Visual Poster SCS – Swiss College of Surgeons Annual Meeting 2025
The Visual Abstracts are displayed in the room «Foyer Garden».
All authors are kindly asked to put the Visual Abstracts on display on Thursday morning, May 22nd
and be present during the poster walk on Friday, May 23rd, from 12h30 to 14h00, to answer questions from interested colleagues.
Visual Abstracts
|
08:00 – 17:00
Foyer Garden
|
Visual Abstracts |
|
|
PSGC1
Magnetic resonance imaging versus 18F-FDG-PET/CT in the detection of tuberculous spondylodiscitis: Results from the Spinal TB X cohort
Julian Scherer, Zurich / Cape Town
AbstractBackgroundMagnetic resonance imaging (MRI) is the current imaging gold standard for the radiological assessment of tuberculous spondylodiscitis, with good sensitivity and. Recently, a study showed that 18F-Fluorodeoxyglucose Positron Emission Tomography-computed Tomography (PET/CT), as a whole-body imaging modality, may produce comparable sensitivity but a better specificity than MRI in the detection of spondylodiscitis. AimsIn this preliminary analysis we assessed and compared the detection of lesions and the number of diseased vertebras per lesion caused by Mycobacterium tuberculosis between the two imaging modalities in 25 patients with confirmed spinal tuberculosis (STB). MethodsThe Spinal TB X cohort is an ongoing prospective cohort study describing the clinical phenotype of spinal TB using whole-body 18FDG-PET/CT (PET/CT) and whole-spine MRI at baseline with repeated PET/CT at six- and 12-months to monitor treatment respond. Results31 patients were enrolled and underwent both MRI and PET/CT. 25 patients had microbiologically confirmed STB (56% male, 44% HIV-infected, median age 47 years, IQR 23). Spinal skip lesions were detected by PET/CT in five patients (80% HIV-uninfected) whereas MRI detected spinal skip lesions in only one patient (p=0.02). Psoas abscess formation was detected by PET/CT in 16 patients (MRI 14 patients). The mean lesion count per patient was 1.3 (SD 0.6) on PET/CT and 1.1 (SD 0.4) on MRI. (Shapiro-Wilk<0.001, p=0.096). PET/CT identified an average of 3.3 diseased vertebras per lesion (SD 1.3), whereas MRI detected an average of 2.4 (SD 0.6) diseased vertebras per lesion. (Shapiro-Wilk<0.001, p=0.052). ConclusionIn our findings, we had a higher rate of lesion detection using PET/CT including spinal skip lesions, compared to the current imaging gold standard. Further, more diseased vertebras per lesions were detected by PET/CT compared to MRI. PET/CT might be an advantageous imaging modality to quantify the extent of disease in patients with STB. With increasing sample size, we aim to confirm these findings. |
||
|
PSGC2
Correlation between inflammatory markers on whole-body 18F-FDG-PET/CT and quality of life in Spinal Tuberculosis: Insights from the Spinal TB X Cohort Study
Julian Scherer, Zurich / Cape Town
AbstractBackgroundWhole-body 18FDG-PET/CT (PET/CT) in spinal tuberculosis (STB) can detect disseminated disease and allows monitoring of treatment response. We are conducting the Spinal TB X cohort study at the University of Cape Town including serial PET/CT imaging. AimsThe aim of this analysis was to assess the correlation between inflammatory markers and quality of life during the 12 months of treatments. MethodsWe assessed the total lesion glycolysis (TLG), C-reactive protein (CRP), pain visual analogue scale (pVAS), Oswestry Disability Index (ODI) and EQ-5D-5L values in patients diagnosed with STB, at baseline PET/CTBL and 12 months end-of-treatment PET/CTEND. Decrease over time and correlations between the assessed parameters were analysed using repeated measures ANOVA and Pearson’s correlation (r). ResultsWe analysed 10 patients (median age 43.5 years, 30% female, 30% HIV-infected) with 14 spinal lesions. The median TB treatment duration at PET/CTEND was 51 weeks; one patient received MDR treatment. The mean TLG of all lesions decreased from 343.8 (PET/CTBL) to 33.1 (PET/CTEND), p=0.017. Persistent 18FDG uptake at PET/CTEND was observed in 3/14 spinal lesions. The mean CRP decreased from 54.5 to 5.4 mg/L (p=0.112); pVAS from 6.7 to 0.5 (p<0.001); ODI from 27.2 to 2.9 (p<0.001); and EQ-5D-5L from 14.9 to 5.8 (p<0.001). (Figure 1) The decrease in CRP (r=0.683, p<0.001), pVAS (r=0.659, p<0.001), ODI (r=0.666, p<0.001), and EQ-5D-5L (r=0.601, p=0.005) correlated significantly with the decrease of TLG over time. At PET/CTEND, nine patients were pain-free (pVAS 0) and had an EQ-5D-5L of 5 and five patients had an ODI of 0. ConclusionClinical improvement at end of 12 months of TB treatment correlates with decrease in spinal inflammation. PET/CT can monitor treatment response in our cohort. The majority of patients had no persisting morbidity at the end of treatment 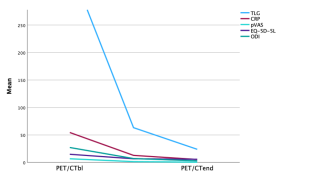
|
||
|
PSGC3
Patient-Derived Tumoroid Xenograft Models for Preclinical Validation of Therapeutics for Pleural Mesothelioma
Tamas Vancsik, Zürich
AbstractBackgroundPleural mesothelioma (PM) is a highly heterogeneous and aggressive cancer with limited therapeutic options. To advance personalized treatments, patient-derived tumoroid cultures that preserve the morphological and molecular characteristics of their original tumors across the epithelioid-sarcomatoid spectrum were established. High-throughput screening of these tumoroids with 3,000 FDA-approved compounds identified both common and patient-specific targets. AimsHere, we conducted in vivo studies to validate the efficacy of promising therapeutic candidates using optimized tumoroid xenograft models. MethodsWe developed orthotopic intrapleural and subcutaneous xenograft models using PM050 PM tumoroid cell line, which represents biphasic characteristics and engineered to express fluorescent and bioluminescent markers for non-invasive monitoring of disease progression. Injection parameters were optimized to achieve reproducible tumor growth kinetics. Pilot studies evaluated the therapeutic effects of romidepsin, a histone deacetylase inhibitor, and sepantronium bromide, a survivin inhibitor, in comparison to cisplatin-pemetrexed, the current standard of care. Tumor growth and drug efficacy were monitored through imaging and confirmed by histological analysis. ResultsBoth orthotopic and subcutaneous models produced detectable tumor phenotypes with growth kinetics correlating to the cell number injected. Subcutaneous grafts developed visible macroscopic tumors, while intrapleural grafts demonstrated diffuse growth patterns. Histological analysis confirmed that xenografts retained the expression of key PM markers including negative calretinin and positive vimentin, consistent with in vitro tumoroids and the original tumor tissue. No significant tumor size reduction was observed with therapeutic intervention with cisplatin-pemetrexed or romidepsin, whereas sepantronium bromide exhibited a trend toward tumor growth attenuation, though variability warrants further study. ConclusionOur findings demonstrate the feasibility of tumoroid-based xenograft models for preclinical validation of PM therapies. The models accurately reflect disease heterogeneity and provide a robust platform for testing novel drugs. These initial results highlight the potential of targeting survivin with sepantronium bromide. Further studies to confirm the therapeutic potential of sepantronium bromide are ongoing. |
||
|
PSGC5
Evaluation of the Competency Evolution of Trainees With a Thoracic Surgery Simulation Program Using the Kirkpatrick Model
Edoardo Zanfrini, Lausanne
AbstractBackgroundMinimal invasive thoracic surgery has become standard, however, teaching this technique remains challenging. There are several frameworks to guide program directors in designing a fit-for-purpose curriculum. AimsWe evaluated how our simulation program improved trainee skill, knowledge, and behavior, in the context of practice-based leaning using the Kirkpatrick model. MethodsWe developed a video-assisted thoracic surgery training program on a simulator (J&J Stupnik® V3.2) to teach right lung segment resections throughout training. Our paradigmatic approach is post-positivistic, and we used the Kirkpatrick model to inform us on different aspects of training: reaction (level 1), learning (level 2), and behavior (level 3). All our residents were included in the program. We preliminarily evaluated results after 7 months of segment 6 resections for trainees that participated in 3 or more sessions (n=3) using a multiple-choice test (MCQ), given before and after the training. This evaluated knowledge of anatomy, sequence, and technical aspects of the task. A feed-back survey using the Likert scale probed participant satisfaction. Additionally, skills were observed by senior staff surgeons, documenting time to task completion and number of mistakes. Finally, we conducted informal interviews with faculty to inform us on trainee progression in the operating room (OR). ResultsAfter the observation period we noted a 10% increase in MCQ results, a 35% decrease in task completion time, and in the number of mistakes (28% for minor mistakes, and 75% for major mistakes). The overall participant satisfaction was high. The informal interviews with faculty members revealed a positive perception of expected trainee behavior during surgery in the OR. ConclusionOur preliminary results show that the implementation of our simulation program objectively increases the efficacy in task completion of trainees, positively impacting the perception of the learning experience by trainees, and the perception on trainee behavior by faculty. |
||
|
PSGC6
The role of indigenous healers in treating surgical conditions in the rural Eastern Cape of South Africa
Paolo Rodi, Zurich / Novara
AbstractBackgroundIndigenous knowledge healers (IKHs) provide alternative healthcare to formal health services in rural South Africa, but there is a gap in knowledge regarding their treatment of surgical conditions. AimsThis study evaluated IKH surgical care and described their perspective of the dual health system. MethodsA cross sectional survey of IKHs in the Madwaleni Hospital catchment of the Eastern Cape, South Africa was conducted. Topics included the training and experience of IKHs, treatment of nine common surgical conditions, referral patterns, disease origin beliefs, benefits and limitations of care, and collaborative opportunities between the two health systems. ResultsThirty-five IKHs completed the survey. IKHs were consulted by persons with all nine surgical conditions. The most common forms of treatment were application of an ointment on the affected site (88%) and oral medication (82%). Operative treatment was only done for abscess. Referrals to the formal healthcare sector were made for all surgical conditions. IKHs reported that they were limited by their lack of training and resources to perform operations. On the other hand, they perceived the treatment of the spiritual aspect of surgical disease as a benefit of their care. Thirty-five (100%) IKHs were interested in closer collaboration with the formal health sector. ConclusionIKHs treat surgical conditions but refer to the formal health sector when diagnostic and operative services are needed. More research is needed to determine the potential advantages and disadvantages between the formal health sector and IKH collaboration. |
||
|
PSGC7
Access to Care in Afghanistan: A Mixed-Methods Study Exploring access to emergency, critical and operative care in 11 Afghan provinces
Paolo Rodi, Zurich / Novara
AbstractBackgroundAfghanistan’s health system has been impacted by 4 decades of war. Despite progress in health service coverage through NGO interventions, access to emergency, critical, and operative (ECO) care remains limited. AimsThe aim is to evaluate barriers and facilitators to access to ECO care in 11 provinces in Afghanistan, that impede patients to seek, reach, receive and adhere to adequate emergency and surgical care. Moreover, it aims to identify key gaps and needs in ECO service delivery, assessing the overall timeliness, capacity, safety, accessibility, affordability and availability of ECO care. MethodsThe study uses a mixed-methods approach. Part 1 will involve descriptive analysis of health records from the facilities of the EMERGENCY NGO to identify trends. Part 2 will use questionnaires for patients and staff to explore accessibility, affordability, and availability of ECO care. Part 3 will include semi-structured interviews with health professionals to evaluate service status. Part 4 will employ the WHO Harmonized Health Facility Assessment tool to assess surgical capacity and quality in selected facilities. Data collection and analysis will take place between October 2024 and January 2025. ResultsWe will analyse facilities’ records from 11 provinces, reviewing existing data, collecting approximately 1200 questionnaires, conducting ca. 40 interviews, and quantitatively assessing care capacity of selected health facilities. Data will provide an extensive overview of the universal and equitable access to ECO services in Afghanistan, including the points of view of both beneficiaries and healthcare providers. ConclusionThis study will produce recommendations on how to expand patient access to ECO services in urban and rural areas, to integrate ECO services into essential health packages, to improve coordination among health providers, and to enhance the sustainability and resilience of Afghanistan's health system. |
||
|
PSGC8
Implementation of a 42+4-Hour Workweek in the Surgical Department of our Hospital
Oscar Feusi, Uster
AbstractBackgroundNationwide surveys reveal that residents face immense pressures, with about 60% of working hours spent on administrative tasks, resulting in stress, burnout, and reduced training quality. These conditions compromise resident well-being and lead to dissatisfaction, necessitating structural reforms. Our hospital addressed this by piloting a 42+4-hour workweek with a collaborating association, allocating 42 hours to patient care and 4 hours to structured education. AimsTo present preliminary results from a step-to-step implementation of a 42+4-hour workweek at our surgical department and the evaluation of the feasibility of its transferability to other departments. MethodsThe implementation first involved analyzing the status-quo after which we developed measures to gradually reduce working hours by optimizing workflows through task delegation, expansion of dictation technology and improved schedules. Furthermore, we monitored patient care and surgery numbers to optimize resource management. We revised the daily structure to accommodate a 46-hour weekly schedule, including four hours of structured education. Three months after initiating the 46-hour workweek, we evaluated the first preliminary results and made further adjustments. ResultsAs of August 2024, our department adopted the 42+4-hour workweek. Digital tracking three months after implementation confirmed adherence among 40% of residents despite staff shortages. These shortages made implementation more challenging. The preliminary results show that the average working time of the residents was 47 hours and 14 minutes. Results after six months of implementation are pending. ConclusionThe implementation of the 42+4-hour workweek at our hospital demonstrates its viability in surgical environments. The results after three months show that not all residents could adhere to the 46-hour workweek, but the working hours fell by almost 3 hours from the initial 50-hour workweek. This model shows potential for reducing burnout, enhancing resident satisfaction, and aligning clinical hours with core competencies, serving as an example for broader application. |
||
|
PSGC9
International Validation of the AO Spine Osteoporotic Fracture Classification
Julian Scherer, Zurich / Cape Town
AbstractBackgroundOsteoporosis, a public health concern of progressively escalating significance, imposes a substantial global burden, with the disease's burden having surged by over 110% in recent decades. Vertebral fractures notably emerge as a pivotal concern within the context of osteoporosis, representing the most frequent fragility fractures. AimsThis study aimed to determine the reliability of the AO Spine-DGOU Osteoporotic Fracture Classification System within the framework of a large global, multicentric analysis. MethodsA total of 320 participants with diverse professional backgrounds assessed 27 osteoporotic vertebral fracture cases on two occasions, four weeks apart. Inter-rater and intra-rater reliability were measured using Fleiss' kappa coefficients (κ), analyzing agreement levels in fracture classification among participants and within individuals over time. ResultsThe overall agreement with the gold standard classification was 76% in both assessments. Inter-rater reliability showed moderate agreement (κ = 0.57 in the first assessment and κ = 0.58 in the second). Intra-rater reproducibility was substantial, with a mean κ of 0.66 and a median κ of 0.71. Higher agreement levels were observed for OF 4 and OF 5 fractures, while OF 3 fractures exhibited lower agreement. ConclusionThe AO Spine-DGOU Osteoporotic Fracture Classification System demonstrates moderate to substantial reliability in an international multicenter context. These findings support its utility as a standardized tool for classifying osteoporotic vertebral fractures, potentially enhancing communication and decision-making in clinical practice. |
||
|
PSGC10
Validation of the AO Spine Osteoporotic Fracture Classification – Effect of geographical region on reliability and reproducibility
Julian Scherer, Zurich / Cape Town
AbstractBackgroundOsteoporosis is a widespread disease with an increasing incidence. In 2018, the “Osteoporotic Fracture working group” affiliated with the German Society for Orthopaedic and Trauma Surgery (DGOU), introduced a novel classification system specifically for osteoporotic thoracolumbar vertebral body fractures. AimsTo evaluate the influence of geographic region on the reliability and reproducibility of the AO Spine-DGOU Osteoporotic Fracture Classification System. MethodsThis study included 320 participants from various global regions who classified 27 cases of osteoporotic vertebral fractures using the AO Spine-DGOU system which categorizes the fractures to 5 subtypes (OF 1 – OF 5). Participants underwent training via an online webinar. Interobserver reliability and intraobserver reproducibility were assessed using Fleiss' kappa coefficient, and agreement with a gold-standard committee was evaluated. ResultsThe classification system showed moderate to substantial agreement with the gold standard globally (initial kappa 0.58, improving to 0.61). European participants had the highest agreement (kappa 0.64 and 0.66). OF4 fractures were most accurately classified, while OF3 fractures showed the least agreement. Intraobserver reliability was highest among European participants. Post-hoc analysis indicated significantly better reliability among German-speaking participants compared to other Europeans (kappa 0.79 vs. 0.70, p=0.0026). ConclusionThe AO Spine-DGOU Osteoporotic Fracture Classification System demonstrates moderate to substantial reliability and reproducibility, with regional differences influenced by factors such as training and clinical experience. This underlines the necessity of proper education adapted to the regional particularities. |
||
|
PSGC11
Primary Stability of Nailing Versus Low Profile Dual Plating of Mid-Clavicular Fractures – a Biomechanical Study
Fabian Pretz, Luzern / Lucerne
AbstractBackgroundLow-profile dual plating techniques have gained popularity for diaphyseal fractures due to their potential to reduce soft tissue irritation, thus decreasing the likelihood of implant removal. However, it has not yet been biomechanically investigated whether 2x2.0mm dual plating achieves stabilization comparable to a titanium elastic nail for clavicle midshaft fracture fixation.
