protocol, with a downward trend in readmission (36.2% vs 39.7%, p = 0.676), surgical revision (8.4% vs 12.4%, p = 0.485) and mortality (24.1% vs 31.7%, p = 0.781) rates one-year post-surgery. From an economic perspective, the daily costs associated with an OGCM were significantly higher, but the overall costs during the hospitalisation period were slightly lower due to a reduced length of stay. ConclusionOGCM clearly demonstrated a beneficial tendency across all aspects of our investigations, along with a positive financial impact reflected in lower direct costs. Although not statistically significant, we believe it justifies the effort in personnel resources and additional therapy sessions. |
||
|
14:10–14:17
Advancing Trauma Training: Survey Study on Simulation Training and Shock Room Management for Resident Doctors
Lina C. Schreiber, Zürich
AbstractBackgroundSimulation is a cornerstone of modern medical training, particularly for managing polytraumatized patients. Traditional teaching often falls short in preparing residents for the complexities of trauma care, making innovative approaches like Advanced Trauma Life Support (ATLS) courses and simulation training essential for improving skills, teamwork, and decision-making under high-pressure conditions. AimsThis survey evaluated the prevalence and effectiveness of shock room training among resident doctors, its impact on confidence and skill application in trauma care, and areas for improvement in medical education. MethodsAn anonymous online survey was distributed to resident doctors in Switzerland, Austria, and Germany involved in trauma shock room care. Participants across specialties and training levels provided data analyzed using Excel and statistical methods, including p-values and chi-square tests. Ethical approval was not required for this survey-based study. Participation was voluntary. ResultsAmong 124 participants (85 females, 37 males, 1 diverse, 1 undisclosed), training levels and hospital types significantly influenced ATLS course participation (p = 0.033, p = 0.002). ATLS attendees reported higher confidence scores (mean: 3.67 vs. 2.91, p = 0.0024). Functional ID badges, prevalent in university hospitals (83.33%), were positively perceived, especially by female participants. Supervisor support and communication ratings were highest in cantonal hospitals, while unprofessional communication was reported most frequently in university hospitals (25% "often"). ConclusionATLS courses and simulation training significantly enhance residents' confidence and skills in trauma care, with differences in the utilization of these tools depending on hospital type and training level. Introducing trauma training earlier in medical education, increasing its implementation in regional hospitals, and fostering collaborative organizational cultures are essential steps to ensure equitable and effective trauma education. These measures can ultimately improve patient outcomes and address systemic inequalities in healthcare training. |
||
|
14:20–14:27
A Single-Centre Retrospective Study on the Impact of Omitting Preoperative Antibiotic Prophylaxis on Wound Infections in Minor Orthopedic Implant Removals
Cyrill Pfammatter, Zurich
AbstractBackgroundThe use of preoperative antibiotic prophylaxis (POAP) in elective implant removal (IR) is controversial due to a lack of evidence-based recommendations. First-generation cephalosporins, which are commonly used in IR, are believed to reduce wound infection risks. However, the potential for serious side effects had raised concerns about their necessity. AimsThis study intended to evaluate whether omitting POAP in small IR increases the risk of wound infections. MethodsThis retrospective, single-centre cohort study was conducted at a level I trauma centre in Switzerland, including patients who underwent IR between January 1, 2016, and December 31, 2021. The IR procedures involved the upper extremities (UEs), such as the clavicle, olecranon, radius and ulna, as well as the lower extremities (LEs), such as the patella, tibia, fibula, (bi)malleolar and foot. Postoperative follow-up included clinical and radiological evaluations 6 weeks after surgery. The outcomes assessed were deep wound infections, wound healing complications, refractures, persistent pain, bleeding, and neurovascular injuries. ResultsOf the 273 patients (mean age: 42.1 ± 14.5; 44% female), 117 (42.9%) received POAP. In the LE group (n = 141) 51.1% received POAP; in the UE group (n = 132) 34.1% received POAP. Eleven (4.0%) wound-healing disorders were documented, with five (4.3%) in the POAP group and six (3.8%) in the non-POAP group (p = 1.0). No deep wound infections were observed. ConclusionWithholding POAP in elective IR procedures did not significantly increase wound infection rates in our cohort, suggesting it may be unnecessary in uncomplicated IR. |
||
|
14:30–14:37
The use of 3D computer-assisted navigation and its influence on radiation exposure and operation time in the surgical treatment of fragility fractures of the pelvis
Roemalie Haveman, Schwyz
AbstractBackgroundPercutaneous screw fixation is increasingly being used for stabilization of pelvic fragility fractures (FFP) in the elderly. Performing this procedure using 2D fluoroscopy is challenging due to the complex anatomy of the pelvis. 3D computer-assisted navigational imaging techniques have emerged to facilitate the procedure. AimsThis study compares traditional 2D fluoroscopy with 3D computer-assisted navigation regarding radiation exposure and operation time in patients with FFP. MethodsThis retrospective study included patients treated with percutaneous screws for FFP between 1st of January 2017, and 31th of May 2023. Patients were divided into two groups: those treated with conventional 2D fluoroscopy (2D-CF) and those with 3D computer-assisted navigation (3D-CAN). Data on demographics, ASA scores, fracture types and operative parameters were collected. The outcomes were intraoperative fluoroscopy time, operation time and complications. Statistical analyses were conducted, with statistical significance determined at p<0.05. ResultsEighteen patients were included in each group. There were no significant differences in baseline patient characteristics between the groups. Compared to 2D-CF (190.3 ± 86.9 seconds, p=0.000), 3D-CAN showed a significant reduction in fluoroscopy time (78.4 ± 33.7 seconds). The mean operative time was also significantly higher in 2D-CF (85.0 ± 28.1 minutes, p=0.007) versus 3D-CAN (62.1 ± 18.3 minutes). In 3D-CAN no screw-related complications were observed. ConclusionIn surgical treatment of pelvis fragility fractures percutaneous screw fixation with 3D computer-assisted navigation systems significantly reduces patient radiation exposure and operative time in comparison to conventional intraoperative 2D imaging. |
||
|
14:40–14:47
Utility of the 6-Weeks Outpatient Visit After Osteosynthesis of Lower Extremity Fractures
Stephanie Strauven-Heppner, Md, Bonn DE / Luzern DE
AbstractBackgroundAccording to the standard postoperative follow-up protocol, every patient with the most common lower extremity fractures will be seen six weeks after surgery. AimsTo investigate the usefulness of routine six-week outpatient visits and X-rays in patients following surgery for the most common lower extremity fractures, including proximal femur, femoral shaft, tibial shaft and malleolar fractures. MethodsThis retrospective study examined surgically treated patients with the most common lower extremity fractures at a Level 1 trauma center from January 2020 to March 2024. It focused on two outcomes: the incidence of abnormalities found on six-week post-operative X-rays and their consequences, and the incidence of deviations from the local standard postoperative treatment and follow-up protocol. Each was categorized as requiring additional imaging, reinterventions, deviation from standard postoperative weightbearing or range of motion (ROM) restrictions, or additional follow-ups. X-ray abnormalities were defined as any differences between the intraoperative (or direct postoperative) X-ray and the six-week follow-up X-ray. If an abnormality was detected, the hospital records were reviewed to determine its consequences. ResultsA total of 275 patients were included. Abnormalities on X-rays at six weeks were found in 6% of patients. Of all the X-rays, only 2% had clinical consequences, and of those only two patients were asymptomatic. Deviations from standard care based on the entire outpatient visit occurred slightly more frequently (9%), but rarely led to reinterventions. ConclusionClinical consequences from X-ray results were rare during the routine six-week follow-up after surgery for common lower extremity fractures. Complications requiring reintervention were infrequent. In most cases with clinical consequences, the lack of progress during rehabilitation was the reason for the deviation. This suggests that, instead of a routine follow-up, a more selective six-week follow-up - i.e. seeing only symptomatic patients - should be considered.