AimsTherefore, the aim of the current study was to compare the biomechanical properties of 2x2.0mm low-profile matrix mandible plates with a 2.5mm TEN (Titanium Elastic Nail) in a human cadaver model to evaluate the biomechanical stability of these two methods. MethodsTwelve paired human cadaveric clavicles with simulated unstable diaphyseal shaft fractures (AO 15.2C) were stabilized with either an intramedullary nail (Group 1) or a combination of a superior and an anterior 2.0mm matrix mandible plate (Group 2). Specimens underwent initial quasistatic pure bending in superior-inferior and anterior-posterior direction, followed by cyclic superior-inferior load to failure. Interfragmentary movements were monitored by optical motion tracking. ResultsDual plating demonstrated significantly higher initial construct stiffness in all bending directions and a reduced neutral zone compared to TEN nailing. In addition, fracture displacement amplitudes over all cycles were significantly higher in Group 1 versus Group 2 (p = 0.002). The number of cycles to reach the test endpoint did not differ significantly between the groups (p = 0.16), with Group 1 averaging 24,420 cycles (SD ±3,614.65) and Group 2 averaging 28,232 cycles (SD ±5,417.13). ConclusionIn selected patients with simpler unstable midshaft clavicle fractures, 2x2.0mm dual plating may offer effective biomechanical stability. However, large-gap C-type fractures remain too unstable for these methods, emphasizing the need for further research to refine indications and assess long-term outcomes. 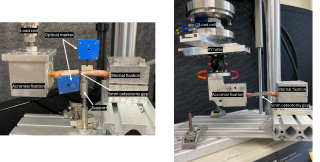
|
||
|
PSGC12
Biomechanical Comparison of Augmented MIPO Versus ORIF Locking Plate Fixation in Proximal Humerus Fractures With Low Bone Mineral Density
Fabian Pretz, Luzern / Lucerne
AbstractBackgroundProximal humerus fractures are common in patients with low bone mineral density. Locking plate osteosynthesis using either MIPO or ORIF technique is widely performed. AimsComparison of biomechanical stability between four cemented humeral head screws in PHILOS plates (MIPO) and six non-cemented head screws with two additional calcar screws (ORIF). Hypothesis: Screw tip augmentation offsets MIPO's reduced stability, resulting in no group differences. MethodsFourteen paired human cadaveric humeri with simulated unstable three-part proximal humerus fractures (AO 21 11-B1) were stabilized using PHILOS plates with four proximal head screws in both groups (row A and B). In the ORIF group, two additional calcar screws were used (row E) while in the MIPO group, the four screw tips were augmented with bone cement. Cyclic axial loading tests were conducted until failure and interfragmentary movements were monitored. ResultsInitial axial construct stiffness and cycles to failure showed no significant differences between groups (p=0.171, 27 p=0.397). Under increasing cyclic loading, the ORIF group exhibited a significant increase in varus deformation (p=0.029), head displacement (p=0.038), and screw bending in row A (p=0.003), whereas no significant increase in these parameters was observed in the MIPO group. Although the overall values were higher in the MIPO group, there was no significant difference in absolute values between the groups (p=0.071). ConclusionFrom a biomechanical perspective PHILOS plates with four augmented screws as used in the MIPO technique demonstrated comparable initial construct stability and cycles to failure as compared to the commonly used PHILOS plates with additional calcar screws as used in the ORIF technique. Moreover, the ORIF group exhibited significantly greater increases in varus deformation and humeral head displacement under cyclic loading, while the MIPO group, despite higher overall values, showed no significant increase. This suggests that the MIPO technique may be a valid alternative to the ORIF technique, particularly in the context of low bone mineral density. 
|
||
|
PSGC13
Evaluating the Biomechanical Efficacy of 2.5+2.0 Double Plating Against 3.5 Single Plating in Ulna Shaft Fracture Fixation: A Cadaveric Study
Moritz Kraus, Zurich / Davos
AbstractBackgroundThe main complications after ulna shaft fracture fixation are non-union and implant irritation. Standard 3.5-mm locking compression plates can cause soft tissue irritation, often requiring implant removal. Using two smaller orthogonal plates has been proposed as an alternative to address these issues. AimsThe aim of this study is to compare the biomechanical properties of a single 3.5-mm locking compression plate versus double-plating using one 2.5-mm and one 2.0-mm matrix mandible plate in a human ulna shaft fracture model. MethodsEight pairs human ulnar specimens with a standardized 10 mm comminuted fracture gap were pairwise assigned for instrumentation with either double plating using a 2.5-mm and a 2.0-mm mandible plate placed posteriorly under the flexor muscles and laterally under the extensor muscles, or with a single 3.5-mm plate placed posteriorly. All constructs underwent biomechanical testing for axial, torsional, and bending stiffness, which was followed by cyclic torsional loading to failure. Interfragmentary movements were monitored by means of optical motion tracking. ResultsThere were no significant differences between double-plating and single-plating techniques in axial stiffness (464.6±424.0 N/mm vs. 754.2±575.2 N/mm; p=0.335), torsional stiffness in supination (0.330±0.072 Nm/° vs. 0.403±0.066 Nm/°; p=0.462) or pronation (0.330±0.071 Nm/° vs. 0.406±0.068 Nm/°; p=0.307), medio-lateral bending stiffness (1.40±0.61 Nm/° vs. 0.97±0.45 Nm/°; p=0.522), and antero-posterior bending stiffness (0.80±0.01 Nm/° vs. 0.85±0.18 Nm/°; p=0.143). Double-plating showed a higher angular displacement rate during cyclic torsional loading (p=0.03), but no significant difference in shear displacement across the fracture gap (p=0.324). Cycles until failure (5° angular deformation) were 1366±685 for double-plating and 2024±958 for single plating. Both constructs failed due to bone breakage at the most distal screw. ConclusionThe double-plate construct provides comparable fixation to single plating, with similar stiffness and shear displacement. Clinical trials are needed to confirm if thinner implants reduce irritation and removal rates. |
||
|
PSGC14
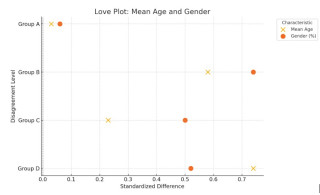
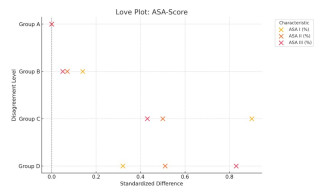
Clinical equipoise as inclusion criterion to control for confounding in natural experiments
Niels van der Hoeven, Oegstgeest NL / Luzern NL / Leiden NL
AbstractBackgroundObservational studies are increasingly recognized as a valuable complement to RCTs in orthopedic trauma surgery. However, the absence of randomization in observational studies can lead to a lack of comparability between treatment groups, resulting in confounding bias. A potential solution is the use of natural experiments, where treatment allocation is determined by factors beyond the investigators' control, resembling experimental randomization. To further reduce confounding, "clinical equipoise" can be used as an inclusion criterion, restricting the study population to patients for whom surgeons disagree on the preferred treatment, thereby improving group comparability. AimsThe aim of this study is to assess how the degree of disagreement among surgeons influences the comparability of treatment groups in a natural experiment using clinical equipoise. MethodsThis retrospective analysis is based on the LADON Humerus study, a multicenter, prospective study comparing operative versus non-operative treatment for acute displaced proximal humerus fractures. Patients from the Netherlands and Switzerland were assessed by independent panels of surgeons from the other country, blinded to actual treatments. Inclusion was limited to cases with significant disagreement between the treatment received and surgeons’ recommendations, enabling classification into four levels of disagreement. Standardized differences were calculated to evaluate the distribution of baseline characteristics (age, gender, AO classification, ASA score) between groups, with results visualized using love plots. ResultsIncreasing levels of disagreement were associated with decreasing standardized differences, leading to improved baseline balance across most characteristics, particularly gender, age, and ASA score. ConclusionNatural experiments using clinical equipoise offer a promising approach to mitigate confounding bias in observational studies. This study demonstrates that leveraging disagreement among surgeons enhances comparability between treatment groups, supporting further exploration of this method in future research. 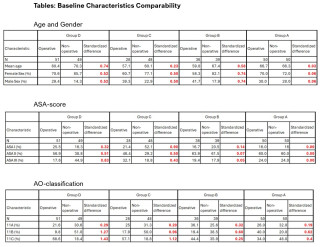
|
||
|
PSGC15
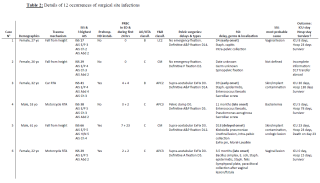
Operatively treated high-energy blunt pelvic ring injuries and surgical site infections – a retrospective assessment based on a prospective registry.
Elvin Gurbanov, Geneva
AbstractBackgroundHigh-energy pelvic ring injuries (PRI) are severe, life-threatening trauma conditions which might require complex surgical management. One of the major complications associated with these injuries is the development of surgical site infections (SSI) which significantly impact patient outcomes. AimsThis study aimed to evaluate the rate of SSI in patients undergoing surgical fixation of high-energy blunt PRI and identify the key predisposing factors. MethodsA retrospective review of patients treated for high-energy blunt PRI was conducted using the prospectively filled institutional Severely Injured Patients’ Registry, focusing on the rate of SSI following surgical fixation. The multifactorial nature of infection risk was analyzed, with particular attention to the type of injury, surgical technique, external fixation devices’ usage and the germs encountered. ResultsA SSI rate of 10,5% (12 out of 114 patients) was encountered among the study population. The primary SSI risk factor was PRI complexity; 83.3% of patients with SSI had an AO/OTA type C fracture and 16.7% a type B fracture, while 43.1% of patients without SSI had a type C fracture and 56.9% a type B fracture (p=0.008). Additionally, SSI patients had a trend to have higher extremities/pelvis AIS and higher ISS, and to have been more often treated with a transient pelvic fixation device including supra-acetabular external fixator. ConclusionThese findings emphasize the need for a comprehensive infection prevention strategy in high-energy PRI patients, especially in complex cases. A multidisciplinary approach is of outmost importance and should include surgical techniques with meticulous soft tissue handling, proper implant selection and aggressive post-operative wound care. Despite external fixation devices being related to certain cases of SSI, their life-saving potential during the initial management phase should be carefully weighed against this risk. 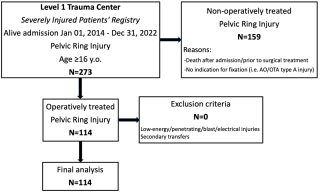
|
||
|
PSGC16
Increased use of Whole-Body-Computed-Tomography in “Non-Emergency-Resuscitation-Room” patients after trauma: indications, findings and therapeutic consequences
Etrit Gashi, Aarau
AbstractBackgroundThe Whole-Body-Computed-Tomography (WBCT) is an essential adjunct in diagnosing and treating polytrauma patients and has been shown to improve survival prognosis. Since its introduction in the emergency department the use of it exponential increased over the years, while lacking on well-defined indication-protocols for “Non-Emergency-Resuscitation-Room” patients. AimsThe aim of the present study was to analyze the role of WBCT in trauma patients in a “Non-Emergency-Resuscitation-Room” setting. MethodsRetrospective analysis of all patients admitted to our emergency department between 01/2019 and 12/2021 who received WBCT in a “Non-Emergency-Resuscitation-Room” setting. Indications for WBCTs, specific injuries and therapeutic consequences were investigated. ResultsDuring the three-year study period, a total of 504 WBCTs were performed in “Non-Emergency-Resuscitation-Room” patients. The number of WBCTs increased significantly (p<0.001) over the years as follows: 2019: n=78 (2.5% of all emergency room patients); 2020: n=91 (3.2%); 2021: n=335 (11.3%). The most common indications for WBCTs were high-energy trauma (n=228, 45.2%) and suspected multiple injuries on clinical examination (n=190, 37.7%). Overall, one or more injuries were detected in 56.7% of WBCT scans (n=286). The injuries detected included thoracic trauma (n=155, 30.8%), head injuries (n=111, 22.0%), spinal fractures (n=95, 18.8%), intra-abdominal organ injuries (n=63, 12.5%), pelvic fractures (n=27, 5.4%), vascular injuries (n=24, 4.8%) and extremity fractures (n=12, 2.4%). Based on the results of the WBCTs, surgical or interventional radiologic procedures were required in 15.3% of cases (n=77), which mainly included spinal injuries (n=16) and thoracic injuries (n=8). ConclusionThe use of WBCTs has increased significantly and has become an integral part of our diagnostic algorithm for traumatology patients even in “Non-Emergency-Resuscitation-Room” settings. However, clear indication-protocols or -algorithms are required to avoid unnecessary radiation exposure. |
||
|
PSGC17
Pelvic ring fracture and erectile dysfunction (PERFECD) – 3 year follow-up cross sectional study
Sascha Halvachizadeh, Zurich
AbstractBackgroundPelvic ring fractures are associated with complications that may involve adjacent organs, often presenting in a delayed manner. AimsThis study evaluates the quality of life (QoL) and erectile dysfunction (ED) in patients with pelvic ring fractures at least three years post-injury. MethodsBetween January 2016 and December 2020, male patients (≥18 years) with pelvic ring injuries were included. Fractures were classified using the Young & Burgess system, and pelvic contusions served as a control group. Data were collected through a questionnaire assessing QoL via the Short Form 12 (SF-12) and ED using the International Index of Erectile Function 5 (IIEF-5). ED was categorized as no ED (21-25 points), mild (16-21), moderate (9-15), or severe (5-7). Comorbidities such as vasculopathy, diabetes, and smoking were also considered. ResultsA total of 182 patients participated, with a mean injury age of 53.5 years and an average age of 57.8 at the time of the survey. Patient distribution was: APC (n = 20, 11.1%), LC (n = 94, 52.2%), CMVS (n = 6, 3.3%), and Control (n = 60, 33.3%). The mean Injury Severity Score (ISS) was 24.6. ED was reported in 82.6% of patients, with 47.8% experiencing severe ED. Patients with CMVS fractures had significantly lower QoL scores, especially in physical function. APC injuries were an independent risk factor for ED (OR -4.5, p = 0.02), similar to risk factors such as diabetes (OR -5.3, p = 0.012) and smoking (OR -2.6, p = 0.05). ConclusionVertical shear fractures result in lower QoL three years post-injury. APC fractures were a significant risk factor for ED, highlighting the need for early screening and intervention in these patients. |
||
|
PSGC18
Metabolomics after polytrauma – A biobank analysis of 97 patients over the time course of 10 days
Michel Teuben, Zurich / Zürich
AbstractBackgroundSevere injury is known to have systemic effects at multiple levels, with the inflammatory response being a major focus of research in recent years. However, little is known about the perturbation of metabolic pathways after polytrauma. AimsTo investigate metabolite dynamics and injury specific pattern, we performed a metabolomic analysis of patients from our in-hospital polytrauma biobank, which contains up to ten days of samples from each patient. MethodsPatients from the in-house polytrauma biobank with signed ethical consent were utilized. Sample time points were baseline (hospital admission), 8h, 24h, 48h, 5d and 10 days post trauma. Untargeted mass spectrometry was performed, while metabolites reliably identified using the KEGG/HMDB database were subset-analyzed in a semitargeted approach. Metabolic changes were identified using MetaboAnalyst 6.0 to detect pathways that were particularly affected and presented using enrichment ratios. Additionally, cluster analyses were performed and metabolite dynamics over time were assessed. Results97 severely injured patients (79.4% male / 20.6% female) were included in the study. The median ISS of this cohort was 29 (IQR=19). 46 metabolites were reliably identified. The immediate response (0-8h) shows increased activation of hemostasis and inflammation along with excessive corticosteroid production. In the 8-24h period, there is an excessive catabolic state with energy mobilization from fatty and amino acids. At 24-48 hours, detoxification, immune regulation and metabolic adjustments are primarily active. In the 5-10 day period, energy requirements are still elevated but reduced compared to the previous time points. ConclusionSevere trauma causes a major disruption in the metabolism. Immediately after trauma, the body activates life-saving pathways and begins to mobilize excessive energy resources by breaking down fats and amino acids for ATP production. Initial treatment and intensive care should take this excessive energy demand into account and assess the extent to which organ-protective treatment (e.g. liver) may be beneficial to the patient. |
||
|
PSGC19
Comparative Analysis of Pretension Maintenance in Suture Tape Cerclage and the Influence of intense Cyclic Loading
Moritz Kraus, Zurich / Davos
AbstractBackgroundFiber tapes have largely replaced steel wire cerclages in treating periprosthetic humerus fractures due to reduced soft tissue injury. However, their ability to maintain initial pre-tension under dynamic loading is insufficiently studied. AimsThis study compares the pre-tension retention of DYNATape (DT) and SutureTape (ST) and evaluates their biomechanical performance in stabilizing humeral shaft fractures. MethodsCortical bone shells from human humeri were stabilized with fiber tape cerclages (Group 1: DT; Group 2: ST) and subjected to standardized biomechanical testing. Tapes were wrapped twice around the bone and secured with a modified Nice-Knot at 30 N pre-tension. The setup was submerged in a 36°C saline bath. The protocol included two 8-hour rest phases (R1, R2), cyclic loading from 30 N to 400 N over 10,000 cycles at 3 Hz (B1), and cyclic loading to failure up to 700 N (B2). Load, displacement, and cycles to failure were recorded, and failure modes analyzed. ResultsBoth groups showed comparable initial pre-tension (DT: 35.5 ± 4.2 N; ST: 28.4 ± 6.2 N; p = 0.06). DT had significantly higher maximum pre-tension after R1 (52 ± 8 N vs. 29 ± 6 N; p < 0.001) and R2 (29 ± 8 N vs. 14 ± 7 N; p = 0.008). Retained pre-tension after B1 was higher for DT (20 ± 7 N vs. 9 ± 6 N; p = 0.012). Failure occurred consistently due to tape rupture near the knot, with no differences in displacement or cycles to failure (p > 0.3). ConclusionDYNATape demonstrated superior pre-tension retention and post-loading retensioning compared to SutureTape, potentially improving stability and fracture compression. Both tapes exhibited similar failure modes. Further studies should explore the clinical implications of these findings. |
||
|
PSGC20
Operative vs. Nonoperative Treatment in Mason Type II Fractures: A Meta-Analysis
Christian Goy, Luzern / Lucerne
AbstractBackgroundIt is unclear whether patients benefit from operative treatment in Mason type II radial head fractures. AimsThis meta-analysis aims to compare the two treatment modalities regarding functional outcomes, complications, and quality of life. MethodsA systematic search of PubMed, Embase, and the Cochrane Central Register of Controlled Trials was conducted for randomized controlled trials and observational studies comparing operative and nonoperative treatment for Mason type II fractures. Effect estimates were pooled using random effects models. The primary outcome was elbow function, assessed by the Mayo Elbow Performance Score (MEPS). Secondary outcomes included range of motion, complications, reinterventions and quality of life. ResultsFour studies, including three observational studies and one randomized controlled trial, with a total of 181 patients were included. No significant difference in the MEPS was observed between the operative and nonoperative group (MD 2.67, 95% CI -4.48, 9.83, I² 82%). Range of motion of elbow flexion, extension, pronation, and supination showed no significant difference. The nonoperative group showed no increased risk for overall complications at 9.2% versus 23.4% (OR 2.66, 95%CI 0.83, 8.49, I2 25%) or reinterventions at 5.7% versus 11.7% (OR 1.29, 95%CI 0.13, 12.30, I2 57%). ConclusionThis meta-analysis could not demonstrate a clear advantage of operative treatment for Mason type II fractures in terms of function or complications. However, the long-term effect of surgery in preventing osteoarthritis remains uncertain and should be considered in the treatment decision as well as the degree of fracture displacement, even within the Mason type II spectrum. Further research focusing on long-term follow-up is needed to make a definitive statement in this regard. |
||
|
PSGC21
Screw fixation versus plate fixation for radial head fractures: meta-analysis
Niels van der Hoeven, Oegstgeest NL / Luzern NL / Leiden NL
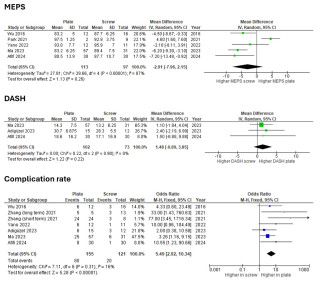
AbstractBackgroundRadial head fractures are often treated with screw or plate fixation, but the optimal method is uncertain. This meta-analysis compares functional outcomes, complication rates, and patient-reported measures (MEPS and DASH) between these methods. AimsThe aim is to determine the comparative effectiveness of screw fixation versus plate fixation for radial head fractures by analyzing functional outcomes, complication rates, and patient-reported measures (MEPS and DASH). MethodsA PubMed search identified 13 studies (1 RCT, 12 observational). Outcomes included range of motion (flexion, extension, supination, pronation), MEPS, DASH scores, and complication rates. Heterogeneity was assessed with I², and analyses were visualized using RevMan forest plots. ResultsScrew fixation showed better outcomes in supination (MD: -6.55°, 95% CI: -10.29 to -2.81, p = 0.0006, I² = 63%) and pronation (MD: -7.15°, 95% CI: -10.61 to -3.69, p < 0.0001, I² = 54%). Flexion (MD: -1.01°, 95% CI: -2.65 to 0.63, p = 0.23, I² = 0%) and extension (MD: 2.98°, 95% CI: -2.64 to 8.60, p = 0.30, I² = 93%) showed no significant differences. MEPS (MD: -2.91, 95% CI: -7.96 to 2.15, p = 0.26, I² = 87%) and DASH (MD: 1.48, 95% CI: -0.89 to 3.85, p = 0.22, I² = 0%) were also similar. Plate fixation had significantly higher complication rates (OR: 5.49, 95% CI: 2.92 to 10.34, p < 0.00001, I² = 16%). ConclusionScrew fixation results in better supination, pronation, and fewer complications than plate fixation for radial head fractures. While screw fixation appears preferable, high heterogeneity in some outcomes underscores the need for further research.