|
||
|
14:50–14:57
Correlation between Vitamin D and musculoskeletal injuries- A systematic review
Nader Maai, Davos
AbstractBackgroundIt is commonly recognised that maintaining the health of the musculoskeletal system depends heavily on vitamin D. However, the relationship between vitamin D level and the frequency of musculoskeletal injuries is yet uncertain. AimsGathering the available information regarding the connection between vitamin D levels and musculoskeletal injuries was the aim of this systematic review. MethodsSeven electronic databases were searched to find relevant studies for this review. The search technique used Boolean operators to connect MeSH terms and free-text phrases, improving the sensitivity and specificity of the search results. The evaluation included studies that looked into the connection between vitamin D status and damage to the musculoskeletal system. ResultsA high frequency of low vitamin D levels was observed by the 12 included studies in people with musculoskeletal symptoms or injuries. This highlights the significance of vitamin D screening and supplementation in these populations. Certain vitamin D metabolites have been linked to the occurrence of injuries in some studies, indicating that the levels and balance of these metabolites may affect the risk of injuries. However, there have been conflicting findings about how vitamin D supplementation affects muscular function and exercise-induced muscle injury; certain studies have found no appreciable changes. Regarding the advantages of vitamin D supplementation in lowering the incidence of stress fractures in athletes, consistent results have been noted. According to one study, genetic variations may have an impact on how vitamin D and musculoskeletal health are related. ConclusionThe reviewed studies collectively demonstrated a complex relationship between vitamin D status and musculoskeletal injuries. While a high prevalence of low vitamin D levels was consistently reported, the effects of vitamin D supplementation on various musculoskeletal outcomes varied. The findings underscore the need for further research to elucidate the underlying mechanisms and develop targeted interventions for different populations, considering factors such as vitamin D metabolites, supplementation dosage, and genetic variations. |
||
|
15:00 – 15:30
|
Coffee Break |
|
|
Break
|
||
|
15:00 – 17:00
Room 1C
|
General Assembly – SGKC |
|
|
Assembly
|
||
|
15:00 – 15:30
Booth 108
|
Short Stitch Technique – Is it worth the extra effort? (French session)Sharing expertise with experts and hands-on training |
|
|
Industry Innovation Session
|
Sponsors
|
|
|
15:30 – 17:00
Room 5C
|
Acute Care Surgery
Phaedra Müller, Winterthur; Kuno Lehmann, Solothurn
|
|
|
Free Communication
|
||
|
15:30–15:37
A Single-Center Assessment of the Antibiotic Therapy Protocol for Pediatric Patients with Complicated Appendicitis
Estelle Studer, Genève
AbstractBackgroundThe treatment of children with complicated appendicitis (CA) involves administering intravenous antibiotics for several days to prevent postoperative complications. Since 2013, our institutional postoperative management protocol for CA in children has recommended Ceftriaxone/Metronidazole (CM) as the first-line treatment. According to the protocol, if a fever >38.5°C occurs 72 hours after the surgery, a switch to Piperacillin/Tazobactam (PT) is indicated and PT is continued for an additional 5-7 days. Fever is the only criterion used to initiate the CM to PT switch. AimsThis study aims to identify factors that predict the need to switch from CM to PT, enabling PT to be considered as a primary treatment option for more effective management. MethodsThis retrospective study included children aged 0–16 years with CA, treated according to our institutional antibiotic protocol, from 1/2013 to 12/2023. Collected data included patient demographics, medical history, biomarkers, imaging findings, appendix characteristics, surgical details, antibiotics, and additional treatments. Variables were analyzed at three time points: T0, pre-operative assessment; T1, peri-operative period; and T2, first 72 hours post-operatively. ResultsA total of 256 children were included in the study, median age at surgery 10 years (interquartile range: 7–13). Thirty-nine patients (15%) underwent antibiotic switch, while 217 (85%) did not. Factors significantly (p > 0.05) associated with switch included: at T0, generalized peritonitis, dehydration necessitating intravenous fluid bolus, elevated C-reactive protein levels, imaging findings of collections and/or stercolith; at T1, the presence of intra-abdominal abscesses, and prolonged anesthesia and/or surgical duration; at T2, a higher frequency of febrile peaks >38.5°C. Conclusion15% of children with CA required a switch from CM to PT. Several factors appear to predict the need for this adjustment. Patients showing these characteristics are at a higher risk of insufficient response to CM and may benefit from primary treatment with PT. |
||
|
15:40–15:47
Management of Extensive Necrotizing Fasciitis: 2 Cases with 20-40% Total Body Surface Area Involvement and Reconstruction Using BTM Novosorb® and Split-Thickness Skin Grafts
Tanja Drenth, Winterthur
AbstractBackgroundNecrotizing fasciitis (NF) is a severe soft tissue infection requiring aggressive surgical debridement, often resulting in extensive tissue loss. The currently advocated techniques for reconstruction after necrotizing fasciitis are either local flaps, free flaps, or split-thickness skin grafts. Other options include the use of subdermal synthetic material. This case series explores the use of BTM Novosorb®, a synthetic dermal matrix, followed by split-thickness skin grafts as an alternative reconstruction technique for large total body surface area (TBSA) involvement in NF cases. Additionally, we aim to provide an overview of the diagnostic and therapeutic decision-making process for this complex clinical picture in the emergency setting, focusing on rapid assessment and initiation of life-saving measures. Case presentationTwo patients with Streptococcus pyogenes-induced NF were treated: a 33-year-old male with 40% TBSA involvement of the trunk and a 59-year-old female with 20% TBSA involvement of the left thigh and lower leg. Treatment included multiple surgical debridements, antibiotic therapy, intensive care management, application of BTM Novosorb®, and split-thickness skin grafting after BTM integration. The final results showed very well-integrated split-thickness skin grafts without signs of wound dehiscence or persistent infection. For the 33-year-old male patient, we achieved a split-thickness skin graft take rate of 95%, and for the 59-year-old female patient, a take rate of just under 100%. ConclusionWhile various techniques for defect coverage after necrotizing soft tissue infections are described in the literature, our approach using subdermal synthetic material (BTM Novosorb®) followed by split-thickness skin grafts proved effective for large TBSA involvement. With graft take rates of 95-100%, we consider Novosorb a viable alternative to conventional techniques for reconstruction after necrotizing fasciitis, particularly in cases with extensive tissue loss. 


|
||
|
15:50–15:57
Minimally Invasive Management of a Thoraco-Abdominal Penetrating Injury: A Case Report and Review of Current Evidence
Arnaud Losdyck, Geneva
AbstractBackgroundPenetrating thoraco-abdominal injuries (TAI) present significant diagnostic and therapeutic challenges. Prompt recognition and appropriate surgical intervention are crucial to prevent complications. Despite a sometimes impressive penetrating trauma, a minimally invasive approach can be appropriate. This case report details the laparoscopic management of a patient with TAI in our surgical department in the light of the current evidence and practice guidelines. Case presentationA 58-year-old male presented to the emergency department following acute alcohol intoxication and a self-inflicted stab wound with a knife embedded in the inferior left parasternal area. The patient remained hemodynamically stable throughout evaluation. Thoracoabdominal CT imaging revealed the knife penetrating the left thoracic base and hypochondrium. Suspected injuries included the 10th rib, diaphragm, and possibly the stomach. Given the patient’s stability and no major vessel involvement, an exploratory laparoscopy was performed to provide a wide overview with a limited surgical burden. The knife was carefully removed under laparoscopic guidance. Exploration revealed a left paramedian diaphragmatic tear extending into the left perigastric area. The anterior gastric wall had a small, non-transfixing serosal breach, repaired with a single Vicryl 2-0 suture. The diaphragmatic tear was closed using a running absorbable 0 V-lock suture. A monitoring drain was placed, and a postoperative thoracic radiograph confirmed no significant pneumothorax. The drain was removed on day 2, with an uneventful recovery. ConclusionThis case underscores the importance of rapid but thorough assessment of TAI, with CT scans, playing a major role in surgical approach selection. Surgical exploration and repair remain the definitive treatment, but laparotomy, once the gold standard, should not be considered the only option depending on hospital resources and surgeon’s experience. A review of the existing literature and the EAST guidelines suggests that a prompt surgical exploration prioritizing a laparoscopic approach for hemodynamically stable patient reduces the morbidity and mortality in TAI. 
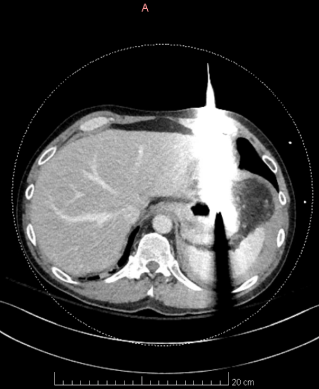
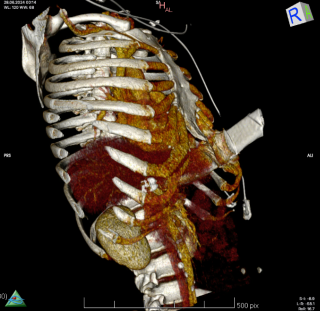
|
||
|
16:00–16:07
Meta-analysis of randomised clinical trials comparing intraumbilical versus periumbilical incision in laparoscopic appendectomy
Justyna Mohr, Münsterlingen
AbstractBackgroundLaparoscopic appendectomy (LA) has become the standard treatment for acute appendicitis. However, surgical site infections (SSI) still occur in up to 8% of patients. AimsThe aim of this review was to compare the short-term outcomes of an intraumbilical incision (IU) with a periumbilical incision (PU) for umbilical port placement in LA. MethodsA systematic literature search was performed in CENTRAL, PubMed, EMBASE and Web of Science. All randomised clinical trials (RCTs) comparing IU with PU port placement were included. Internal organ injury, umbilical SSI, operation time, and length of hospital stay were meta-analysed in a random-effects model. Risk of bias (Cochrane 2.0) was assessed for every RCT and certainty in evidence (GRADE) was determined for every outcome. ResultsSix RCTs from Asia with 1576 patients were included. There was no difference in internal organ injuries (OR 0.70, 95%-CI: 0.34 to 1.43, p=0.33) or umbilical SSI (OR 0.76, 95%-CI: 0.40 to 1.44, p=0.40). In addition, there was no difference in operation time (MD -1.57 minutes, 95%-CI: -5.30 to 2.16, p=0.41) or length of hospital stay (MD 0.17 days, 95%-CI: -1.12 to 1.47, p=0.79). There was a high risk of bias in all included RCTs and the certainty in evidence was low to moderate. ConclusionThere is no difference in all short-term outcomes between IU and PU port placement in laparoscopic appendectomy. Surgeons should use their preferred approach. The body of evidence would benefit from a high-quality study in a Western population. |
||
|
16:10–16:17
A Novel Technical Step During Laparoscopic Cholecystectomy as an Addition to Strasberg’s Safety Rules
Janosch Kränzle, Bern
AbstractBackgroundFrench surgeons performed the first laparoscopic cholecystectomies in 1987/88. It quickly became the standard technique for the majority of indications. The most dreaded complication still is a common bile duct (CBD) injury. In order to minimize CBD injuries, the critical view of safety (CVS) was introduced in 1995 and is widely used ever since. Despite Strasberg’s rules the incidence of CBD injuries still lies between 0.2 – 0.4%. AimsTo introduce a novel and simple non-traumatic technique of visualizing the common bile duct at the beginning of a laparoscopic cholecystectomy as an initial add-on step to Strasberg’s rules. This technique delineates the right lateral border of the hepatoduodenal ligament and helps define the anatomical course and direction of the CBD in the vast majority of cases. MethodsWe recorded short video sequences during consecutive emergency and elective laparoscopic cholecystectomies. All patient data has been anonymized. Prior to the start of this pilot study, the project was presented to the local ethics committee, no ethics application was required. All recorded sequences were combined and are demonstrated in a short video. ResultsFrom June 2024 to January 2025 the technique has been performed in 60 laparoscopic cholecystectomies. The visibility of the CBD was clearly better and the CBD easier to demonstrate in elective cases than in patients with acute cholecystitis. However, even in cases with inflammation, extensive adherences or after previous abdominal surgery the CBD could readily be demonstrated in the majority of patients. ConclusionThis novel technical step to visualize the common bile duct helps surgeons and in particular inexperienced surgeons to orient and navigate during laparoscopic cholecystectomies. We propose to introduce it as a simple non-traumatic initial step prior to the start of the dissection of Calot’s triangle. |
||
|
16:20–16:27
The Influence of Surgical Teaching for Laparoscopic Cholecystectomies on Outcomes: A Propensity Score-Matched National Cohort Study
Joana Rodrigues Ribeiro, Genève / Geneva
AbstractBackgroundTeaching in the operating room represents the cornerstone of surgical education. A sufficient number of basic procedures in training is needed to gain independence. However, it is still debated whether surgical teaching has a negative impact on outcomes. AimsThis study aims to determine the impact of surgical teaching for laparoscopic cholecystectomies on patient outcomes. MethodsWe conducted a retrospective study using the national database of the Swiss Association for Quality management in Surgery (AQC). We identified adult patients who underwent a laparoscopic cholecystectomy between 2009 and 2019. Baseline characteristics were analyzed, and a propensity-score was constructed based on age, gender and American Society of Anesthesiologists (ASA) classification. Patients were then matched in a 2:1 ratio (non-teaching vs. teaching), and surgical outcomes were assessed. ResultsWe included 26’871 cholecystectomies in our analysis. After propensity-score matching, 7’172 interventions used for surgical teaching were compared to 14’344 performed by board-certified surgeons. Mean cohort age was 52 years, and 8% of patients had an ASA >II. A majority of teaching cases were operated in hospitals >200 beds (p<0.001). Teaching was associated with a longer mean operative time (85±39 vs. 77±45 minutes, p<0.001), a higher rate of conversion to laparotomy (29% vs. 12%, p<0.001), but a shorter total length of stay (4.71±5.97 vs. 5.10±7.01 days, p<0.001), and fewer intraoperative complications (0.6% vs. 0.9%, p=0.032). Postoperative complications were similar both in terms of frequency (1.4% vs. 1.5%, p=0.5) and severity with 0.7% requiring surgical management in both groups (p=0.5). ConclusionTeaching of a common surgical procedure such as cholecystectomy appears safe with a similar rate of intraoperative and postoperative complications. Teaching is currently only performed in a minority of procedures and should be promoted further to improve training in Switzerland. 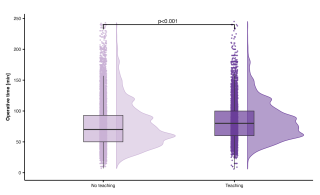
|
||
|
16:30–16:37
Is Measurement of Bilirubin a Valuable Predictive Tool to Detect Choledocholithiasis Before Cholecystectomy?