|
||
|
PSGC22
Validation of the AOSpine-DGOU Osteoporotic Fracture Classification – Effect of surgical experience, surgical specialty, work-setting and trauma center level on reliability and reproducibility
Julian Scherer, Zurich / Cape Town
AbstractBackgroundOsteoporotic vertebral fractures (OVFs) are of increasing concern as they may result in a major morbidity and a potential risk factor for mortality. AimsThe aim of this international validation study was to assess the reliability of the new AO Spine-DGOU Osteoporotic Fracture Classification (OF classification) stratified by surgical specialty, work-setting, work-experience, and trauma center level. Methods320 spine surgeons participated in this online-webinar based validation process and were asked to rate 27 cases according to the OF classification at two time points, four weeks apart (assessment 1 and 2). The Cohen´s Kappa (κ) statistic was calculated to assess the inter-observer reliability and the intra-rater reproducibility. ResultsAmongst all participants, the global interrater reliability was moderate in both, first and second assessment (κ=0.57; κ=0.58). Participants with a work-experience of more than 20 years showed the highest inter-rater agreement amongst all participations in both assessments globally (κ=0.65; κ=0.67). Neurosurgeons had the best global inter-rater agreement in the first assessment (κ=0.59) whereas orthopaedic spine surgeons showed a higher agreement in assessment two (κ =0.60). Participants from a level-1 trauma center showed the highest agreement (κ=0.58), whereas participants working at a tertiary trauma center showed higher grade of agreement in the second assessment (κ=0.66). Participants working in academia showed the highest agreement in the second assessment (κ=0.6). Surgeons with academic background and surgeons employed by a hospital showed substantial intra-rater agreement in the second assessment. Amongst all participants, the median intra-rater reproducibility was substantial (κ=0.71). ConclusionOverall, the AO Spine-DGOU Osteoporotic Fracture Classification showed moderate to substantial inter-rater agreement as well as intra-rater reproducibility regardless of work-setting, surgical experience, level of trauma center and surgical specialty. Non-spine colleagues’ ratings were inferior to the ratings of spine surgeons, which suggests that training for non-spine disciplines should be educated towards this classification. |
||
|
PSGC24
Comparative Biomechanical Analysis of Radial Neck Plate Versus Tripod Fixation in Complex Mason Type III Radial Head Fractures
Moritz Kraus, Zurich / Davos
AbstractBackgroundProximal radius fractures, particularly Mason Type III, pose significant challenges in elbow surgery due to their complexity and impact on joint function. While the radial neck plate is a reliable option, it may cause soft tissue irritation and restrict range of motion. The tripod fixation method, using headless compression screws (HCS), aims to address these complications. AimsThis study compares the biomechanical properties of two fixation techniques: the radial neck plate and an advanced tripod fixation approach. MethodsProximal radius fractures, particularly Mason Type III, pose significant challenges in elbow surgery due to their complexity and impact on joint function. This study compares the biomechanical properties of two fixation techniques: the radial neck plate and an advanced tripod fixation approach. While the radial neck plate is a reliable option, it may cause soft tissue irritation and restrict range of motion. The tripod fixation method, using headless compression screws (HCS), aims to address these complications. ResultsIn both fracture models, tripod fixation demonstrated superior biomechanical performance compared to the radial neck plate, particularly in AP bending and axial compression. In the three-part fracture model, tripod fixation exhibited significantly higher stiffness in AP bending (197 ± 56 N/mm vs. 51 ± 31 N/mm, p < 0.001) and axial compression (794 ± 263 N/mm vs. 327 ± 122 N/mm, p = 0.005). In the four-part fracture model, tripod fixation also showed greater stiffness in AP bending (110 ± 67 N/mm vs. 46 ± 60 N/mm, p = 0.14) and axial compression (647 ± 243 N/mm vs. 326 ± 194 N/mm, p = 0.038). No significant differences were observed in mediolateral bending, pronation, or supination. ConclusionTripod fixation provides superior stiffness in AP bending and axial compression while minimizing soft tissue irritation and preserving range of motion. These findings highlight its potential clinical benefits, warranting further randomized trials. |
||
|
PSGG26
Multistaged Aortic Repair for a 14-Year-Old with Loeys-Dietz Syndrome: A Case Report
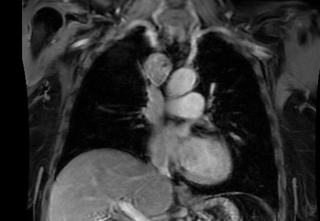
Konstantinos Koumarelas, Bern
AbstractBackgroundLoeys-Dietz Syndrome (LDS) is an autosomal dominant connective tissue disorder characterized by aggressive vascular manifestations, often necessitating early surgical intervention. Case_presentationWe report on a 14-year-old female with LDS Type 2, with a previous open surgical repair (OSR) of aortic root and arch, who presented with a symptomatic diverticulum of the ductus arteriosus and critical right upper extremity ischemia, due to newly diagnosed subclavian artery (SA) aneurysm and occlusion immediately distal to the site (axillary and branchial artery). Urgent surgical management included the exclusion of the right SA aneurysm using a 8mm reinforced PTFE graft. Additional embolectomy through the brachial artery was performed using a Fogarty catheter, to restore blood flow, resulting in palpable radial and ulnar pulses after the operation. In a second procedure three days later, left common carotid artery (LCCA) - SA bypass and thoracic endovascular aortic repair (TEVAR) landing in zone 2 followed. Chimney stent in the LCCA was required caused by partial coverage of LCCA's origin. LSA was occluded with 14mm vascular plug. Postoperative scans revealed distal progression of the disease, resulting in distal extension with TEVAR, an open aortic repair of the thoracoabdominal segment. ConclusionCombined endovascular and open aortic repair can be used to treat acute aortic patholiges in LDS. In younger patients, vessel diameters are likely to expand over time, which can compromise the durability of the endovascular intervention and increase the risk of complications, such as endoleaks and fixation failures. 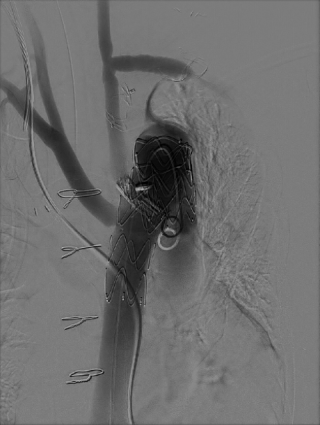
|
||
|
PSGT32
Massive Hypopharyngeal Dilatation and Cervical Lung Herniation in a Semi-Professional Wind Instrument Player
Michail Galanis, Bern
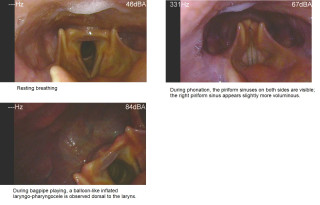
AbstractBackgroundWind instrument playing requires high intrathoracic and pharyngeal pressures. Over time, this can lead to rare structural changes in the upper airway and surrounding areas. This case report describes a musician who developed massive hypopharyngeal dilatation and cervical lung herniation. The aim is to highlight the risks of these conditions and the importance of early diagnosis and treatment. Case_presentationA 46-year-old semi-professional wind instrument player reported sharp pain on the right side of his throat while playing. He had no difficulty speaking or breathing, but the pain occurred during performances. A detailed examination, including laryngostroboscopy and dynamic CT scans, was done. The tests showed significant dilatation of the hypopharynx and herniation of the lung apices into the neck, particularly on the right side. The size of the dilation increased with the amount of pressure required by the instrument being played. A multidisciplinary team recommended stopping wind instrument playing to avoid complications like pneumothorax. ConclusionThis case highlights the dangers of sustained high-pressure activities like wind instrument playing. Early recognition of symptoms, use of imaging techniques, and proper management are key to preventing serious complications. Musicians and clinicians should be aware of these risks for timely diagnosis and intervention. 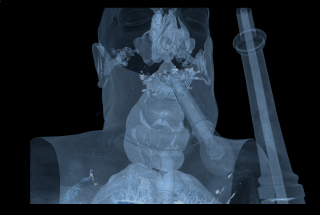

|
||
|
PSGT33
Tailored Multimodal Management of Desmoplastic Small Round Cell Tumor: Optimizing Survival with Precision Surgery, Systemic Therapy and Coordinated Care
Eleonora Minerva, Zürich
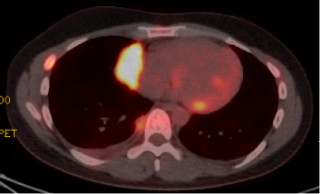
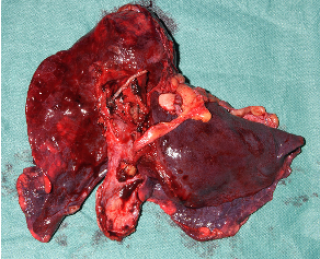
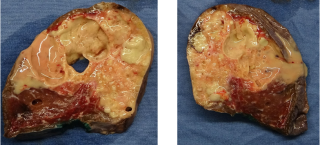
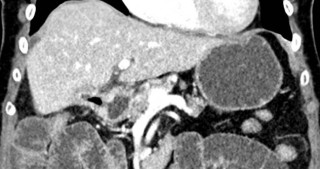
AbstractBackgroundDesmoplastic small round cell tumor (DSRCT) is a rare and aggressive malignancy primarily affecting young individuals. Characterized by a unique chromosomal translocation (EWSR1-WT1 fusion), it often presents with widespread metastases at diagnosis. Multimodal treatment, including chemotherapy, surgery, and radiotherapy, is essential for disease control, though prognosis remains poor. Case_presentationA 32-year-old male was diagnosed with DSRCT (UICC Stage IV) with tumor localizations including the right pleura, right hilum (Fig.1), mediastinum, right paratracheal lymph nodes, subpleural and paracardiac parenchymal masses (Fig.2), left supraclavicular masses, right portal lymph nodes and retroperitoneal lymph nodes. Initial treatment comprised two cycles of cisplatin and etoposide, followed by immunochemotherapy incorporating atezolizumab. After a revised diagnosis, treatment transitioned to the vincristine, doxorubicin and cyclophosphamide regimen combined with ifosfamide and etoposide (VDC/IE) for 11 cycles. Restaging indicated a metabolic and morphological tumor response. Multidisciplinary sarcoma board discussions recommended stereotactic radiation therapy of abdominal and cervical lesions followed by surgery. The patient underwent a right pneumonectomy (Fig.3) with partial resections of the pericardium, diaphragm, and liver. Post-surgical PET-CT showed no evidence of recurrence or active metastases. Chemotherapy was resumed and completed with additional three cycles of VDC/IE. A follow-up PET-CT four months after surgery confirmed no disease progression. The patient remained clinically stable, reporting improved quality of life. ConclusionManaging DSRCT requires a personalized and multidisciplinary approach integrating systemic therapy, surgery, and radiotherapy to optimize survival outcomes. Complex surgical procedures, including multi-organ resections, are pivotal and should be performed in highly specialized centers. PET-CT imaging is essential throughout management, guiding decisions and monitoring response. Long-term follow-up and coordinated care are essential for early detection of recurrences and mantaining quality of life. 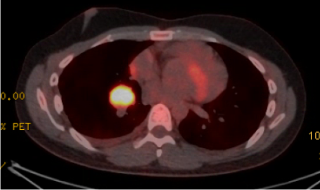
|
||
|
PSGT34
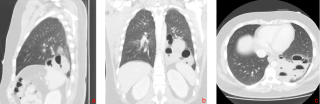
Rare Differential Diagnosis of Symptomatic Pericarditis: Isolated Epithelioid Mesothelioma of the Pericardium
Eleonora Minerva, Zürich
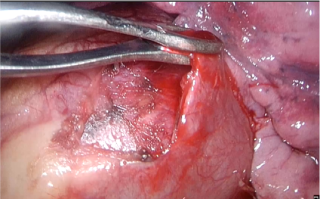
AbstractBackgroundIsolated pericardial mesothelioma is an extremely rare malignancy, often presenting with nonspecific symptoms such as recurrent pericarditis or pericardial effusion. Due to its rarity and nonspecific presentation, it is frequently misdiagnosed or discovered only at advanced stages. Definitive treatment options are limited, and the prognosis remains poor. Multimodal imaging and histological analysis are critical for accurate diagnosis, and management typically focuses on palliative care. Case_presentationA 69-year-old female with a history of recurrent pericarditis first diagnosed in April 2024 was admitted in September 2024 with worsening dyspnea, fatigue, and a reduced general condition. Initial workup revealed an inflammatory response and a pericardial mass infiltrating left-sided cardiac structures and compressing the left atrium, superior pulmonary veins, and superior vena cava. Echocardiography showed a pericardial mass, while CT imaging suggested a primary pericardial mesothelioma with mediastinal lymph node involvement (Fig.1) Biopsy obtained via video-assisted thoracoscopic surgery (VATS, Fig.2) confirmed epithelioid mesothelioma six months after onset of symptoms, positive for WT1 and D2-40, and negative for Claudin-4, BerEP4, ALK, and PDL-1. The patient had no history of asbestos exposure. Given the advanced stage and tumor location, the multidisciplinary tumor board recommended systemic palliative therapy based on the MAPS trial protocol, consisting of Carboplatin, Pemetrexed and Bevacizumab. Symptom management included glucocorticoids, antiarrhythmic therapy with Amiodarone, and anticoagulation. The patient remained hemodynamically stable despite a moderate pericardial effusion. Radiotherapy was deferred due to the tumor's critical anatomical location. ConclusionIsolated pericardial mesothelioma is a rare condition often mimicking recurrent pericarditis. Diagnosis requires multimodal imaging, such as echocardiography and CT, with histological confirmation via biopsy. Immunohistochemical markers like WT1 and D2-40 help differentiate it from other malignancies. Treatment is primarily palliative, focusing on systemic chemotherapy, with radiotherapy considered in selected cases. Early multidisciplinary collaboration is essential for optimal care. 
|
||
|
PSGT35
ROBOTIC-ASSISTED THORACOSCOPIC SURGERY FOR ECTOPIC MEDIASTINAL THYROID: A RARE PRESENTATION WITH PROGRESSIVE ENLARGEMENT
Eleonora Minerva, Zürich
AbstractBackgroundEctopic thyroid tissue is an uncommon developmental anomaly resulting from aberrant migration of thyroid precursor cells during embryogenesis. While ectopic thyroid tissue is most frequently located in the lingual region, mediastinal ectopic thyroid is a rare entity (<1%). Management includes distinguishing ectopic thyroid from other mediastinal masses, especially in cases of progressive enlargement, which raises concerns for malignancy or compressive symptoms. Case_presentationA 58-year-old female presented with a progressively enlarging mediastinal mass detected during follow-up imaging. The mass was initially identified four years prior, measuring approximately 3 cm, and diagnosed as benign (Thy 2) through endobronchial ultrasound-guided biopsy. The patient remained asymptomatic with no evidence of thyroid dysfunction. However, recent imaging revealed the lesion had increased to 4.8 cm and was now causing subtle compression of adjacent structures. Thoracic magnetic resonance imaging confirmed a well-circumscribed mass with no signs of infiltration to surrounding structures, and localized anterolateral to the trachea on the right side of the superior mediastinum (Fig.1). Given the increase in size and potential risk of developing malignancy and relevant tracheal compression, the patient was referred for surgical management. A robotic-assisted thoracoscopic surgery (RATS) was performed to achieve complete resection (Fig.2). The procedure was uneventful, and the patient experienced a smooth postoperative recovery. The patient was discharged on the second postoperative day. Histopathological analysis confirmed the mass as ectopic thyroid tissue without evidence of malignancy. ConclusionProgressive enlargement of ectopic thyroid tissue warrants surgical evaluation to exclude malignancy or manage compression-related complications. Cross-sectional imaging, combined with prior biopsy results, is valuable for monitoring and guiding management decisions. RATS is a minimally invasive and effective option for resecting mediastinal lesions, ensuring rapid recovery and precise outcomes. In conclusion, awareness of this rare entity can facilitate timely diagnosis and appropriate management, avoiding delays or overly aggressive interventions. 