Jasmin Zeindler, Liestal / Basel
AbstractBackgroundLaparoscopic cholecystectomy is the treatment of choice for acute or chronic cholecystitis and symptomatic cholelithiasis. Preoperative measurement of Bilirubin is standard of care in most surgical clinics, while the predictive value of its measurement to detect choledocholithiasis is questionable. AimsWe aimed to investigate the association of preoperative high bilirubin and detection of choledocholithiasis diagnosed with preoperative MRCP. MethodsThis is a retrospective multicentre cohort study including all patients receiving preoperative MRI-MRCP before undergoing elective or emergency cholecystectomy between 2010 and 2020. Preoperative blood parameters such as Bilirubin and MRCP reports were documented as well as postoperative outcome of the patients. Results3163 patients have undergone laparoscopic cholecystectomy between 2010 and 2020, of which 2568 have shown normal cholestatic parameters preoperatively. Of these patients, 684/2568 (27%) have been male and 1884/2568 (73%) female. The most frequent indications for laparoscopic cholecystectomy have been cholecystolithiasis in 72% (1845/2568) of cases, followed by cholecystitis in 18% (465/2568). The majority of patients (2267/2568, 88%) have received pMRCP, while only 301/2568 have not. We could detect silent CBD-stones in 6% of the patients with normal preoperative cholestatic parameters in MRCP (130/2267). Sensitvitiy of elevated bilirubin to detect CBD stones was only 33%. ConclusionSilent CBD stones are common and MRCP is a good diagnostic tool to detect them. Preoperative elevated bilirubin is not necessarily associated with CBD stones and patients should always receive MRCP. In normal lab tests preoperatively, the value of MRCP regarding cost-effectiveness remains debatable. |
||
|
16:40–16:47
Dexter-assisted Cholecystectomy: the First Prospective Multicenter Study
Lukas Gantner, Zurich / Zürich
AbstractBackgroundThe evolution of robotic platforms has transformed minimally invasive surgery, improving ergonomics and precision. The Dexter robotic system, designed for accessibility and ease of use, offers a new approach to robotic-assisted surgery, particularly for routine procedures such as cholecystectomy. AimsThis study aimed to evaluate the perioperative safety and performance of Dexter-assisted cholecystectomy in a prospective, multicenter, multinational setting. MethodsA prospective single-arm study was conducted across four hospitals in three countries, involving six surgeons with varying robotic surgery experience. Fifty-one patients (32 females, 19 males) underwent robotic-assisted cholecystectomy using the Dexter system for indications including symptomatic cholelithiasis, cholecystitis, choledocholithiasis, and biliary pancreatitis. Trocars ranging from 8 to 12 mm in diameter were used. Follow-up was conducted for 30 days postoperatively. Primary outcomes were the occurrence of Clavien-Dindo grade ≥3 adverse events and procedural success without conversion to open or laparoscopic surgery. Secondary outcomes included other surgical data and postoperative outcomes ResultsHere we report the interim analysis of the perioperative data. The cohort had a median age of 59 years (IQR 42–65) and a median BMI of 28.0 kg/m² (IQR 24.9–29.6). Median skin-to-skin operative time was 58 minutes (IQR 49–78), which included a median docking time of 3 minutes (IQR 2–5) and a median console time of 25 minutes (IQR 21–36). The median estimated blood loss was 5 mL (IQR 0–10), and no blood transfusions required. All procedures were completed successfully without device deficiencies or conversions. Two minor intraoperative complications occurred, none related to the device. Median length of hospitalization was 1 day (IQR 1-2). ConclusionDexter-assisted cholecystectomy demonstrated excellent safety and performance outcomes in elective surgery. The system’s efficiency, minimal blood loss, and absence of device-related complications highlight its potential as a viable robotic platform for routine minimally invasive cholecystectomies. |
||
|
16:50–16:57
Role of Damage control surgery in the treatment of perforated sigmoid diverticulitis
Marie Burgard, Geneva / Fribourg
AbstractBackgroundWhile primary anastomosis (PRA) is a potential option for stable, immunocompetent patients with perforated diverticulitis, non-restorative resection (NRR) remains the most common procedure. NRR frequently leads to permanent stoma and substantial morbidity related to stoma reversal. Damage control surgery (DCS) has gained attention as a potentially superior approach, offering the advantage of a higher stoma-free discharge. AimsTo compare DCS to conventional surgical treatment (NRR/PRA) for perforated diverticulitis, evaluating stoma-free discharge rates and postoperative complications. MethodsA prospective cohort study included 56 patients with Hinchey III/IV diverticulitis. Twenty-six patients (study group) underwent surgery from 2022 to 2024, following the implementation of a DCS-based treatment algorithm. Thirty patients (control group) were operated on from 2020 to 2022 (pre-algorithm implementation). The primary outcome was stoma presence at discharge, 6 months, and 12 months. Secondary outcomes included postoperative complications, hospital length of stay, costs and complications after stoma reversal. ResultsIn the control group, 97% of patients underwent NRR. In the study group 15 % received PRA, while 85% received DCS; of the latter, 18% required conversion to NRR and 82% achieved anastomosis during the second-look procedure (Figure 1). Demographics, post-operative complications and hospital length of stay were similar between groups. The control group hat significantly higher rates of stoma at discharge (100% vs 42.3%, p < 0.001) and at 6 and 12 months (p=0.003). Early complications after stoma reversal dit not differ significantly. Multivariate analysis showed that conventional treatment (NRR/PRA) was independently associated with increased stoma presence at discharge and 6 months (hazard ratio 13.1 p= 0.05, hazard ratio 10.65, p= 0.013, respectively). ConclusionDCS appears to be a safe and effective strategy, resulting in significantly higher rates of stoma-free discharge compared to conventional treatment for perforated diverticulitis. 
|
||
|
15:30 – 17:00
Room 4A
|
Focus: Personnel du bloc opératoireValoriser les équipes opératoires – Bien-être et durabilité
Hugo Teixeira Farinha, Lausanne; Lukas Widmer, Fribourg
|
|
|
Course
|
The Swiss Society for Surgery (SGC) is proud to offer a workshop-like session specially tailored to the personnel working in the operating theatre. This 2x90 minutes session is open (for free) to all congress participants. For the OR staff the registration for this congress day and these two sessions is offered by the SGC. The language of the session is French. |
Language(s)
|
|
15:30–15:45
Pratique chirurgicale et durabilité: le concept de chirurgie verte et ses innovations
Laure-Méline Piotet, Morges
|
||
|
15:50–16:05
Fumées chirurgicales: enjeux et risques en salle d'opération
Laurence Paris, Fribourg
|
||
|
16:10–16:25
Projet d'harmonisation des techniques chirurgicales visant à promouvoir la collaboration interprofessionnelle
Emmanuel Daniel, Geneva
|
||
|
16:30–16:45
Bien-être en salle d'opération: Stress, Anxiété et Impacts des Nuits
Alexis Litchinko, Fribourg
|
||
|
15:30 – 17:00
Room 5B
|
Guardians of the Scalpel: Securing excellence in Hernia Surgery – Progress, Specialisation and Education
Rebecca Kraus, Chur; Henry Hoffmann, Basel
|
|
|
Guardians of the Scalpel
|
||
|
15:30–15:45
Hernia Surgery in Switzerland – Tradition vs. Innovation
Walter Brunner, St. Gallen
|
||
|
15:45–16:00
3 important hernia publications 2024 you should know
Jonathan Douissard, Geneva
|
||
|
16:00–16:15
MILOS vs. eTEP pro & con
Sebastian Lamm, Liestal
|
||
|
16:15–16:30
CPIP – is there a diagnostic and treatment algorithm?
Debora Nowakowski, Basel
|
||
|
16:30–16:45
The perfect hernia training – young surgeons perspective
Sandra Widjaja Kaufmann, Lucerne
|
||
|
16:45–17:00
Robotic hernia surgery – evidence vs. enthusiasm
Sebastiano Spampatti, Bellinzona
|
||
|
15:30 – 17:00
Room 4BC
|
Guardians of the scalpel: securing excellence in the trauma bay
Björn-Christian Link, Lucerne; Birgit Oberreiter, Basel
|
|
|
Guardians of the Scalpel
|
||
|
15:30–15:48
Dos and Don'ts in the pre-hospital and early hospital phase
Johannes Moeckel, St. Gallen
|
||
|
15:52–16:10
Optimized modern trauma bay management - Time is of essence
Daniel Wagner, Lausanne
|
||
|
16:14–16:32
Disaster management: how do we prepare?
Valentin Neuhaus, Zurich
|
||
|
16:36–16:54
Traumatic resuscitation
Beat Schnüriger, Bern
|
||
|
15:30 – 16:30
Room 5A
|
Meet the Expert
Didier Lardinois, Basel; Franco Gambazzi, Aarau
|
|
|
Main Session
|
||
|
15:30–16:10
Current Surgical Management of Stage III NSCLC
Jonathan D. Spicer, Montréal CA
|
||
|
15:30 – 17:00
Room 1A
|
Residents Cup
Zoran Rancic, Lachen; Sébastien Déglise, Lausanne
|
|
|
Free Communication
|
Sponsors
|
|
|
15:30–15:36
Primary Aortic Mural Thrombi as an Embolic Source in Younger, Healthy, Female Patients
Tamina Popp, Solothurn
AbstractBackgroundPrimary aortic mural thrombi (PAMT) are a rare source of limb threatening arterial embolization. In most cases, ischaemia is the first clinical manifestation. While no treatment guidelines exist, various therapeutic regimens have been proposed. This report aims to highlight the clinical presentation, surgical management and outcomes of acute arterial occlusion resulting from PAMT in two young female patients. Case_presentationCase 1 involved a 38-year-old woman with a 3-day history of progressive bilateral leg pain. Imaging revealed multiple embolic arterial occlusions of varying ages and a floating thrombus of the infrarenal aorta (see Figure 1). Case 2 concerned a 44-year-old female with sudden pain, pallor, and paresthesia of the right leg. Imaging confirmed thromboembolic occlusion of the tibiofibular trunk as well as chronic occlusion of all lower right leg arteries and a floating mural thrombus of the proximal right common iliac artery. Both underwent emergent femoro-popliteal and crural embolectomy, followed by staged open thrombectomy (see Figures 2-3), which we favored over an endovascular approach. In case 1, complications included impaired perfusion and compartment syndrome, requiring venous bypass and fasciotomy. Case 2 experienced sufficient perfusion restoration after embolectomy without further interventions. Both patients showed favorable outcomes upon discharge and at follow-up after 6 weeks and 6 months. ConclusionWhile aortic mural thrombi are typically associated with atherosclerosis, aneurysms or hypercoagulable states, they can also occur in the non-diseased vessel. Although conservative and endovascular treatment have importance in this entity, surgical thromboendarterectomy may be the appropriate measure, especially in the event of acute embolization in young, otherwise healthy patients. The cases presented demonstrated the importance of considering PAMT as an embolic source and showed favorable outcomes after surgical therapy in both multiple bilateral and localized occlusions. 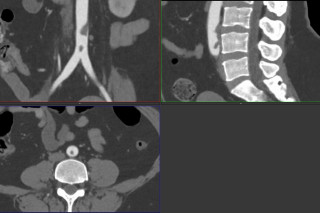


|
||
|
15:40–15:46
Treatment of a Symptomatic High Flow Arteriovenous Fistula With the "Revision Using Distal Inflow" (RUDI) Technique: A Case Report
Chiara Maria Fragati, Locarno