|
||
|
PSGT36
The Role of Surgical Stabilization of Rib Fractures (SSRF) in Patients With Clinically Relevant Flail Chest After Mechanical Resuscitation; A Case Report
Moritz Menz, Schaffhausen
AbstractBackgroundFlail chest is a serious traumatic injury characterized by the fracture of multiple ribs, resulting in a paradoxical movement of a chest segment during respiration. This condition leads to impaired ventilation, respiratory distress, and often requires intensive medical intervention. Flail chest commonly occurs in high-impact trauma, such as accidents, falls or in cases of mechanical chest compression. Timely diagnosis and management are crucial to prevent complications such as respiratory failure and prolonged recovery. Treatment may include mechanical ventilation, pain control, and surgical stabilization in severe cases. Case_presentationWe present a 56-year-old patient after emergency department trauma activation due to an out-of-hospital cardiac arrest, with successful ROSC following bolus aspiration. CT imaging revealed a right-sided hemothorax as well as several displaced rib fractures bilaterally. A chest drain was inserted, and the patient was monitored in the surgical intensive care unit. The residual bolus (broccoli) was successfully removed bronchoscopically. During the ICU stay, the patient developed a progressive severe respiratory acidosis with paradoxical breathing suggestive of a flail chest, thereafter a protective intubation was performed. Due to the lack of respiratory compensation and the inability to extubate, a decision was made to proceed with SSRF due to a clinically relevant flail chest. Subsequently, there was a rapid improvement in the patient's symptoms, and the patient was extubated in a timely manner. The course of recovery was uneventful, and the patient was discharged for rehabilitation. ConclusionThe clinical picture of flail chest due to rib fractures is a common occurrence following high-energy trauma or mechanical resuscitation. The role of rib fracture osteosynthesis has been increasingly emphasized in recent studies. The main benefits include a significant reduction in the cumulative time spent in the intensive care unit, markedly reduced respiratory fatigue, intubation times, and a significant improvement in pain management. |
||
|
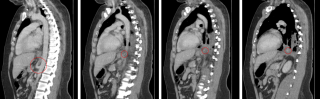
PSGT37
Infected Intralobar Pulmonary Sequestration – a Case Report
Lea Projer, Bern / Aarau
AbstractBackgroundBronchopulmonary sequestration is a rare congenital lung anomaly characterized by the presence of non-functioning lung tissue that does not communicate with the bronchial tree and receives its blood supply from the systemic circulation. The arterial blood supply derives mostly directly from the thoracic or abdominal aorta. Bronchopulmonary sequestrations are divided into intralobar and extralobar sequestrations, whereby intralobar sequestrations have the same pleura visceralis as the rest of the lung whereas extralobar have their own pleura visceralis. They are often asymptomatic but can lead to recurrent pulmonary infections and haemoptysis in children or young adults. Case_presentationWe aim to present the case of an infected intralobar pulmonary sequestration of a 23-year-old male. The patient was diagnosed with an infected intralobar pulmonary sequestration after investigations for persistent respiratory symptoms. There was no increased susceptibility to pulmonary infections in the patient`s history. CT-scan revealed a 10,5 cm consolidation in the left lower lobe with an aberrant systemic arterial supply trough the celiac trunk. After initial antibiotic treatment and improvement of the patient`s clinical condition, uniportal-VATS left lower lobe resection was performed. Intraoperatively, the aberrant artery was identified next to the pulmonary ligament and dissected separately. The postoperative course was uneventful, and the patient experienced complete resolution of symptoms. Chest tube was removed on day two and the patient discharged on the third postoperative day. ConclusionThis case report highlights the importance of early recognition and accurate treatment of bronchopulmonary sequestrations by performing lobar or sublobar thoracoscopic resection. 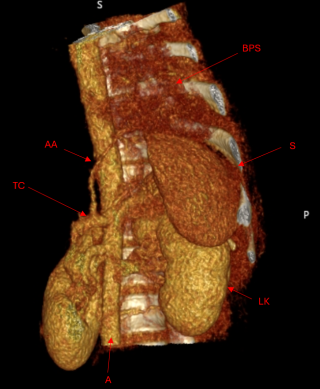

|
||
|
PSGT38
Cavitary Pulmonary Lesion With Bronchopleral Fistula Covered With a Pericardial Patch and Pedicled Latissimus Dorsi Muscle Flap – A Case Report
Andra-Luana Lazarescu,
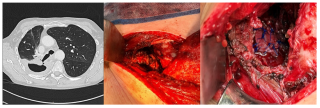
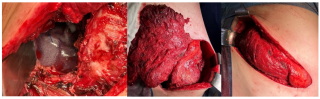
AbstractBackgroundNot only primary lung cancers, but also metastasis can lead to cavitations, with squamous cell carcinomas being the most commonly associated with this phenomenon. The aim of this presentation is to underline the versatility of local and regional, thoracal and abdominal muscle flaps for covering cavitary pulmonary lesions. Case_presentationA 63-year-old male patient with COPD was diagnosed with central hilar squamous cell carcinoma (cT4 cN3 cM0, UICC Stadium IIIC) in the right upper lobe. (Figure 1) He underwent chemo-, radio- and immunotherapy. He was admitted to our department eleven months subsequent to the tumor diagnosis, following recurrent infections and a persistent cavern in the posterior right upper lobe. The bronchoscopies showed no tumor and confirmed an infection with Haemophilus influenzae for which he underwent a longterm therapy with Clindamycin. As paliative surgical sanitation, we performed a partial resection of the 5th and 6th ribs, removed the abscess and identified a relatively large defect – bronchopleural fistula. (Figure 1) It was not viable for primary suture closure or resection. In order to achieve an airtight seal over the bronchial fistula, a bovine pericardial flap was utilized to cover the defect. In scope of transfering the Latissimus dorsi to the cavity, we chose an infrascapular route.(Figure 2) Postoperatively the patient developed a seroma that was resolved at one month after the surgery, otherwise the clinical course was progressively better with lower infection parameters and a satisfactory thorax-CT control. (Figure 3) ConclusionA pedicled latissimus dorsi muscle flap that is highly vascularized is a highly efficient option for tissue coverage in cavitary lesions, not only due to its bulky size but also due to its ability to combat infection. 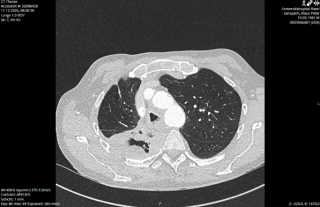

|
||
|
PSGVC39
Combination of Traumatic Diaphragmatic and Costal Rupture With Organ Herniation: Report of a Case
Iride Porcellini, Genève
AbstractBackgroundTraumatic diaphragmatic rupture is a rare, life-threatening injury, often caused by blunt or penetrating trauma. Its nonspecific presentation and association with other injuries frequently delay diagnosis and treatment, increasing the risk of complications. Definitive treatment is surgical repair, often performed by a multidisciplinary team. Case_presentationA 77-year-old female involved in a high-speed motor vehicle collision presented with thoraco-abdominal pain. CT-scan revealed a 10 cm diaphragmatic tear associated with an abdominal wall rupture, altogether resulting in an intra-thoracic hernia involving the colon and the liver. Additional injuries included a right pneumothorax, rib fractures, a sternal fracture, and seatbelt-related hematomas. Surgical exploration by visceral and thoracic surgeons required an incision centered on the tear along the axis of the ribs and involved reducing herniated organs, repairing diaphragmatic and abdominal wall defects, reconstructing the costal margin, and stabilizing ribs with a Stratos staple (Fig. 1, 2, 3) . The patient recovered without complications and was discharged after two weeks. ConclusionHigh-speed collisions are a major cause of traumatic diaphragmatic rupture (TDR), with delayed diagnoses often due to nonspecific symptoms. While TDRs typically affect the left side due to the liver’s protective effect, this case involved a right-sided rupture combined with an abdominal wall tear resulting with organs herniation. Imaging findings were consistent with severe cases, but the combination of abdominal wall hernia and extensive rib fractures represents a rare presentation. Prompt surgical intervention, usually performed via thoracotomy, laparotomy, or minimally invasive methods, is critical. We opted for an open approach, given the the size of the defect and organ herniation. 


|
||
|
PSGVC40
Incidental Discovery of Pneumatosis Intestinalis in an Hemodialysis Patient
Lina Berrada Dirhoussi, Yverdon-les-Bains
AbstractBackgroundPneumatosis intestinalis (PI) is a clinical condition characterized by the presence of gas within the bowel wall and is considered a rare medical finding. In some cases, it may be a harmless incidental discovery; however, in others, it can indicate more severe forms of gastrointestinal disease. Case_presentationWe present the case of an 87-year-old male with end-stage kidney disease on hemodialysis, in whom PI was incidentally discovered during a routine follow-up computed tomography (CT) scan for a renal mass (Figure 1). The patient was asymptomatic, and imaging showed no signs of ischemia, bowel obstruction, or perforation. The absence of symptoms or complications allowed for successful conservative management. ConclusionThis case highlights the incidental discovery of PI in an asymptomatic patient with chronic kidney disease. The absence of complications and risk factors underscores the benign nature of idiopathic PI in some patients, allowing for conservative management. This report emphasizes the importance of distinguishing between benign and life-threatening forms of PI through thorough clinical and radiological evaluation. Further research is needed to explore the relationship between chronic kidney disease, hemodialysis, and the development of PI, as well as to refine management strategies for this rare condition. 
|
||
|
PSGVC41
The Risk of Barbecuing: Metal Bristle Ingestion Can Cause Gastrointestinal Perforation - A Case Report
Theodora Dionysopoulou, Oberwil
AbstractBackgroundWhile barbecuing in summer is a popular activity, it bears a rare but dangerous risk of ingestion of metal bristles attached to the grilled food. This case reports describes a liver abscess caused by gastric perforation due to metal bristle ingestion. Case_presentationA 33-year old man presented with fever and weakness of unknown origin. Computed tomography scan showed a liver abscess with a metal foreign body. Eventually, diagnostic laparoscopy showed a small gastric perforation next to the liver abscess with migration of the metal bristle into the liver, causing the abscess. Consecutively, liver abscess evacuation, recovery of the foreign body and gastric perforation repair with sutures was performed. The patient received intravenous antibiotic treatment for 10 days followed by oral antibiotics for another 4 days. Follow-up showed decreasing CRP and WBC and rapid recovery after surgery. ConclusionUtensils used for food preparation should be considered in differential diagnosis for bowel perforation and liver abscesses. Thin metal wires can detach, be ingested and cause gastrointestinal complications. |
||
|
PSGVC42
A Case Report of the Surgical Management of an Elderly Patient With Biliary Ileus
Francesco Bartoloni Saint Omer, Locarno
AbstractBackgroundBiliary ileus is a rare cause of intestinal obstruction, accounting for roughly 1% of ileuses and associated with the presence of a biliary-enteric fistula, known as “Mirizzi syndrome”. It’s management can be complex in elderly patients, the dominating symptomatic population, where the balance between conservative and surgical management is crucial. Case_presentationOur case involves an 88-year-old female, resident in a long term care facility (LTCF) with a medical history of Alzheimers disease and cholecystolithiasis. She presented to the emergency department for an aspecific clinical deterioration and agitation. Clinical exam demonstrated abdominal distension and absence of bowel sounds. A CT scan showed ileus caused by a biliary stone of the middle-ileal tract, with a cholecystduodenal fistula with pneumobilia, known as the classical “Riglers triad”. Due to the patients general condition and family wishes, conservative therapy was undertake. Within 24hours of hospitalisation a Xray showed no progression of the calculus towards the terminal ileum. Additionally, patient management with nasogastric tube resulted difficult due to the cognitive state. Following a familial conference, laparoscopy and extra-corporeal enterotomy of the obstructed ileum and calculus extraction was indicated. The post-operative course was regular, with progressive clinical improvement and discharge to the LTCF. ConclusionThis case highlights the classical signs and symptoms of biliary ileus, being “Riglers triad” and the challenges in the elderly population. The decision between conservative and surgical approaches requires careful risk-benefit analysis however surgical management remains the treatment of choice also in the fragile polymorbid population. Targeted management, considering the patient's general condition and collaboration with family members, can ensure a favourable outcome even in the most complex cases 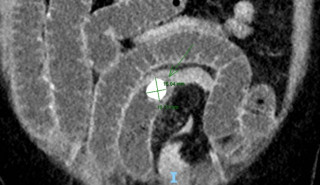

|
||
|
PSGVC43
A Case of Spontaneous Splenic Rupture two Weeks After Appendectomy: A Rare and Life-Threatening Condition
Evan André, Muraz / Rennaz
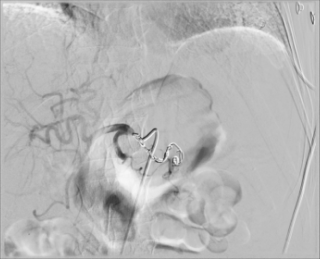
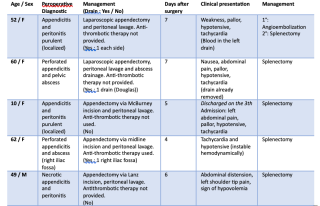
AbstractBackgroundSpontaneous splenic rupture (SSR) is an exceedingly rare and potentially life-threatening complication, typically associated with underlying conditions such as hematologic disorders, infections, or inflammatory diseases. While SSR has been documented following various abdominal procedures, its occurrence after appendectomy is exceptionally uncommon, with only five cases reported in the literature to date (Table 1). To our knowledge, this is the first case of SSR following appendectomy successfully managed with arterial embolization. This study details a rare case of SSR in a 73-year-old male, with treatment decisions guided by a comprehensive literature review. Case_presentationA 73-year-old male with a history of ischemic heart disease, treated with dual antiplatelet therapy, developed spontaneous splenic rupture 14 days after laparoscopic appendectomy. The patient presented with acute abdominal pain and hypotension, without any history of trauma. Imaging confirmed a large subcapsular splenic hematoma with active bleeding (Figure 1). Following prompt diagnosis, the patient was successfully treated with arterial embolization (Figure 2). SSR following appendectomy is an exceptionally rare phenomenon, with only five cases documented in the literature. Previous cases typically involved splenectomy as the treatment of choice. In contrast, this case represents the first successful use of arterial embolization, an alternative, less invasive approach. The pathophysiology of SSR remains unclear, though factors such as postoperative inflammation, the patient's antiplatelet therapy, and potential splenic vulnerabilities may contribute. Additionally, perioperative manipulation, such as abdominal lavage and organ handling, may increase mechanical stress on the spleen or exacerbate inflammatory responses. ConclusionSpontaneous splenic rupture (SSR) is a rare but serious complication following abdominal surgeries. Clinicians should remain vigilant and consider SSR in cases of unexplained postoperative abdominal pain. Its potential causes are not well-defined, making diagnosis challenging. This case emphasizes the importance of early detection and timely intervention. Arterial embolization, a well-established procedure, offers a less invasive alternative to splenectomy. 
|
||
|
PSGVC44
Management of a Patient with Acute Abdomen and Thyroid Storm – A Case Report
Sophie Eschlboeck, Basel
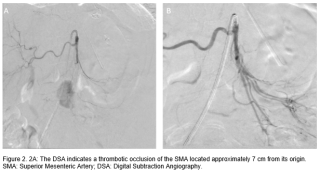
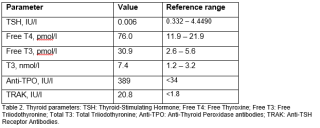
AbstractBackgroundAcute abdomen, typically characterized by severe and sudden abdominal pain, often requires urgent surgical intervention. In some cases, thyrotoxicosis can directly or indirectly contribute to the development of acute abdomen, complicating both diagnosis and management. Understanding the interplay between thyrotoxicosis and acute abdomen is crucial for effective management. Case_presentationWe describe a case of a 54-year-old female with no significant medical history who presented with acute abdominal pain and diarrhea, rapidly deteriorating to respiratory failure requiring intubation. Initial investigations, including computed tomography angiography, revealed an embolic occlusion of the superior mesenteric artery (SMA) and signs of bowel ischemia as well as cardiopulmonary decompensation. Subsequent thyroid function tests confirmed thyrotoxicosis. The patient underwent emergency endovascular embolectomy, bowel resection, and later a total thyroidectomy. The patient’s acute abdomen was managed with embolectomy and bowel resection. When investigating the underlying cause, thyroid function tests revealed a thyroid storm, necessitating urgent total thyroidectomy. Postoperatively, the patient stabilized hemodynamically and was discharged in good condition. Histopathology confirmed chronic thyroid inflammation with increased endocrine activity. Multidisciplinary management, including endocrinology and cardiology input, was pivotal in the patient’s recovery. ConclusionThis case highlights the rare but serious complication of mesenteric ischemia due to thyroid storm. The combination of treatments not only addressed the acute vascular emergency but also stabilized the underlying thyrotoxicosis. Endovascular thrombectomy and bowel resection effectively managed the ischemia, while thyroidectomy facilitated a rapid return to a euthyroid state, preventing further complications. This case serves as a valuable reference for the management of similar complex presentations, demonstrating the potential for successful outcomes with timely, aggressive treatment. 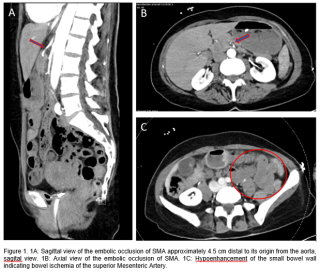
|
||
|
PSGVC45
Coexistence of Adenomyomatosis in a Left-Sided Gallbladder: A Case Report.