AbstractBackgroundRevision using distal inflow (RUDI) is currently proposed in patients with hemodialysis (HD) access-induced distal ischemia (HAIDI) or having a high blood flow access (HFA). Vascular access related high flows (HF) are common with brachial artery-based fistulas. We describe the case of a patient with episodes of angina pectoris, dyspnoea on exertion and marked hemorrhaing during dialysis puncture due to a 3 L/min HF proximal radio-cephalic fistula. Revision of the arteriovenous fistula with distalisation of the anastomosis using an ulno-cephalic inverted saphenous vein graft was performed. AimsThe aim of our case report is to highlight the complexity and importance of surgical intervention in the case of high flow arteriovenous fistula. MethodsAfter careful study with Echocolour-Doppler and CT scan it is decided to distalise the anastomosis of the ulnar artery. The previous anastomosis was closed and an interposition with the great saphenous vein fed from the ulnar artery (4cm from the bifurcation) and the cephalic vein was performed. ResultsThe post-operative hospitalization was uncomplicated. There was a reduction in flow rate from 3 to 1.3 L/min, with good functioning of the arteriovenous fistula and resumption of dialysis sessions. Additionally, the patient had no more angina like pain on physical exertion. ConclusionMultiple vascular access sequelae, including HF, pose a challenge to the vascular surgeon. RUDI effectively reduces access flow in a high-flow HD vascular access and is a valid surgical option in the treatment of Steal Syndrome. An autologous vein is preferred as an interposition graft. 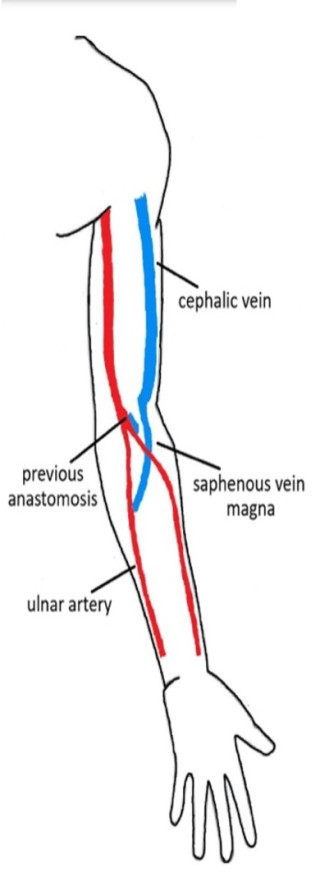
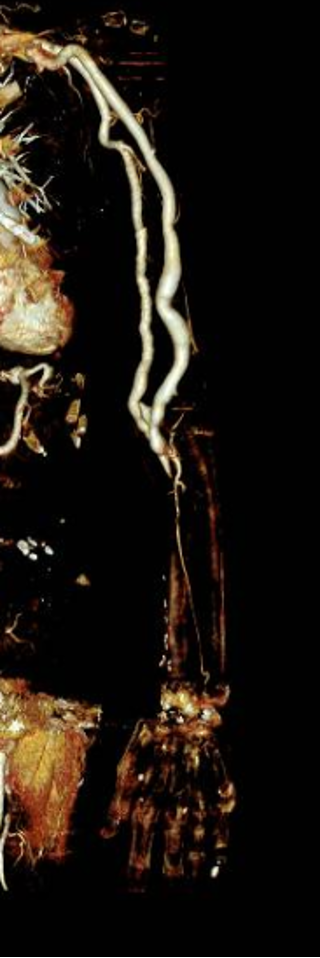
|
||
|
15:50–15:56
Suprarenal Caval Filter Extraction in a Pregnant Patient: A Surgical Success Without Vena Cava Clamping
Antonietta Petrusic, Lugano
AbstractBackgroundInfrequent yet critical complications such as filter migration can arise during endovascular procedures. In severe cases a surgical explantation is needed. Case_presentationWe report a successful surgical removal without clamping the vena cava, reducing the risk of hemodynamic instability, vein bleeding and thrombosis. This case involves a 30-week pregnant patient with unilateral deep vein thrombosis of the iliac-femoral axis, a condition with heightened thromboembolic events. Anticoagulant therapy was initiated. Due to fetal growth restriction, a cesarean delivery required temporary anticoagulation discontinuation and cava filter placement, which was located at the suprarenal level but resulted in tilting. Given the patient’s hemodynamic stability and to avoid additional radiation exposure in pregnancy, the removal attempt was deferred. Another attempt to remove the caval filter was made after delivery. Based on literature review, a midline laparotomy was performed, followed by the rightward rotation of the descending colon and duodenum, which allowed to expose of the inferior vena cava, the right and left renal veins. The suprarenal juxtahepatic vena cava was isolated, and trial clamping was well tolerated. The distal hook of the filter was identified near the confluence of the inferior vena cava and the left renal vein, with its distal margin extending outside the vessel into the periadventitial area. A purse-string suture with tourniquets was placed around the filter hook. The vena cava was incised under continuous flow. The filter was pushed externally and inserted into a 10 Fr introducer, which was advanced into the vena cava to encapsulate and safely withdraw the filter, ensuring effective extraction. The purse-string suture was tightened and knotted, achieving hemostasis. Follow-up at three months revealed no complications. ConclusionPreoperative literature review is crucial in challenging cava filter extraction, highlighting alternative approaches like maintaining continuous venous flow and using purse-string sutures to avoid vena cava clamping and its possible complications. |
||
|
16:00–16:06
High-Grade Leiomyosarcoma of the Inferior Vena Cava With Infiltration of the Right Kidney and Adrenal Gland
Amandine Chavanon, Biel/Bienne / Biel
AbstractBackgroundHigh-grade leiomyosarcoma (LMS) of the inferior vena cava (IVC) is a rare and aggressive malignancy, often presenting with significant local invasion. We report a case of a 55-year-old male with IVC LMS involving the right kidney and adrenal gland, highlighting diagnostic challenges, surgical management, and postoperative progression. Case_presentationA 55-year-old male presented with right-sided paravertebral pain localized to the thoracolumbar junction, accompanied by significant weight loss. MRI revealed a large mixed mass involving the IVC and extending into the hepatic portal. Hormonal screening suggested adrenal carcinoma, and FDG-PET did not indicate distant metastasis. The patient underwent an en bloc resection, including right adrenalectomy, right nephrectomy, vena cava resection with total vascular exclusion, and reconstruction using a Gore-Tex interposition graft. Pathological analysis confirmed a pT2, R0 high-grade LMS of the IVC with infiltration of the right kidney and adrenal gland. Following surgery, the patient was referred to the interdisciplinary Sarcoma Board at Bern University Hospital for follow-up and postoperative treatment. Due to the high risk of recurrence and metastasis (5-year disease-free survival [DFS] rate of 35%), the patient was evaluated for adjuvant chemotherapy. The patient received adjuvant chemotherapy with doxorubicin and dacarbazine. However, after 4 cycles, progressive lesions in the chest wall and lung were noted. A thoracic CT scan confirmed the chest wall nodule's progression, which was resected with an R0 margin. Histology confirmed metastatic disease. The Sarcoma Board recommended active surveillance following the resection. ConclusionThis case underscores the challenges of managing IVC LMS, a rare and aggressive malignancy. Despite initial surgical resection and adjuvant chemotherapy, metastasis to distant sites occurred, emphasizing the need for ongoing surveillance in high-risk patients. Leiomyosarcoma of the IVC requires a multi-disciplinary approach, including aggressive surgery and adjuvant therapy, followed by vigilant long-term monitoring for recurrence or metastasis. Active surveillance remains essential for managing the potential for metastasis after initial treatment, especially given the high risk of recurrence and metastasis in these patients. 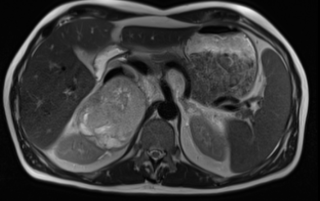
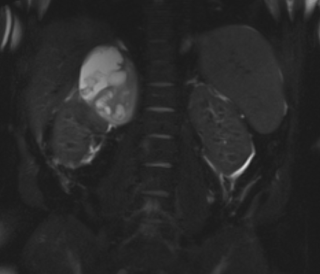
|
||
|
16:10–16:16
Interlobar Renal Artery Aneurysm: A Case Report of Superselective Liquid Embolization.
Chiara Miatello, Villars-sur-Glâne / Fribourg
AbstractBackgroundRenal artery aneurysms, though rare, represent potentially life-threatening conditions, with an incidence of 0.3 to 2.5%. The risk of rupture is 3-5%, with mortality rates of 10% in the general population and up to 60% in pregnant women. Treatment indications are guided on risk factors for rupture (diameter > 20-30 mm, growth rate > 0.9 mm/year, pregnancy) and symptoms. Surgical repair or endovascular approaches (stenting, embolization) are selected according to aneurysm localization and morphology; In rare cases, partial or total nephrectomy may be required. This case report aims to present the effectiveness of selective liquid embolization in treating interlobar renal aneurysms. Case_presentationA 27x16 mm saccular renal aneurysm was Incidentally detected during an abdominal CT-scan of a 56-year-old male. The aneurysm had an interlobar localisation at the superior pole of the left kidney, featuring a narrow neck and perfused by three afferent arterioles. The patient was asymptomatic, with normal renal function. Considering the aneurysm’s size and interlobar location, endovascular management by Onyx-embolization was planned after multidisciplinary board discussion. Onyx-18 is a permanent occlusive agent routinely used in liquid embolization of cerebral arteriovenous malformations. Under general anaesthesia, the intervention was conducted using a transfemoral approach. A selective Cone Beam CT (CBCT) angiography of the renal artery enabled detailed multiplanar reconstruction of the lesion, facilitating precise 3D-guided embolization of all afferent vessels. A total of 2 ml of Onyx-18 was administered. Final CBCT-angiography confirmed complete exclusion of the aneurysm while maintaining renal perfusion, despite a small focal infarction at the superior pole. Postoperative recovery was uneventful and the patient was discharged after 2 days, with preserved renal function. ConclusionSuperselective liquid embolization is a reliable and effective endovascular technique for treating interlobar renal artery aneurysms, ensuring optimal preservation of renal parenchymal perfusion, even in challenging anatomies. Small parenchymal infarctions may occur, without clinical implications. 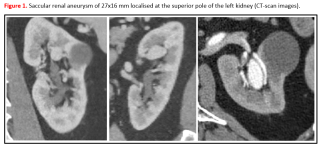
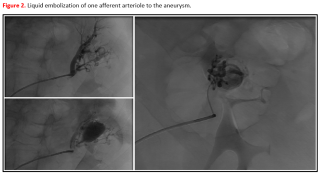
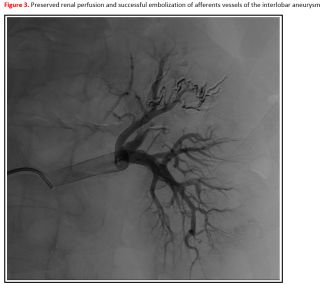
|
||
|
16:20–16:26
Primary Aorto-Enteric Fistula; A Case Report
Marc Rickenbacher, Baden
AbstractBackgroundPrimary aorto-enteric fistula (PAEF) is a rare and life-threatening condition characterized by a direct connection between the aorta and the gastrointestinal tract (GI). It accounts for less than 0.2% of all causes of GI bleeding. While secondary AEF occur after aortic surgery, PAEF are extremely rare. Their poor prognosis is largely due to challenges in diagnosis and low clinical suspicion. Case_presentationWe describe the case of an 83-year-old male, who presented with hematochezia and melena. He had a history of coronary artery disease and anticoagulant use for a prior pulmonary embolism. There was no history of abdominal aortic aneurysm (AAA). Gastroscopy revealed no clear bleeding source, but a hemostatic clip was applied for suspected angiodysplasia. Six days later, another episode of melena occurred. CT angiography subsequently revealed an undiagnosed infrarenal AAA in direct contact with a duodenal diverticulum, raising high suspicion of an aorto-enteric fistula (Figure 1). Therefore we decided for surgical exploration. During surgery, an aorto-duodenal fistula was confirmed between the fourth part of the duodenum and the aortic aneurysm (Figure 2). Infrarenal clamping was possible prior to further dissection of the duodenum showing a clear connection between the aortic aneurysm and the intestinal lumen. The aortic aneurysm was repaired using a self-made bovine pericardium tube graft and a transverse seromuscular suture of the duodenum. We used a transmesocolic omental flap to cover the vascular reconstruction. The patient recovered well. Tissue biopsy identified Lactococcus lactis and Streptococcus mitis / oralis. Consequently, antibiotic treatment was continued according to the regimen for graft infection, with a treatment duration of 6 months. ConclusionClinicians should remain aware of aorto-enteric fistula, particularly in elderly patients presenting with obscure gastrointestinal bleeding, regardless of the presence of a known AAA. 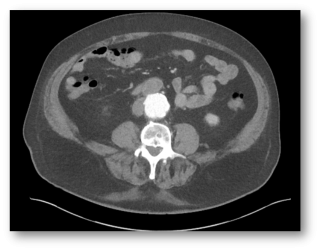
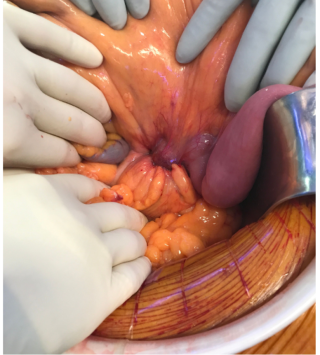
|
||
|
16:30–16:36
Intraoperative Physician-Modification of an Iliac Limb with One Fenestration for the Lower Right Renal Artery as a Rescue Measure for Falsely Planned FEVAR
Konstantinos Kotopoulos, 3010 / Bern
AbstractBackgroundCustom-made fenestrated grafts (FEVAR) became standard approach for treating juxtarenal aortic aneurysms. Although the production time can stretch up to four months, the biggest benefit of the customization is it`s adjustment to patient`s anatomy. Physician-made fenestrated endografts (PMEG) evolved over time to accommodate various anatomies, especially in an emergency setting. We present a case treated with a custom-made 4x FEVAR and one physician-modified iliac limb to accommodate the lower right renal artery (RRA). Case_presentationWe present a 77-year-old male with open surgical repair in 2014 using a tube graft for juxtarenal aortic aneurysm (60mm). Eight years later, a follow-up CT scan revealed two anastomotic aneurysms (proximal 54mm) and distal (69mm). A 4x custom-made-FEVAR was planned based on the CT scan merged from two scans, a thoracic and an abdominal one. Both, the planning and the implantation site have overseen a lower RRA, equally large (5mm) as the upper RRA, thus manufacturing a 4x instead of 5x custom-made FEVAR. We proceeded with implanting the custom-made FEVAR while simultaneously preparing a physician-modified right iliac limb (Endurant II, 13/13/82mm) to preserve the lower RRA. After 4xFEVAR completion, right iliac limb PMEG was advanced, and the target vessel was catheterized and preserved with bridging stents via ipsilateral femoral approach. The final angiography revealed complete exclusion of the aneurysm, without type I or III endoleaks, and adequate position of all bridging stents. Two-year follow-up CT scan demonstrated patent bridging stents without endoleak and completely excluded aneurysm. ConclusionThis case emphasizes the importance of adaptability in complex aortic endovascular procedures. Initially planned as a 4-fenestrated FEVAR, the procedure was modified to include a surgeon-modified iliac limb to accommodate the second right renal artery, ensuring renal perfusion and, therefore, improving the outcome of the patients. 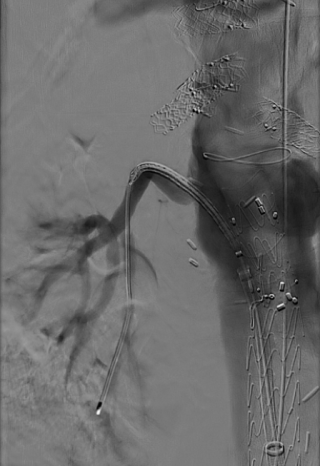