Hadeer Hafez, october 6th EG
AbstractBackgroundThe coexistence of gallbladder (LSG) and adenomyomatosis (ADM) is extremely uncommon presenting a novel clinical dilemma that has not been previously documented. LSG refers to a anomaly where the gallbladder is situated to the left of the round ligament deviating from its usual position. This anomaly is rare, with reported occurrences ranging between 0.04% and 1.1%. Identifying LSG before surgery poses challenges. It is often discovered incidentally during procedures necessitating surgical expertise to safely manage anatomical variations. Case_presentationA patient in his 60s with untreated hepatitis C virus (HCV) and hepatocellular carcinoma (HCC) presented with acute epigastric pain, liver cirrhosis, and malignant thrombi in the IVC and portal vein. Physical exams and lab tests showed elevated WBC and CRP, with worsening condition after 48 hours. A CT scan confirmed a left-sided gallbladder and acute cholecystitis. Surgery was performed within 48 hours using modified port positions due to anatomical anomalies (Figure 1). Intraoperative findings revealed an abnormal Calot’s triangle (Figure 2) and adenomyomatosis. The patient was discharged without complications but later readmitted due to unrelated liver function issues. ConclusionThe combination of LSG and ADM in a setting poses an intricate challenge. Surgeons need to be ready to recognize and address these abnormalities effectively for the well being of the patient and favorable results. This particular case highlights the importance of staying alert and flexible during surgery when dealing with gallbladder variations. 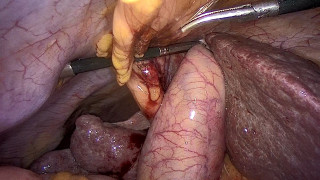

|
||
|
PSGVC46
Spontaneous Thrombosis of the Pampiniform Plexus: A Report of Two Cases
FABIEN Schaller, Fribourg
AbstractBackgroundThrombosis of the pampiniform plexus is an extremely rare condition, with fewer than 50 documented cases since its first description by McGavin in 1935. It commonly manifests as acute scrotal pain and swelling, mimicking urological emergencies like testicular torsion or epididymo-orchitis. The left side is more frequently affected due to anatomical factors. Risk factors include hypercoagulable states, physical exertion, trauma, surgeries, and infections such as COVID-19, although some cases arise spontaneously without identifiable causes. There are no standardized treatment guidelines; however, anticoagulation therapy is widely used, while surgery is reserved for complications or diagnostic uncertainties. AimsTo describe two cases of pampiniform plexus thrombosis, highlighting their presentation, treatment, and outcomes to enhance awareness in emergency care and contribute to existing literature. MethodsCase 1: A 39-year-old healthy male presented with acute, progressive right testicular pain radiating to the pubic region. Examination revealed painful testicular palpation and a mass in the right spermatic cord without signs of infection. He had undergone a vasectomy six months earlier. Both patients received rivaroxaban (20mg daily for six weeks), analgesics, and scrotal support. ResultsBoth patients showed significant clinical improvement. Follow-up Doppler ultrasonography confirmed thrombus resolution in three weeks for Case 1 and four weeks for Case 2. ConclusionThese cases emphasize the importance of considering pampiniform plexus thrombosis in patients with atypical acute scrotal pain. Conservative anticoagulant therapy proved effective for symptom resolution and thrombus clearance, supporting its use in uncomplicated cases. This report contributes valuable insights into diagnosing and managing this rare condition. |
||
|
PSGVC47
Metastatic Intussusception : A Rare Complication Of Myxofibrosarcoma
Lina Berrada Dirhoussi, Yverdon-les-Bains
AbstractBackgroundMyxofibrosarcoma is a common subtype of soft tissue sarcoma that occurs mostly in elderly people and is characterized by its invasiveness as well as high recurrence rate. Its propensity for both distant metastasis and local recurrence complicates the treatment plan and outcomes, presenting significant challenges in patient management. Small bowel metastases are of unusual location, we describe a possible manifestation. Case_presentationOur case report involves an 86-year-old male diagnosed with high-grade myxofibrosarcoma of the right thigh. After undergoing surgical resection followed by adjuvant radiation therapy, the patient developed pulmonary and muscle metastases. Subsequently, the patient presented clinically with small bowel obstruction. A computed tomography (CT) scan of the abdomen confirmed intussusception (Figure 1). The patient was taken to the operating room, where reduction and resection of the affected small bowel were performed (Figure 2,3). Histopathological analysis confirmed metastasis of the known myxofibrosarcoma. ConclusionThis case highlights the aggressive nature of high-grade myxofibrosarcoma (MFS) and its potential to metastasize to unusual sites, complicating diagnosis and management. Uncommon presentations, such as intussusception, should raise suspicion and prompt a multidisciplinary approach with close monitoring for optimal patient care. The occurrence of intussusception due to metastatic MFS in this patient is rare, underscoring the importance of considering unusual complications when managing high-grade MFS. This case also emphasizes the critical role of advanced imaging in guiding diagnosis and treatment, ultimately improving patient outcomes. 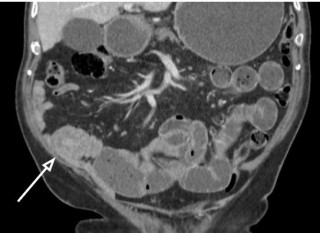


|
||
|
PSGVC48
Atraumatic Splenic Rupture due to Chronic Pancreatitis and Pancreatic Pseudocysts: A Rare Case of Conservative Management
Raimon Blanche, St-Sulpice / Fribourg
AbstractBackgroundAtraumatic splenic rupture (ASR), referring to splenic rupture occurring without any history of trauma, is a rare and potentially life-threatening condition that typically requires surgical intervention. It is commonly associated with infections, malignancies, or anticoagulant use, though rarer causes, such as pancreatic cysts or pancreatitis, have also been documented. This case describes ASR likely secondary to chronic pancreatitis and pancreatic pseudocysts (PP). This report highlights ASR as a possible complication of chronic pancreatitis and PP, emphasizing the diagnostic challenges of ASR and its successful conservative management.
Case_presentationA 56-year-old man with chronic pancreatitis related to suspected intraductal papillary mucinous neoplasm (IPMN) and caudal pancreatic pseudocysts presented with acute abdominal pain, fever, and chills. Lab tests revealed elevated CRP and hemoglobin levels at 124 g/L. CT imaging showed mild splenomegaly with a hypodense lesion suggestive of splenic rupture, but no active bleeding, and a moderate amount of free fluid in the perisplenic region. Signs of chronic pancreatitis, including caudal PP, were also noted. The patient was hemodynamically stable and was managed conservatively with intravenous antibiotics and close monitoring. Serial ultrasounds showed no progression of free fluid. He was discharged in stable condition, and follow-up CT two months later confirmed regression of the hematoma. This case illustrates ASR as a rare complication of chronic pancreatitis and PP, potentially caused by inflammatory or enzymatic damage to the spleen. While splenectomy is currently the standard of care for ASR, conservative management is a viable option in stable patients without active bleeding. ConclusionASR remains a diagnostic and therapeutic challenge. Early diagnosis and individualized care are essential to improving outcomes. This case underscores ASR as a rare yet potential complication of pancreatitis and PP. Further research is needed to clarify the mechanisms behind this association. 
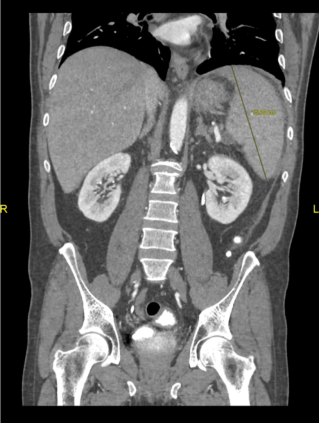
|
||
|
PSGVC49
Importance of Surgical Management in Cystic Duct Remnant Syndrome
Esayas Mustefa, Leuggern
AbstractBackgroundA long cystic duct remnant with or without calculi after laparoscopic cholecystectomy may not be an uncommon occurrence. Residual stones overlooked during the index procedure or recurrent calculus formation within the remnant cystic duct can result in post-cholecystectomy syndrome, which refers to the persistence of gastrointestinal symptoms after cholecystectomy. After establishing the diagnosis, surgical treatment is needed. Case_presentationWe report a case of long cystic duct remnant syndrome with stones in a 45-year-old male patient who experienced persistent preoperative symptoms (upper abdominal pain, dyspepsia) beginning in December 2024, after laparoscopic cholecystectomy performed in April 2023 for acute symptomatic calculous cholecystitis. The diagnosis was made based on transabdominal ultrasound (showing cystic formation in gallbladder fossa) and Magnetic Resonance Cholangiopancreatography (MRCP), supported by laboratory findings. MRCP revealed no evidence of intra- or extrahepatic cholestasis and showed enlarged cystic duct stump with inflammation and two small stones with one of which was distally impacted. Laparoscopic resection was performed without complications. Histopathological findings revealed a segment of the stump with an embedded calculi obstructing the cystic duct remnant. Postoperatively the patient has no symptoms ConclusionLong cystic duct remnant syndrome is not uncommon and is one of the common causes of persistent biliary symptoms after cholecystectomy. MRCP is considered the gold standard to make the diagnosis. Once diagnosed, laparoscopic removal of the stump by an expert surgeon is generally considered safe and is necessary to alleviate symptoms and prevent further complications. 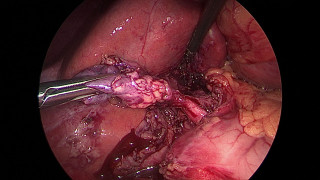
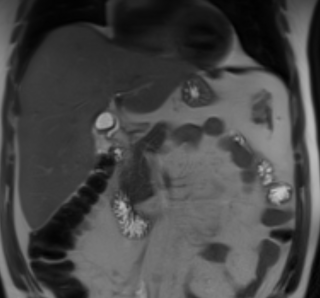
|
||
|
PSGVC50
A Rare Case of Campylobacter Fetus Abdominal Sepsis due to Mesenteric Panniculitis Exacerbation
Julia Cheong, Nyon
AbstractBackgroundMesenteric panniculitis (MP) is defined by chronic inflammation and fibrosis of the mesenteric adipose tissue, predominantly at the root of the small bowel. It is a non-neoplastic condition often detected incidentally on abdominal imaging and is asymptomatic in about 50% of patients. Clinical symptoms of mesenteric panniculitis are highly variable. In case of failure, immunosuppressive treatments can be introduced (azathioprine, anti-TNF agents), although with limited evidence of success. Case_presentationA 71-year-old man with known chronic MP initially presented with fever and abdominal pain with diffuse sensitivity on clinical examination. Initial blood tests showed marked inflammatory response with leucocytosis of 21G/L, CRP 190mg/L and PCT 1.71mcmol/L. Blood cultures were positive for Campylobacter fetus. Abdominal CT scan showed an acute crisis of the known MP with pseudotumoral appearance and peripheral nodes (Figure 1, Figure 2). Antibiotic treatment (imipenem) was administered for 2 weeks with significant clinical and biological improvement. A PET CT highlighted the described MP with multiple moderately hypermetabolic peripheral lymph nodes. Lymphoma was excluded with mesenteric biopsies confirming an inflammatory origin. The treatment administered was effective, leading to a good recovery after this episode and no further exacerbation was reported. ConclusionWe reported a rare case of Campylobacter fetus sepsis on chronic MP. The cause and effect relationship is difficult to establish. This the first documented case of a Campylobacter fetus-specific infection being linked to an MP crisis in literature. 

|
||
|
PSGVC51
Robotic Vertical Gastrectomy With A Suprapubic Approach: A Video Case Report
Antonietta Petrusic, Lugano
AbstractBackgroundRobotic assistance in bariatric surgery has been established as both feasible and safe, offering valuable support in challenging cases. Traditional approaches often result in abdominal scarring, which can be particularly concerning for younger patients. Conversely, the suprapubic approach may be preferred for its potential aesthetic benefits. Despite existing literature on robotic techniques in sleeve gastrectomy (SG), the suprapubic robotic approach was not described yet. This video case report aims to illustrate the application of the suprapubic robotic approach in sleeve gastrectomy for morbid obesity. Case_presentationThe patient, a 55-year-old woman with grade III obesity (BMI 41.7kg/m²) and no obesity-related comorbidities, was selected due to her lack of prior intra-abdominal surgery and height under 175 cm. A suprapubic approach for sleeve gastrectomy was chosen. The procedure began with a supra-umbilical incision, through which an 8 mm trocar for the camera was inserted. Additional trocars were placed suprapubically, including a 12 mm trocar in the left iliac fossa and a 5 mm trocar for assistance in the left hypochondrium. Docking was successful, followed by resection of the gastro-colic ligament and dissection up to the left diaphragmatic pillar to free the His angle. Gastrolysis was performed, leaving a 4-6 cm distance from the pylorus. The antrum was divided using a 60 mm stapler, followed by longitudinal gastrectomy using additional 60 mm staplers, guided by a 42-French bougie. The resected stomach was safely extracted through the 12 mm port using an Endo Catch, with no complications reported during or after surgery. The patient experienced an uneventful recovery, achieving a weight loss of 15 kg at the 3-month follow-up. ConclusionThis case demonstrates that the suprapubic robotic approach is a viable option for sleeve gastrectomy in patients with morbid obesity. Careful patient selection is crucial when considering this surgical technique. |
||
|
PSGVC52
Management of Unexpected Intestinal Nonrotation During Elective Bariatric Surgery
Sima Ulugöl, Zürich
AbstractBackgroundThis case report with intraoperative video documentation details the management of an unexpected anatomical anomaly encountered during elective bariatric surgery. A 54-year-old male patient was admitted for the laparoscopic creation of a proximal gastric bypass due to WHO class III obesity (BMI 40 kg/m²). The patient’s medical history included arterial hypertension and symptomatic cholecystolithiasis. Case_presentationFirst, a routine laparoscopic cholecystectomy was performed without complications, followed by the preparation of a gastric pouch. However, an unexpected anomaly of intestinal anatomy was identified, consistent with nonrotation. Nonrotation is a rare congenital malrotation variant where the small intestine predominantly occupies the right abdomen, and the large intestine is displaced to the left. This posed a significant surgical challenge, as the pre-constructed gastric had already been prepared. Intraoperatively, due to the completely altered abdominal anatomy and the pronounced visceral obesity with a markedly thick greater omentum, it was decided to perform a laparoscopic sleeve gastrectomy with gastrogastrostomy (OrVil™/EEA™ 25 mm circular stapler) instead, especially as the pouch was well perfused from both sides. A tension-free gastrojejunostomy was deemed unfeasible due to the aforementioned anatomical constraints. ConclusionThe intraoperative detection of nonrotation in a bariatric surgery patient underscores the need for surgical adaptability. Transitioning to a sleeve gastrectomy provided a viable alternative that addressed the patient's obesity while mitigating the risks associated with performing a gastric bypass in anomalous anatomy. |
||
|
PSGVC53
Conversion of open vertical banded gastroplasty to robotic gastric bypass: a case report
Virginia Sitta, Lugano
AbstractBackgroundVertical banded gastroplasty (VBG), a once-popular bariatric procedure, is associated with significant long-term failure rates due to complications such as weight regain, dysphagia, and gastro-gastric fistula. This case report describes the robotic-assisted conversion of VBG to Roux-en-Y gastric bypass (RYGB) in a patient presenting with severe dysphagia and class III obesity. The aim is to detail the surgical approach, perioperative challenges, and outcomes of revisional bariatric surgery in a complex case. Case_presentationA 72-year-old female with a history of open VBG, open revisional banding, and median incisional hernia repair with synthetic mesh presented with weight regain (BMI 41.3 kg/m²) and severe dysphagia. The preoperative workup (abdominal CT scan, gastroscopy, and barium study) confirmed the presence of proximal stenosis of the stomach and a gastro-gastric fistula. A robotic-assisted revisional surgery was undertaken, requiring extended adhesiolysis. After resection of the fundus of the stomach, a conventional RYGB was performed. On postoperative day 4, the patient required reoperation due to a jejuno-jejunal anastomosis stricture caused by kinking from a long and adherent barbed suture tail. The anastomosis was revised and widened with mechanical suturing. Intraoperative gastroscopy confirmed a patent gastro-jejunal anastomosis without leaks. A perianastomotic abscess developed postoperatively, likely due to intraoperative contamination, but it was successfully managed with percutaneous drainage and intravenous antibiotics. The patient recovered well, with resolution of dysphagia and initial weight loss at follow-up. ConclusionRobotic-assisted conversion of VBG to RYGB is an effective technique for managing weight regain and dysphagia, though its complexity entails significant risks for complications. This case underscores the importance of meticulous surgical technique, contamination prevention, and vigilant postoperative care. Robotic technology, combined with a multidisciplinary approach, serves as a valuable asset for optimizing outcomes in complex revisional bariatric surgery. 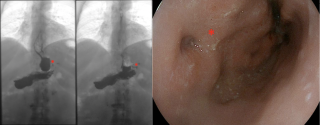
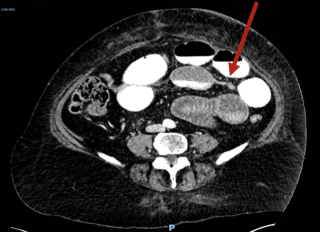

|
||
|
PSGVC54
Melanoma metastasis to the thyroid: an uncommon finding
Nelly Gauderon, Villars / Fribourg
AbstractBackgroundMetastasis to the thyroid gland from non-thyroid primary tumors is uncommon, accounting for an estimated 1-3% of all thyroid malignancies. The most common sources of metastasis are lung cancer and renal cell carcinoma with cutaneous tumors making up only 4% of all primary origins. Due to its low incidence and limited number of reported cases, no consensus established on the management and role of surgery. Surgery is typically considered for local symptom control or with curative intent in selected patients. AimsTo present a case of metastatic melanoma to the thyroid gland highlighting the diagnostic and therapeutic approaches involved. MethodsA 76 year old male patient, with a history of cutaneous elbow melanoma diagnosed 7 years earlier and a small intestinal resection for intestinal metastasis 2 years prior, presented suspicious lesions in the left thyroid and right lung on PET-CT scan. Biopsies confirmed melanoma metastasis. Systemic therapy with Ipilimumab and Nivolumab was initiated but discontinued after one cycle due to polymyalgia. A follow-up PET-CT scan showed a persistent thyroid lesion. After multidisciplinary discussion, a surgical metastasectomy was recommended due to the patient’s good condition and limited disease extent. ResultsA left thyroid lobectomy was performed and the patient discharged on postoperative day 1. Histopathology confirmed metastatic melanoma. The patient showed no recurrence of disease at 3 and 6 months. ConclusionMetastasis to the thyroid from non-thyroid tumors are rare and can manifest at initial presentation, during follow-up, or as a new presentation. The surgical indication for thyroid metastasis depends on disease status, the patient’s general conditions and symptoms caused by the thyroid mass necessitating case-by-case discussion in a multidisciplinary setting. The surgical goal is the removal of the gross tumor with negative margins; most experts recommend lobectomy or isthmectomy for isolated nodules and total or near-total thyroidectomy in multifocal disease without prophylactic neck dissection. 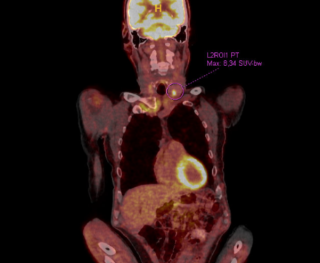
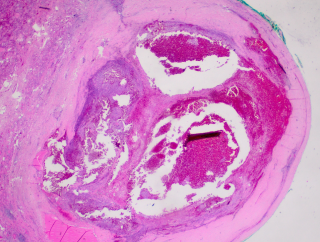
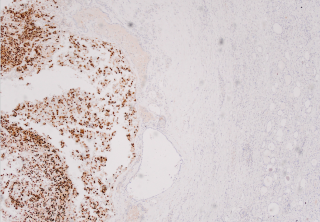
|
||
|
PSGVC55
Composite Adrenal Tumor with Coexisting Cortisol-Secreting Adenoma and Melanoma Metastasis: A Case Report and Literature Review
Davide Schiavi, Lugano
AbstractBackgroundAdrenal incidentalomas (AIs) are asymptomatic adrenal masses often detected incidentally during imaging. While most AIs are benign, some require intervention due to malignancy or hormone secretion. Metastasis of melanoma to the adrenal gland is rare and not well documented. This report describes an unusual case of a composite adrenal tumor, featuring a cortisol-secreting adenoma with a melanoma metastasis. Case_presentationWe report the case of a 77-year-old woman with a history of duodenal melanoma and low-grade B-cell lymphoma was found to have an adrenal incidentaloma, with suspicious FDG tracer accumulation on PET/CT corresponding to an 8 mm lesion without suspicious characteristics inside a 3 cm adrenal mass on MRI. Preoperative hormonal workup revealed ACTH-independent subclinical Cushing's syndrome, and the patient underwent adrenalectomy with perioperative cortisol replacement. The postoperative course was uneventful. Histological analysis identified a melanoma metastasis within an adenoma. Immunohistochemical staining confirmed melanoma markers (Melan-A, S100, PRAME). Follow-up imaging revealed no additional metastatic disease at three months. ConclusionThis case highlights the complexity of managing composite adrenal tumors, combining hormone secretion and metastasis. While 10-12% of AIs secrete cortisol, metastatic involvement, especially from melanoma, is rare. Hormonal evaluation allowed for precise preoperative planning and guided perioperative management, emphasizing the importance of an evidence-based approach. This case serves as clinical example of managing rare adrenal pathologies with implications for advancing the treatment of composite adrenal tumors.
I declare that there are no conflicts of interest related to this abstract. |
||
|
PSGVC56
Composite Pheochromocytoma-Ganglioneuroma: A Case Report
Valérian Tanner, Fribourg
AbstractBackgroundComposite pheochromocytoma (CP) are rare neoplasms originating from neural crest cells, combining chromaffin cells (typically found in pheochromocytoma) with neuronal tumors such as ganglioneuroma (62%), ganglioneuroblastoma (16%), neuroblastoma (11%), or schwannoma (1%). Fewer than 100 CP cases have been reported, with 27% presenting a genetic syndrome, including neurofibromatosis 1 (19%), MEN 2A (4%), von Hippel Lindau syndrome (2%), and watery-diarrhea hypokalemia-achlorhydria (2%). This case report presents a CP, discussing its atypical presentation, surgical treatment, and histopathological findings. Case_presentationA 43-year-old woman with a family history of neurofibromatosis type 1 was admitted to our emergency department with acute coronary syndrome and Menard's triad (headaches, palpitations, and sweating). Coronarography suggested Tako-Tsubo syndrome. Subsequent ambulatory work-up revealed elevated urinary metanephrines and cortisol levels. Abdominal CT showed a heterogeneous right adrenal mass (52x45x52mm). 123I-meta-iodobenzylguanidine scintigraphy and 18-F DOPA PET-CT confirmed the lesion was compatible with pheochromocytoma, with no evidence of metastatic disease. Elective laparoscopic right adrenalectomy was marked by a hypertensive state before and hypotension immediately after resection, with a good response to IV infusions. Histopathology revealed a CP with ganglioneuroma (Figure 1). The pheochromocytoma component's immunohistochemistry was positive for chromogranin A and negative for neurofilament, while the ganglioneuroma component was positive for neurofilament and negative for chromogranin A. Both components exhibited low mitotic activity (1% Ki-67 index) and were negative for inhibin and MelanA (markers for the residual medulla and adrenal cortex, respectively). Blood cortisol levels normalized by day 2. The in-hospital follow-up was uneventful, and the patient was discharged on day 6. At a 6-week follow-up, she was asymptomatic. Given the metastatic risk despite complete resection, endocrinology follow-up was organized. ConclusionCP is a rare tumor, diagnosed through histopathology, that shares its treatment approach with typical pheochromocytomas. However, the rarity of cases leads to uncertainty in prognosis, emphasizing the need for lifelong clinical and biochemical follow-up. 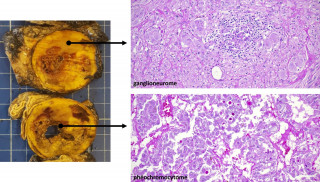
|
||
|
PSGVC57
Minimally Invasive Lateral Cervical Approach for Retropharyngeal Lymph Node Metastasis in Differentiated Thyroid Carcinoma
Bastien Picut, Genève / Geneva
AbstractBackgroundRetropharyngeal lymph node metastases (RPLNs) are rare in differentiated thyroid carcinoma (DTC), occurring in 0.43–5% of cases, typically in recurrent or persistent disease. Surgical management of RPLNs is challenging due to their proximity to vital structures, and conventional approaches are associated with significant morbidity. AimsThis case report highlights a minimally invasive lateral cervical approach for RPLN resection, focusing on its safety, efficacy, and functional outcomes. MethodsA 22-year-old female with papillary thyroid carcinoma underwent total thyroidectomy and bilateral neck dissection for a tall cell variant of DTC. Following radioactive iodine (RAI) therapy, disease progression resulted in recurrent metastases in the left RPLN. Imaging confirmed intense fixation in the left RPLN and Level II–III nodes. Surgical resection was performed using a minimally invasive lateral cervical approach, carefully avoiding involvement with complex nearby structures. The metastatic RPLN was successfully removed. The patient experienced transient marginal mandibular nerve palsy, which resolved spontaneously and she did not develop dysphagia or any other neurological deficits. Postoperative pathology confirmed metastatic papillary carcinoma. ResultsThis case demonstrates the feasibility and efficacy of a minimally invasive lateral cervical approach for RPLN metastases in DTC. Traditional approaches, such as transoral and transcervical techniques, are associated with high morbidity, including cranial nerve injuries and dysphagia. In contrast, the minimally invasive approach reduces dissection, minimizes complications, and provides effective oncologic control. The use of intraoperative nerve stimulation was critical in preserving neural function, with only transient complications observed. ConclusionThe minimally invasive lateral cervical approach is a safe and effective alternative to traditional methods for retropharyngeal lymph node dissection. By reducing morbidity and preserving function, it offers a promising option for managing complex metastatic thyroid cancer cases, particularly in young patients requiring multiple interventions and prolonged follow-up. 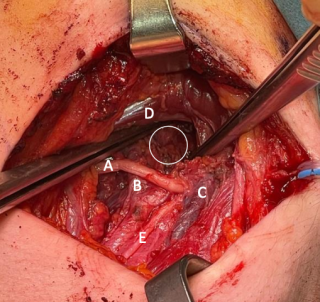
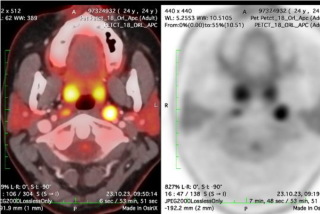
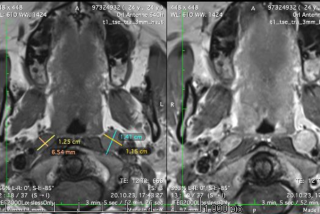
|
||
|
PSGVC58
Life-Threatening Hemorrhagic Shock From a Ruptured Pancreaticoduodenal Artery Aneurysm: An Unusual Clinical Presentation
Gayani Gunawardena, Genève
AbstractBackgroundPancreaticoduodenal artery aneurysm (PDAA) accounts for < 2% of all visceral aneurysms often associated with celiac trunk stenosis, itself often caused by a hypertrophic arcuate ligament. PDAA can rupture unexpectedly and cause a life-threatening emergency. Its rare and unspecific presentation makes early diagnosis and management challenging, especially in critically unstable patients. Case_presentationA 61-year-old healthy man presented with sudden epigastric pain, nausea, and modified EKG, suggesting a myocardial infarction. He underwent an emergency coronary angiography, which ruled out any cardiac issues. However, he became critically unstable with signs of hypovelomic shock and was rushed to the emergency room for resuscitation. Bedside extended focused assessment with sonography for trauma (E-FAST), revealed free intraperitoneal fluid. An emergency exploratory laparotomy was performed, without preoperative CT imaging. Intraoperative findings included massive hemoperitoneum and retroperitoneal hematoma. A supra-coeliac aortic clamping allowed stabilization of the patient. Exploration revealed a ruptured PDAA, causing destruction of the head of the pancreas. A total pancreatectomy was performed. A laparostoma was placed, allowing for 2 days of fluid resuscitation in the intensive care unit. CT scan demonstrated a hypertrophic arcuate ligament with hemodynamic repercussion, confimed by Doppler ultrasound. Therefore, digestive and biliary reconstruction was performed during second look surgery, associated with the release of the arcuate ligament. The postoperative recovery was uneventful. ConclusionSudden abdominal pain and shock in a healthy patient often point to septic shock from digestive perforation, hypovolemic shock from a ruptured abdominal aneurysm, or severe dehydration from bowel obstruction. CT angiography remains the gold standard for diagnosing aneurysms, which require treatment (open or endovascular) if their anteroposterior diameter exceeds 2 cm. Inspiratory and expiratory vascular imaging determines whether arcuate ligament release is necessary. This case highlights the importance of considering visceral aneurysm rupture in sudden abdominal pain with shock; immediate surgery and awareness of PDAA etiologies are crucial. |
||
|
PSGVC59
Volvulus of the Gallbladder
Soufiane Chami, Geneva
AbstractBackgroundCholecystectomy is one of the most frequently performed abdominal surgical procedures, indicated for gallstones disease, polyps, and, exceptionally, for volvulus of the gallbladder. Nowadays, laparoscopy is the gold standard approach for cholecystectomy due to reduced operative pain, shorter hospital stays and better cosmesis compared to open surgery. The most frequent complication of this surgery compared to open surgery is an injury of the common bile duct, even if various measures implemented overt time mitigated the occurrence. Case_presentationWe report the case of an 86 year old female presenting to the emergency department with mild diffuse abdominal pain and constipation. Blood tests showed no signs of inflammation. A CT-scan showed vesicular hydrops and fecal impaction in the colon. She was given an enema and was discharged. She came the next day with significant worsening of the pain, localized now in the right upper quadrant without nausea, vomitting or fever. The white blood cell count was at 13.9 G/l and serum CRP at 186 mg/l with mild cytolysis and cholestasis without elevation of the bilirubin. The new CT-scan showed signs of a volvulus of the gallbladder with ischemia and perforation. The patient underwent a laparoscopic exploration which confirmed a volvulus of the gallbladder with intraperitoneal liquid but without franc perforation. A flabby peritoneum was the most probable explanation for the volvulus. A cholecystectomy was performed without complication. Post-operative recovery was uneventful under 48h of parenteral ceftriaxone-metronidazole. Histopathologic results showed necrosis of the gallbladder without gallstones. ConclusionThis case shows the importance to recognize the radiological features and the clinical awarenes for a good global management of the patients resulting in good outcomes. 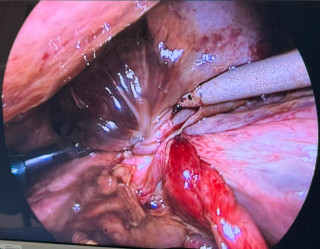
|
||
|
PSGVC60
Implementing a surgical robotic program in a tertiary center for pancreatic surgery: learning curve for pancreaticoduodenectomy
Charles-Henri Wassmer, Geneva
AbstractBackgroundRobotic-assisted surgery has revolutionized complex procedures, offering improved precision, and enhanced recovery. However, implementing a robotic surgical program is associated with unique challenges, including cost, expertise, and patient volume, especially for complex surgeries such as the pancreaticoduodenectomy (PD). AimsWe aimed to describe the learning curve for complex pancreatic robotic surgery MethodsWe performed a retrospective analysis of all robotic-assisted PD since the initiation of the pancreatic robotic program in our center. We divided the cohort in two eras, early and late, representing the first and more recently performed cases, respectively. We compared our results to the established benchmarks for open PD (Sánchez-Velázquez et al. Ann Surg 2019). It is noteworthy to mention that these benchmarks have been established on a large cohort of low-risk patients in term of comorbidities and complexity of the tumors, when our cohort includes all patients, regardless of patient and tumor characteristics. ResultsA total of 34 PD were performed in our center. Thirteen in the early group and 21 in the late group. Most patients presented with pancreatic duct and ampullar adenocarcinoma. Conversion rate to open surgery was 11.8 %. Operative time was significantly reduced in the late group. Among the 13 benchmarks points explored in our study, 12 were within the benchmarks in the late group with exception for length of hospitalization (Table 1). We reported no in-hospital mortality and no major bleeding. ConclusionRegardless the surgical approach, PD remains a complex procedure. Implementing a surgical robotic program requires a significant surgical expertise in open and robotic surgery. Our results demonstrate that almost all benchmark objectives could be met after less than 15 procedures, despite the fact that we compared our patients, regardless of their clinical and tumor characteristics, with low-risk patients used to established the benchmarks. 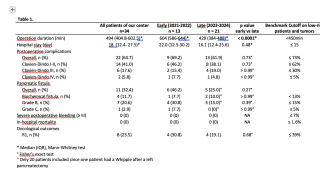
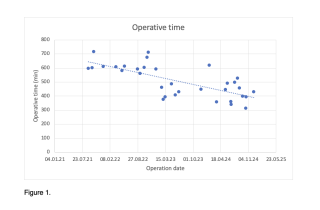
|
||
|
PSGVC61
Resistant Bile Microbes: Harmless Hitchhikers or Potential Threats in Pancreatic Surgery?
Annatina Weber, Baden / 5404
AbstractBackgroundRecent studies recommend piperacillin-tazobactam prophylaxis before pancreatoduodenectomy to prevent surgical site infections (SSI), suggesting that contaminated bile may foster SSIs through bacterial resistance to common single-dose antibiotics. AimsThis study aims to assess the impact of resistant organisms in intraoperative bile samples (ROBS) on SSIs and other complications in pancreatic surgery. MethodsData of consecutive patients undergoing pancreatic resections between January 2015 and December 2023 were retrospectively analyzed. Pancreatic resections involving bilioenteric anastomosis with intraoperative bile sampling were included. ResultsIntraoperative bile samples were obtained in 103 pancreatoduodenectomy- and 19 total pancreatectomy patients. ROBS were identified in 68 patients. Patients with and without ROBS had a comparable mean age of (71 vs. 69 years) and median BMI (24 each). Cholangiocarcinoma was more frequent in the ROBS-group (21% vs. 3%, p=0.004). Preoperative biliary drainage was common among ROBS patients (ERCP: 83% vs. 12%, p<0.001; PTCD: 7% vs. 0%, p<0.001). Among the 59 patients without ROBS, 52 had sterile bile samples. The majority in both groups received a single-dose combination of cefuroxime and metronidazole preoperatively (85% vs. 86%, p=0.884). ROBS predominantly contained Enterococcus faecalis (71%), Enterococcus faecium (32%), and Enterobacter cloacae (31%).