|
||
|
16:40–16:46
Rapid Sac Shrinkage after EVAR
Vanessa Sanchez, Winterthur
AbstractBackgroundVascular endograft infection is a rare but severe postoperative complication of EVAR. This may be complicated by enteric fistulation. Its pathogenesis remains unclear up to this date. Case_presentationThis case reports of an 81y old male patient 4 months after endovascular aortic repair of an asymptomatic 5.5 cm abdominal aortic aneurysm presenting with fever and elevated CRP of 160mg/l. Blood cultures revealed Parvimonas micra, frequently found in patients with chronic periodontitis. A CT scan showed peri-graft air and significant aneurysm sac shrinkage to 3.5 cm. Due to peri-graft air, fever, abnormally elevated inflammatory markers, and positive blood cultures, a vascular endograft infection was diagnosed according to the MAGIC criteria. Additionally, due to the air and the extraordinarily rapid sac shrinkage (from 5.5 cm to 3.5 cm in 4 months) an aortoduodenal fistulation was postulated. Esophagogastroduodenoscopy did not show a bowel wall defect. An aortoduodenal fistula was confirmed intraoperatively. Open surgical repair consisting of complete graft explantation, in situ reconstruction with a physician made xenopericardial graft and closure of the duodenal fistulation, debridement and omentoplasty was performed. The patient died on postoperative day 25 due to bowel ischemia. ConclusionA secondary aortoduodenal fistula represents a life threatening complication. Open surgery including the above-mentioned steps is recommended for curative treatment. An extraordinarily rapid sac shrinkage may be a sign of fistulation. The role of routine examination of dental status prior to aortic surgery is unclear. 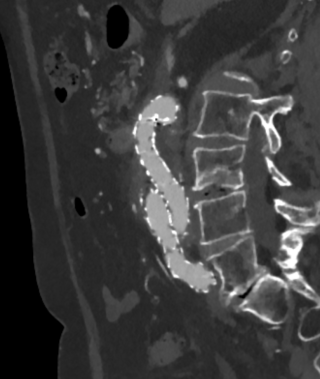
|
||
|
15:30 – 17:00
Room 1B
|
State of the Art in General Surgery - Tips and Tricks
Stephanie Taha-Mehlitz, Basel; Dimitri Christoforidis, Lugano
|
|
|
Main Session
|
||
|
15:30–15:45
Appendectomy
Alexis Litchinko, Fribourg
|
||
|
15:45–16:00
Cholecystectomy
Vanessa Banz, Bern
|
||
|
16:00–16:15
Inguinal hernia repair
Philipp Kirchhoff, Basel
|
||
|
16:15–16:30
Incisional hernia repair
Andrea Donadini, Lugano
|
||
|
16:30–16:45
Subcutaneous port implantation
Florian Dick, St.Gallen
|
||
|
15:30 – 17:00
Auditorium B
|
Ten hot topics in six minutes
Frédéric Ris, Geneva; Beat Schnüriger, Bern
|
|
|
Main Session
|
||
|
15:30–15:36
Surgical therapy for postpartal rectus diasthasis - is there a benefit/ which technique?
Andrea Donadini, Lugano
|
||
|
15:39–15:45
D3 Dissection for all right sided colon cancer?
Matthias Turina, Zurich
|
||
|
15:48–15:54
Where does outpatient management of diverticulitis stand?
Fabian Grass, Lausanne
|
||
|
15:57–16:03
Timing of cholecystectomy after cholecystitis- all clear?
Alessandra Cristaudi, Lugano
|
||
|
16:06–16:12
What to do with esophageal dysmotility and hiatal hernia?
Stefan Mönig, Geneva
|
||
|
16:15–16:21
What to do with normocalcemic hyperparathyroidism?
Valentine Luzuy-Guarnero, Geneva
|
||
|
16:24–16:30
Indications to go forward with surgery in MACS
Corina Kim-Fuchs, Bern
|
||
|
16:33–16:39
Bariatrics - what are the ideal limb lengths?
Ralph Peterli, Basel
|
||
|
16:42–16:48
Robotic kidney transplantation - where is its role?
José Oberholzer, Zurich
|
||
|
16:51–16:57
Using resorbable mesh for hiatoplasty - is it better than nothing?
Yves M. Borbély, Bern
|
||
|
16:45 – 18:15
Room 5A
|
Guardians of the Scalpel: Securing Excellence in the Treatment of Stage III Non Small Cell Lung Cancer - Main Session 2
Patrick Dorn, Bern; Isabelle Opitz, Zurich
|
|
|
Guardians of the Scalpel
|
||
|
16:45–17:05
Minimal invasive surgery offers the best chance of cure
Thorsten Krueger, Lausanne
|
||
|
17:05–17:25
Many ways to Rome: open surgery is not extinct (yet)
Tamas Molnar F, Pécs HU
|
||
|
17:35–17:50
Comprehensive staging and diagnostic strategies for stage III NSCLCThe pathologist's perspective: challenges in accurate staging
Sabina Berezowska, Lausanne
|
||
|
17:55–18:10
Comprehensive staging and diagnostic strategies for stage III NSCLCAdvanced PET/CT imaging: Enhancing diagnostic precision
Niklaus Schäfer, Lausanne
|
||
|
From 18:00
|
Surgeons' NightMusée Olympique |
|
|
Social Program
|
We are delighted to invite you to the SCS Surgeons’ Night 2025 in Lausanne, an evening of celebration, inspiration, and camaraderie. The event takes place at the stunning Olympic Museum, where we’ll immerse ourselves in the rich history of both the ancient and modern Olympic Games.
18:00: The Olympic Museum opens its doors exclusively to guests of the Surgeons’ Night. Step into the world of Olympism and let the spirit of the Games inspire you as you explore fascinating exhibits and remarkable stories from Olympic history. 19:00: We warmly invite you to join us for a Welcome Drink. Enjoy light refreshments and a selection of snacks, and take the opportunity to connect with fellow participants. 20:15: We will have the honor of presenting the awards to this year’s winners. With great pride and applause, we will recognize their outstanding achievements — “Honor to whom honor is due.“ 20:30: Indulge in a delicious Seated and Standing Dinner, accompanied by breathtaking views of Lake Geneva. Take this opportunity to engage in stimulating conversations with colleagues, all while enjoying a culinary experience that promises to delight your senses. As the night continues, get ready for an unforgettable party. The DJ will take the stage, spinning the perfect mix of songs and beats to keep the energy high and the dance floor moving well into the early hours. We look forward to sharing this special evening with you. It promises to be a memorable night of celebration, inspiration, and fun. |