Superficial, deep, and organ-space SSIs occurred at comparable rates (9%, 6%, and 18% vs. 5%, 5%, and 18%, respectively). Similarly, there was no difference in pancreatectomy specific complications like postpancreatectomy pancreatic fistula. Severe complications graded according to Clavien-Dindo were present in 33% vs. 37% of patients with a similar 90-day mortality rate of 4% vs. 7% (p=0.704). ConclusionDespite the presence of resistant organisms in bile samples, SSIs, POPF, and overall morbidity were not significantly increased when patients received single-dose prophylactic cefuroxime and metronidazole before pancreatectomy
|
||
|
PSGVC62
Two Cases of Ciliated Hepatic Foregut Cyst
Isabella Hunjan, Lugano
AbstractBackgroundCiliated hepatic foregut cysts (CHFCs) are rare entities with less than 150 cases reported in the literature. They are due to the persistence of aberrant embryonic foregut epithelium typically in the S4 of the left liver. Despite being benign lesions, often incidental in asymptomatic patients, CHFCs are at risk of malignant transformation into squamous cell carcinoma. Surgical resection is the only potential curative option. Case_presentationTwo cases of CHFCs were incidentally found in asymptomatic male patients and confirmed at final pathology. Patient 1: 19-year old male with recurrence of aspecific abdominal pain. Abdominal US revealed a hypoechoic hepatic cyst at S4a and MRI confirmed a 21 x 12 mm bilobated hypointense lesion on T1-weighted sequences and hyperintense on T2-weighted imaging, consistent with CHFC. Patient 2: 59-year old male with liver cirrhosis AHS-NASH related was found with a S8/4a cyst during a screening work-up. MRI showed a 28 x 16 mm cystic lesion with a mixed solid-liquid content and contrast enhanced on T1-weighted imaging. Echinococcosis serology was negative twice. After multidisciplinary discussion, parenchymal sparing hepatic resection was suggested. In both cases, infectious diseases were excluded. After multidisciplinary discussion, a minimally invasive parenchymal sparing hepatic resection was suggested. Indeed, S4a wedge resections were performed with an uneventful recovery. Final pathology was consistent with CHFC for both, reporting as follow: Patient 1: 2 cm cyst with columnar pseudostratified epithelium, partially ciliated, with a muscular out layer, no atypia and no malignant features. Patient 2: 2.5 cm biloculated cystic lesion with monostratified epithelium without atypia, partially ciliated, with a subepithelial smooth muscle layer and connective tissue layer. ConclusionConsidering the potential malignant transformation, surgical resection is safe and feasible to achieve definitive diagnosis and cure. 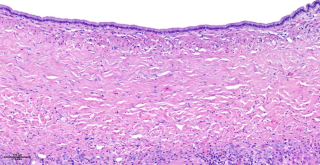

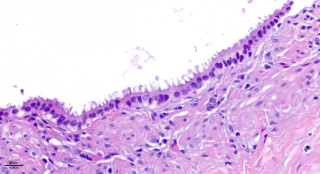
|
||
|
PSGVC63
Surgical Management of Solitary Gallbladder Metastasis From Melanoma: An Illustrated Case Report
Michaella Florent, Lausanne / Rennaz
AbstractBackgroundMelanoma is the deadliest form of skin cancer, with a 5-year survival rate of 32% for patients with distant metastases. Gastrointestinal metastases occur in less than 4% of cutaneous melanoma cases, and gallbladder metastases are exceedingly rare. Fewer than 10 cases of solitary gallbladder metastasis have been reported in the literature, with no standardized therapeutic guidelines. Case_presentationA 76-year-old patient, initially diagnosed in November 2022 with ulcerated melanoma (Clark IV, Breslow 5mm, pT4b cNx cM1a), underwent surgical excision and mediastinal metastasis resection in early 2023, followed by adjuvant pembrolizumab immunotherapy for a year. In late April 2024, after treatment completion, a control PET-CT revealed a suspicious gallbladder lesion, confirmed by MR cholangiography. Laparoscopic cholecystectomy was performed in May 2024, and pathology confirmed metastatic melanoma. Post-surgery, combined ipilimumab-nivolumab immunotherapy was initiated within days. ConclusionGallbladder metastases are typically associated with widespread disease and abdominal symptoms. Solitary lesions, as in this case, are extremely rare, contributing to a lack of consensus on treatment. While open cholecystectomy is often recommended to prevent port-site or peritoneal seeding, a laparoscopic approach may be appropriate for isolated metastases. In this case, minimally invasive surgery allowed rapid recovery and timely initiation of adjuvant immunotherapy. This report underscores the importance of individualized treatment strategies in rare melanoma metastases. 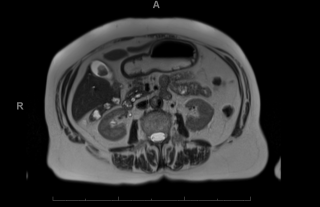
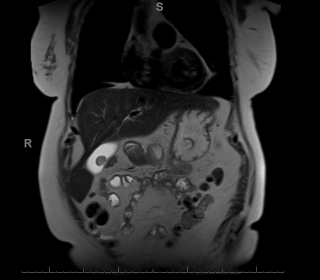
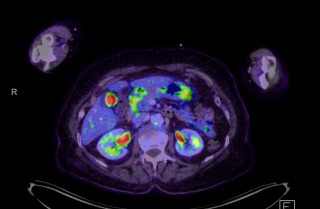
|
||
|
PSGVC64
Endoscopic Resection of Intraductal Papillary Mucinous Neoplasm of the Bile Duct: The First Case Report
Gioia Pozza, Lugano
AbstractBackgroundIntraductal papillary mucinous neoplasm of the bile ducts (IPMN-B) are pre-cancerous growth of mucin-secreting epithelium arising from the biliary tree. They have a variable risk of progressing to cholangiocarcinoma and the treatment depends on size, location, symptoms, and likelihood of malignancy. Management includes follow-up, curative strategies such as surgical resection and liver transplantation, or the palliation of symptoms with endoscopic or percutaneous biliary stenting. Case_presentationAn 87-year-old female with Lynch syndrome and a complex oncological history—including ovarian adenocarcinoma, colon adenocarcinoma, and triple-negative breast cancer—developed recurrent cholangitis following extended right hepatectomy performed in 2019 for hilar cholangiocarcinoma (Bismuth3A, pT1N1M0R0). MRI revealed images of intraductal masses, associated with upstream biliary dilation of the left biliary duct. At multiple biopsies, low- and high-grade IPMN-B were found. Given the patient's advanced age, comorbidities, and refusal of major surgery, a novel approach was undertaken. Endoscopic resection with a diathermic loop, an approach not previously reported in the literature, was successfully performed. Follow-up at six months demonstrated excellent outcomes, including the absence of new episodes of cholangitis, preserved hepatic function, unremarkable MRI, and negative tumor markers. ConclusionThis groundbreaking case highlights the feasibility of endoscopic resection for IPMN-B in select patients as a minimally invasive alternative to surgery or biliary stenting. The findings emphasize the potential for innovative, patient-centered approaches to complex biliary conditions, warranting further exploration and validation in broader clinical practice. |
||
|
PSGVC65
Migration of Hem-o-Lok Clips in the Common Bile Duct: a Very Unusual Late Complication after Laparoscopic Cholecystectomy
Eleonora Garosi, Lugano
AbstractBackgroundLaparoscopic cholecystectomy (LC) is the gold standard treatment for symptomatic gallstones. Late complications following LC (i.e., >3 months) occur in fewer than 1% of cases. These typically include stones or inflammation of the cystic stump, common bile duct (CBD) stones, CBD strictures, neuromas and incisional hernias. Clip migration into the CBD has also been reported, but recommendations about its management are lacking. Case_presentationThis report describes the management of a highly unusual case of delayed complication after LC: Hem-o-Lok clip migration into the CBD. A 78-year-old woman presented with fever and a confusional state. Two years earlier, the patient had undergone endoscopic retrograde cholangio-pancreatography (ERCP) followed by LC for acute obstructive gallstone cholangitis. Laboratory tests on admission revealed an inflammatory syndrome characterized by elevated neutrophil count and C-reactive protein (CRP). Liver function tests were normal. Imaging studies, including abdominal CT scan and magnetic resonance cholangiopancreatography (MRCP), identified a suspected foreign body within the CBD. Diagnostic ERCP was performed. ERCP confirmed the presence of two migrated clips within the CBD, which were successfully retrieved. These clips were identified as the source of the patient’s symptoms, which completely resolved following the procedure. Follow-up imaging showed no residual obstruction or complications. Revision of the literature showed 36 similar cases, of which 22 with Hem-o-lock, 9 managed endoscopically. ConclusionAlthough rare, post-cholecystectomy clip migration (PCCM) is a relevant complication that may lead to stone formation, obstructive jaundice, cholangitis, biliary colic, Mirizzi syndrome, fistula, and acute pancreatitis. Prompt diagnosis with advanced imaging techniques, resting on the awareness that the condition exists, combined with endoscopic treatment, appears to be the proper modern management. |
||
|
PSGVC66
Perioperative Real Time Glucose Assessment as a Predictive Tool for Complications After Pancreatic Resection- A Prospective Single Center Pilot Study
Felix Bussmann, Winterthur
AbstractBackgroundPostoperative hyperglycaemia was described as an early marker for complications after pancreatic resection. Nevertheless, evidence heavily relies on retrospective assessment of arbitrary serum blood sugar measurements. In contrast, continuous glucose monitoring (CGM) systems allow real-time monitoring of glucose fluctuations. AimsThe aim of this study was to examine continuous perioperative glucose changes after pancreatic resections and the impact these changes have on postoperative complications. MethodsProspectively, twenty (n=20) consecutive patients undergoing pancreatic resection were included. Additionally, n=5 patients undergoing other major abdominal surgeries served as control group. The Dexcom G6 CGM system was utilized. Time in euglycemic Range (TIR) and peak glucose levels were analyzed. Furthermore, routine serum glucose measurements and daily C-reactive protein (CRP) levels were assessed. Comprehensive Complication Index (CCI) was used to quantify postoperative complications.
ResultsNo adverse event was observed related to CGM devices. Glucose levels significantly increased from a median 7mmol/l (IQR 6-8mmol/l) to 9 mmol/l (IQR 8-1mmol/l, P=0.026) after pancreatic resection. Accordingly, the TIR decreased from 86.5% (IQR 85-96%) to 78.1% (IQR 34-89%, p=0.042). Perioperative glucose levels (p=0.623) and TIR (p=0.408) remained unchanged in the control group. Linear regression showed a significant correlation of peak glucose levels on day 1, measured by CGM (R=0.738, p=0.004, Figure 1A), and CRP levels on day 2 (R=0.528, p=0.034, Figure 1B) with CCI. In contrast, routine serum glucose levels failed to predict complications. ConclusionIn this pilot study, peak glucose levels on day 1 after pancreatic resections were associated with adverse events. CGM may be a valuable tool to detect patients at risk for complications.

|
||
|
PSGVC67
Laparoscopic-Assisted Pancreatic necrosectomy (LAPN) in the Treatment of Walled off Pancreatic Necrosis: A Retrospective Study
Valérie Kremo, Luzern
AbstractBackgroundAcute infected necrotizing pancreatitis is associated with high rates of organ failure and mortality. The step-up approach which combines percutaneous drainage with laparoscopic-assisted pancreatic necrosectomy (LAPN) or transgastric drainage with necrosectomy, has reduced complications and mortality. AimsThis study aimed at comparing surgical and endoscopic step-up approach treatments. MethodsA retrospective analysis of patients with infected necrotizing pancreatitis treated using the step-up approach between 2019 and 2023 was conducted. Surgical treatment involved CT-guided percutaneous drainage followed by LAPN if needed, while the endoscopic approach used transgastric drainage and endoscopic necrosectomy as required. The primary endpoint was a composite of major complications and 6-month mortality. Secondary outcomes included complication rates, reinterventions, and duration of hospital stay. ResultsThe study included 31 patients (mean age 60.7±14.2 years). Eighteen underwent the surgical step-up approach with CT-guided drainage, followed by LAPN in 11 cases (61.1%). Thirteen received the endoscopic step-up approach with transgastric drainage, followed by necrosectomy in 7 cases (53.8%). Major complications or death occurred in 54.5% of the surgical group and 57.1% of the endoscopic group within six months. The LAPN group reported one intraoperative and six postoperative complications. In the endoscopic group were one intraoperative and six postoperative complications. Four patients required LAPN after endoscopic necrosectomy due to insufficient clinical improvement. ConclusionOur findings indicate that both LAPN and endoscopic necrosectomy are effective in controlling the local and systemic infection. While outcome analysis suggests endoscopic treatment as the preferred first-line approach, the supporting evidence is limited. LAPN remains important for managing extensive infected necrosis, particularly when endoscopic methods cannot fully address the infection or when there is no direct contact between the infected area and the gastric wall. |
||
|
PSGVC68
Prolonged antibiotic prophylaxis do not impact perioperative outcomes after pancreatoduodenectomy in patients with biliary stent. A Propensity Score and Mediation Analysis
Marie Klein, St. Gallen
AbstractBackgroundWhether the use of prolonged antibiotic prophylaxis (PAP) enhances the outcomes of pancreaticoduodenectomy (PD) in patients with preoperative biliary drainage (PBD) remains a controversial subject. AimsThis study aimed to determine whether the addition of PAP reduced infection-related complications following PD. MethodsThis study assessed patients who underwent PD with PBD at two centres. Patients in group 1 received a single dose of antibiotic prophylaxis (SDAP) prior to PD, while patients in group 2 received an additional dose of PAP. Postoperative complication rates were compared using bipartite propensity score matching and weighting (PSM), Cox regression and mediation analysis. ResultsOf the total participants, 57.5% (n=119) were female with a median age of 67.5 (IQR 11.6) years. Multivariable analysis rates showed that PAP did not result in a reduction of superficial SSI (OR 1.23, 95% CI: 0.77-1.96; P=0.393). There were no significant differences found between PAP and SDAP for deep incision SSI (4.3% vs. 4.3%; P=0.861), deep organ SSI (10.1% vs. 15.2%; P=0.358), and pneumonia (15.9% vs. 9.4%; P=0.163). The study found that PAP was linked to higher 30-day postoperative mortality (OR 2.42, 95% CI: 2.36-2.47; P<0.001) and 90-day readmission (OR 2.02, 95% CI: 1.19-3.44; P=0.009). Both groups had similar rates of POPF grade B (11.6 vs. 12.3%; P=0.096), POPF grade C (10.1 vs. 6.5%; P=0.096), PPH grade B (1.4 vs. 4.3%; P=0. 332), PPH grade C (10.1 vs. 7.2%; P=0.332), DGE (39 vs. 36.2%; P=0.438), bile leak (7.2 vs. 2.9%; P=0.158) and gastric anastomotic leak (2.9 vs. 0.7%; P=0.368). The duration of surgery, age, immunosuppression, and history of cholangitis did not significantly affect the relationship between PAP and SSI (P > 0.05). ConclusionOur analysis based on PSM and mediation suggests that SDAP may effectively prevent postoperative infectious complications in patients with PBD undergoing PD. As a consequence, we do not recommend PAP therapy as a routine for such patients. |
||
|
PSGVC69
Gallbladder duplication: A case report
Panagiotis Spiliotis, Bern
AbstractBackground
Case_presentationWe report the rare case of a double gallbladder type 1 according to Harlaftis in a 67-year-old male patient admitted with wall thickening of the gallenbladder and cholelithiasis, detected by endosonography during the work-up of recurrent pancreatits and suspected IPMN. Preoperative imaging with MRI Cholangiographie detected gallbladder duplication with cholelithiasis. The patient underwent laparoscopic cholecystectomy which revealed a double gallbladder with a single cystic duct and two cystic arteries, all divided between clips. Cholecystectomy was completed laparoscopically. Huge gallstones were revealed, but only in one of the two gallbladders. By pathology, a V-septated duplicated gallbladder according to Harlaftis type 1 with chronic cholecystitis was confirmed. ConclusionDuplication of the gallbladder is a rare congenital anomaly of the biliary system with the incidence of 1 in 3800, which requires special attention and emphasis to avoid surgical complications. The classification of Harlaftis dicriminates the types 1 to 4. Concomittant anomalies of the arterial blood supply are common. Laparoscopic cholecystectomy remains the preferred method of treatment after clarifying the biliary anatomy by endosonography and MRCP or ERCP. |
||
|
PSGVC70
Scirrhous Hepatocellular Carcinoma: Case Report of a Rare Subtype of Hepatocellular Carcinoma, a Challenge in Diagnosis and Treatment
Sara Pereira de Sousa, Sion
AbstractBackgroundAbout 90% of primary liver malignancies are Hepatocellular Carcinoma (HCC). Rare subtypes of HCC represent 20-30% of all HCCs. Scirrhous HCC is a rare subtype with a prevalence of 0.2 to 4.6% mainly arising in hepatitis- or cirrhosis-afflicted livers, recently recognized as a subtype of HCC in the WHO classification. It is characterized by cords of cancerous cells in a rich fibrous stroma often misdiagnosed as cholangiocarcinoma, metastasis or fibrolamellar HCC. Due to scarcity of publications there is conflictual data, mainly provided by Asian centers (45% of articles from Japanese Centers). However a recent systematic review and pooled data analysis reports a poorer overall survival and a worse prognosis. AimsTo contribute to the literature by documenting a European case of a very rare subtype of HCC with conflictual data mainly provided by Asian centers. MethodsWe report a case of a patient with a scirrhous HCC developed in a non-cirrhotic liver but with a medical history of eradicated HCV infection and HIV infection under treatment. ResultsA 63-year-old female patient mainly known for a treated HIV infection (undetectable viremia), successfully eradicated HCV infection and diffuse interstitial pneumopathy due to tobacco smoking. A follow-up CT-scan for a solitary pulmonary nodule revealed an incidental finding of a unique liver lesion. Proper abdominal CT-scan and MRI showed a 4 cm segment IVB lesion with radiological features of cholangiocarcinoma (Figure 1). We performed a percutaneous biopsy of the lesion that revealed scirrhous-subtype HCC. We pursued with a transjugular liver biopsy with the gradient measurement (3 mmHg). The histological result was within normal limits. The patient had a segment IV resection by modified Makuuchi laparotomy. ConclusionAn increase in scientific reports from different parts of the world regarding rare sybtypes of HCC could lead to a more comprehensive analysis of these rare malignancies often asociated with a worse prognosis. 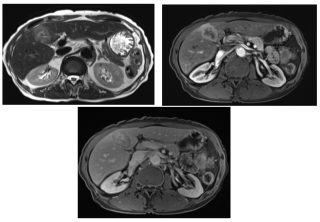
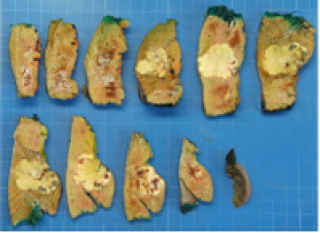
|
||
|
PSGVC71
Cholangiocarcinoma? Don’t Skip The IgG4
Hassan Youssef, Genève / Geneva
AbstractBackgroundImmunoglobulin G subclass 4 (IgG4)-related disease (IgG4-RD) is a rare immune-mediated fibroinflammatory disorder, with an estimated prevalence of 0.78–1.39 cases per 100,000 individuals. Initially identified in association with Type I autoimmune pancreatitis (AIP), IgG4-RD has since been recognized as a systemic condition potentially affecting nearly all organ systems, especially the biliary tree. Histologically, affected tissues typically demonstrate tumor-like lesions with dense lymphoplasmacytic infiltrates rich in IgG4-positive plasma cells, storiform fibrosis, obliterative phlebitis, and increased eosinophilic infiltration. Case_presentationWe herein report the case of a 66-year-old male with progressive jaundice and weight loss, initially suspected of having perihilar cholangiocarcinoma. A multimodal diagnostic strategy was employed, integrating advanced imaging modalities, comprehensive laboratory investigations, cytological evaluations, and input from a multidisciplinary team of specialists. This approach enabled the identification of hallmarks of IgG4-SC, such as elevated serum IgG4 levels and imaging findings consistent with autoimmune pancreatitis, while ruling out malignancy through cytology and histopathological analysis. The collaborative multidisciplinary discussions were pivotal to establish a definitive diagnosis of IgG4-SC associated with type I autoimmune pancreatitis. The patient responded favorably to corticosteroid therapy, and immunosuppressive therpay. ConclusionThis case underscores the importance of an interdisciplinary approach and the use of evidence-based medical interventions to navigate the diagnostic and therapeutic complexities associated with IgG4-SC. It further illustrates the importance of clinical awareness and precision in distinguishing IgG4-SC from malignancies, such as perihilar cholangiocarcinoma, to optimize patient outcomes and reduce the risk of unnecessary invasive procedures. 
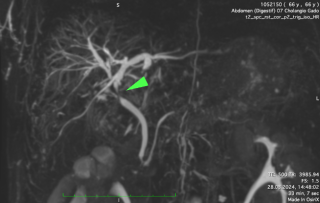
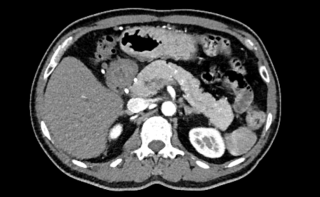
|
||
|
PSGVC72
Intraoperative Left Hepatic Branch Artery Aneurysm Rupture During Cholecystectomy: A Case Report Of A Rare and Potentially Lethal Diagnosis
Alexis Poirier, Genève
AbstractBackgroundHepatic artery aneurysm (HAA) is a rare (0.002%-0.4%) but life-threatening condition. HAA represents the second most frequent visceral aneurysm. The incidence is approximately 20%, with a reported rupture rate up to 44%. The literature describes some risk factors as atherosclerosis, trauma, infection, connective tissue disorders, or iatrogenic. The natural history remains unclear; from asymptomatic to abdominal pain, gastrointestinal symptoms, or obstruction of the biliary tract. Cross-sectional vascular imaging (CTA-MRI) is the imaging modality of choice. Management strategies lack consensus and are guided by symptoms, aneurysm size, and rupture status, ranging from observation to endovascular or surgical interventions. We report a case involving the incidental discovery of hemoperitoneum caused by a ruptured HAA during laparoscopic cholecystectomy. Case_presentation82-year-old female presenting in the ER with a 10-day upper right quadrant pain, vomiting, and fever. Physical exam revealed a positive Murphy sign associated with increased inflammatory markers. CT scan confirmed acute calculous cholecystitis and laparoscopic cholecystectomy was indicated. Intraoperatively, perihepatic hemoperitoneum was observed with sclero-atrophic calculous cholecystitis. Removal of clots on the hepatic pedicle unraveled massive spontaneous arterial bleeding requiring artery clamping and laparotomy. At laparotomy, bleeding was found to arise from a ruptured aneurysm of the left branch of the hepatic artery. Repair of the artery was neither possible. The left branch of the hepatic artery was removed with the aneurysm, and cholecystectomy was performed. The postoperative course was uneventful. Whole-body CTA additional arterial malformations and a gastro-duodenal artery aneurysm. Fulll vascular work-up ongoing, the rupture aneurysm etiology remains unclear. ConclusionIdentification of HAA is crucial due to its life-threatening complications. Our case illustrates the unpredictable nature of HAA, with an incidental intraoperative hemoperitoneum during laparoscopic cholecystectomy revealing HAA rupture. Bleeding control, conversion to open surgery, and artery removal are essential,while arterial repair should not be attempted unless it can be performed on macroscopically normal tissues. 
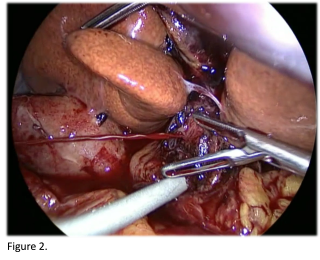
|
||
|
PSGVC73
Drug-Induced Cirrhosis Complicated by a Primary Liver MALT lymphoma: Case Report of a Rare and Often Misdiagnosed Liver Malignancy
Cátia Felgueiras Gaudêncio, Sion
AbstractBackgroundPrimary hepatic lymphoma (PHL) represents 0.4% of extranodal non-Hodgkin lymphoma (NHL) and 0.016% of all NHLs. Primary liver MALT lymphoma represents 2.9% of all PHLs. To date, the literature reports six cases of primary liver MALT in the presence of cirrhosis. In such cases, it is often misdiagnosed as hepatocellular carcinoma (HCC). Due to the rarity of the lesion and the absence of specific radiological features, the clinical and radiological suspicion is seldom mentioned before the treatment, which in most cases leads to surgical resection. AimsTo contribute to the literature by documenting a case of a rare primary liver malignancy, often misdiagnosed as HCC leading to surgical resection. MethodsWe report a case of a patient with a primary liver MALT in the presence of drug-induced cirrhosis. ResultsA 77-year-old female patient on Atorvastatin treatment in whom a chest CT scan revealed incidental findings suggestive of chronic liver disease. The patient was asymptomatic. The follow-up Ultrasound 8 months later showed a focal lesion in segment IV and the Fibroscan revealed Metavir F3 fibrosis. The MRI showed a 30 mm segment IV lesion with radiological characteristics of HCC (Figure 1). We performed a transjugular liver biopsy with the gradient measurement (16 mmHg). The histological result confirmed a Laennec 4B cirrhosis of toxic drug-induced origin "Atorvastatin" (Figure 2). Staging workup showed no further lesions. After discussion at HBP multidisciplinary concilium, the patient had a segment IV resection by laparotomy. Unexpectedly, the histological result revealed primary MALT lymphoma (Figure 3). ConclusionRadiotherapy and chemotherapy with Rituximab or Rituximab alone have shown promising results in the treatment of primary liver MALT, whereas after surgery, distant or local recurrence may occur. Making an accurate preoperative diagnosis of this disease is usually difficult, and percutaneous liver biopsy could be an appropriate avenue to improve the diagnostic accuracy and avoid surgical resection. 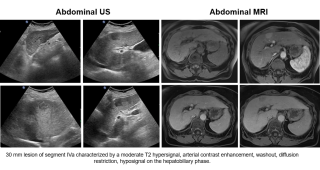
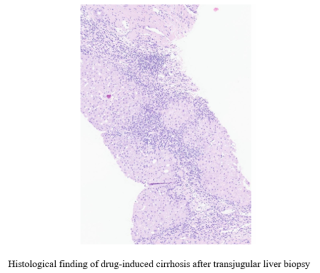
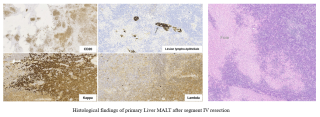
|
||
|
PSGVC74
Completion of adjuvant chemotherapy after total versus partial pancreaticoduodenectomy for pancreatic cancer – a retrospective analysis
Romy Weber, Bern
AbstractBackgroundPartial pancreaticoduodenectomy (PD) followed by adjuvant chemotherapy (AC) is the standard treatment for primarily resectable pancreatic ductal adenocarcinoma (PDAC) in the pancreatic head. Total pancreatectomy (TP) was historically reserved for selected cases due to the negative impact on quality of life (QoL) caused essentially by pancreatogenic diabetes. However, recent findings show similar outcomes including short-term morbidity, mortality and QoL, and have lowered the threshold for opting for TP over PD. By avoiding PD’s most severe complication, pancreatic fistula, we hypothesize that TP will lead to similar AC completion rates as PD even in patients with a more complex disease. AimsThe aim of our study was to investigate the initiation, timing, and completion rates of postoperative chemotherapy in patients who underwent TP for PDAC compared to those who underwent PD. MethodsWe performed retrospective analysis including all patients who underwent TP or PD for PDAC between 2014 and 2021 in our center. The rates, timing and degree of completion of AC were compared. Decision for TP vs PD was left to the discretion of the surgeon; however TP was performed for repetitive positive resection margin or tumor infiltration of the splenic vessels in most cases (59%). ResultsWe included 263 patients of those 74 underwent TP and 189 PD. TP patients had more comorbidities (liver diseases 16.2 vs 5.8%, p=0.013, diabetes 40.5 vs 24.9%, p=0.016), longer surgeries (7.2 vs. 6h, p=0.001), more frequent vascular reconstructions (77 vs. 50.8%, p=0.001), and higher blood loss (1200 vs. 600ml, p=0.001), with comparable morbidity and mortality. Rates of AC initiation (66 vs 76%, p=0.156), completion (69.4 vs 74.1%, p=0.578), and timing (7 vs 7weeks, p=0.533) were comparable. ConclusionDespite higher complexity of the cases, completion of AC after TP was comparable with PD. Advances in medical management of diabetes now support TP as a valid surgical option in high-risk situations without compromising oncological care. |
||
|
PSGVC75
COMMON BILE DUCT DUPLICATION: A RARE ANATOMICAL ANOMALY ON A 31-YEAR-OLD FILIPINO FEMALE PATIENT
Kristine Joy Flores, Valenzuela City PH
AbstractBackgroundAnatomical anomalies in the biliary system are uncommon but have a profound clinical consequences. Common bile duct duplication, for example, is an extremely rare congenital variant with significant diagnostic and surgical implications. It results from failure of regression of the embryological double biliary system and can be classified into five distinct subtypes as proposed by Choi et al. Case_presentationA 31-year-old female, ECOG 1, sought consult at the out-patient department due to occasional abdominal pain associated with jaundice, significant weight loss, anorexia and vomiting. Past medical history showed no history of previous hospitalization or surgery. Family and Personal/Social History was also unremarkable
Focused physical examination revealed soft, not distended, non tender abdomen with no palpable mass and normoactive bowel sounds. An MRCP was requested which revealed: Non-distended gallbladder with cholelithiasis. The liver has homogenous pattern with no abnormal intensity signal changes. The intrahepatic ducts are not dilated. Non-dilated, double biliary drainage with extra-hepatic communicating channels are seen, which then bifurcates into two separate distal common bile ducts prior to entering the Ampulla of Vater. The cystic duct connects with the most lateral common bile duct, located just distal to the communicating channels (Modified Choi Classification Type IV). No evidence of hypointense signal seen. The pancreas is homogenous with no abnormal intensity signal changes. The pancreatic duct is not dilated. Spleen and visualized kidneys appear intact. ConclusionCommon bile duct duplications as well as other congenital anatomic variants, though very rare, should nevertheless be a consideration pre-operatively when managing patients with obstructive jaundice. This highlights the importance of recognizing duplicated CBD both pre-operatively and intraoperatively, as an unrecognized aberrant biliary duct could be detrimential in the patient’s overall survival and quality of life post-operatively. This article aims to aid in the local and international literature review since there are very few reported cases of DCBD and actual incidence is unknown. |
||
|
PSGVC76
PANCREATIC TUBERCULOSIS MASQUERADING PANCREATIC MUCINOUS NEOPLASM: A CASE REPORT ON AN IMMUNOCOMPETENT FEMALE PATIENT
Kristine Joy Flores, Valenzuela City PH
AbstractBackgroundPancreatic tuberculosis (TB) is an extremely rare form of extrapulmonary tuberculosis even in endemic areas that masquerades as a mass or inflammation because of lack of typical clinical manifestations and radiologic features and therefore usually misdiagnosed as a pancreatic malignancy or pancreatitis Case_presentationA 43-year-old female, ECOG 0, sought consult at the out-patient department due to occasional abdominal pain, not associated with weight loss, anorexia, vomiting, fever, jaundice or changes in bowel habits. Past medical history showed controlled hypertension. A whole abdominal ultrasonography was done which noted an anechoic focus in the proximity of the pancreatic head measuring 2.1 x 1.7cm which prompted EUS-FNA of the pancreatic head mass to be done. The histopathology result was a Mucinous Neoplasm and the sampling specimen was also tested for Brown and Brenn which is negative for bacterial colonies, Periodic-Acid Schiff (PAS)which did not reveal presence of fungal elements, and tissue Acid Fast Bacilli (AFB) which is negative for tuberculosis. The preoperative CA 19-9 was within normal range. Patient underwent Classic Whipples procedure and Reconstruction was done with the following anastomosis: pancreatico-gastrostomy (dumping technique), hepatico-jejunostomy, gastro-jejunostomy, jeju-jejunostomy with an addition of feeding jejunostomy distally. Intraoperative findings were pancreatic head mass measuring 3 x 3 x 2.5cm abutting the portal vein and superior mesenteric vein. No gross liver metastasis, lymphadenopathy or suspicious peritoneal seedings noted. Final histopathologic result was consistent with pancreatic tuberculosis. Patient followed up and was already started on anti-Koch’s medications. ConclusionPreoperative diagnosis of pancreatic tuberculosis remains a challenge in cases of pancreatic masses. Clinical and radiologic ancillaries can be nonspecific, creating a cautious area for surgeons to proceed with surgical resection. A high index of suspicion coupled with preoperative tissue diagnosis and cytology are emphasized. |
||
|
PSGVC77
An Internal Hernia with an Incarcerated Ileal Loop through a Defect in the Left Broad Ligament: A Case Report
Amairany Salas Mercado, Ecuvillens / Fribourg
AbstractBackgroundInternal hernias through the broad ligament of the uterus are rare, accounting for approximately 0.2%-0.35% of all hernias. Often underestimated, they predominantly affect multiparous women. A review of the literature revealed a scarcity of articles on the subject, consisting mainly of case reports describing late diagnosis, frequently leading to intestinal resections, with limited data on morbidity and mortality. This case report aims to raise awareness and emphasize the importance of prompt and accurate diagnosis to prevent life-threatening outcomes. Case_presentationA 68-year-old female with a history of open appendectomy and vaginal delivery presented to the emergency department with sudden onset abdominal pain, vomiting, and liquid stools. On examination, she exhibited abdominal tenderness without rebound or guarding and was discharged with a diagnosis of gastroenteritis. She returned 24 hours later with persistent pain and acute abdominal signs. Laboratory tests revealed significant inflammation. Abdominal CT imaging showed a mechanical small bowel obstruction caused by an incarcerated ileal loop in the pelvis, with signs of intestinal ischemia. The patient underwent laparoscopic exploration. A 30 cm necrotic segment of the small intestine incarcerated through an orifice in the left broad ligament, specifically the mesovarium was found. The procedure was converted to an infra-umbilical laparotomy. The affected bowel was resected, followed by side-to-side anastomosis and closure of the defect to prevent recurrence. The patient recovered uneventfully and was discharged on postoperative day four. ConclusionInternal hernias through the broad ligament are often strangulated and require emergency surgery, as they can rapidly progress to bowel ischemia. A high index of suspicion is crucial in female patients presenting with acute small bowel obstruction and a scannographic transition point in the pelvis. 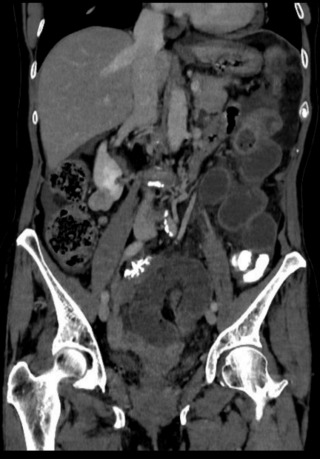
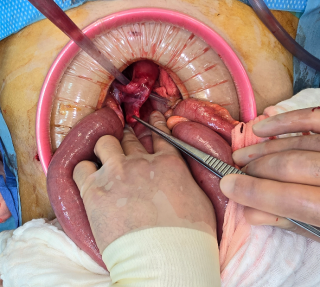

|
||
|
PSGVC78
A Strangulated Meckel's Diverticulum in a Femoral Hernia (Littré's Hernia)
Michael Benoit, Thun
AbstractBackgroundA femoral hernia usually presents as a bulge on the medial side of the thigh, 2-3cm below the inguinal ligament. Among abdominal wall hernias, femoral hernias are the second most common groin hernias. They are characterised by a high level of incarceration or strangulation. Meckel's Diverticulum (MD) is a remnant of the omphalomesenteric duct and it occurs in about 2% of the general population. In rare cases, MD can become incarcerated or strangulated within an abdominal wall hernia, known as Littré's hernia. With an incidence of <0.1% of all complicated hernias, only about 100 cases have been published over the last 300 years. To our knowledge, no cases have been reported in Switzerland. Case_presentationWe present the case of a 75 year old women with a 2-day history of groin pain. On examination an irreducible mass with local skin inflammation was noted. No signs of intestinal obstruction were present. She had an elevated CRP at 95.6 mg/l without leucocytosis. On ultrasound imaging the suspicion of a groin abscess was raised. Intraoperatively the mass revealed to be an incarcerated femoral hernia. We performed a diagnostic laparoscopy where a small bowel loop was adherent to the inguinal region (Fig. 1). After gentle traction a MD could be extracted from a 1-cm femoral ring (Fig. 2). After a TAPP-Repair was performed, the MD was resected with a stapler (Fig. 3). ConclusionA mass in the groin with no signs of intestinal obstruction should raise suspicions preoperatively for the presence of a Littré’s hernia. In such patients conducting a CT scan may have a key role in reaching this difficult diagnosis before surgery. The repair of Littré’s hernia includes both Meckel's Diverticulum resection and hernia repair. This can be achieved successfully laparoscopically. 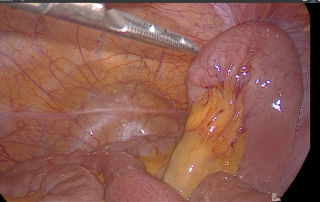
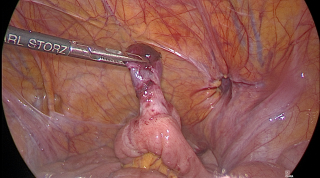
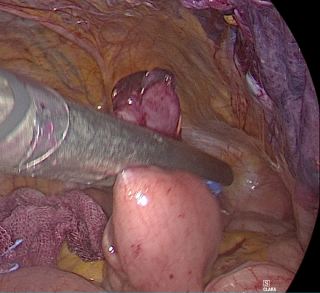
|
||
|
PSGVC79
Never Give Up on Your Patient: A Case of Complex Midline Incisional Hernia
Aline Misar, Zürich / Fribourg
AbstractBackgroundBotulinum toxin A (BTA) injection is a minimally invasive technique that increases the chances of fascial closure in large midline incisional hernias (MIH). Despite several studies proving its efficacy the indication remains off-label. AimsTo present a case with a long history of burst abdomen and MIH. MethodsA 72-year-old male patient underwent open distal esophagectomy for adenocarcinoma at the esogastric junction. During the first 16 days post-operatively the patient presented four episodes of a burst abdomen. No signs of infection were present and during the re-interventions, a Vicryl mesh was placed intra-abdominally. The patient then underwent negative pressure wound therapy. Fascial closure was achieved on post-operative day (POD) 37 and complete skin closure on day 44. The patient has been presenting with a large MIH since (Figure 1+2). Repair had to be delayed because of wound healing issues and malnutrition. ResultsPresenting with a diastasis measured at 18cm on the CT scan (Figure 3) the patient was injected with 200 units of BTA in the lateral abdominal muscles. Three weeks later the patient underwent open Rives-Stoppa repair. BTA administration can reduce the need for component separation but was still necessary in our case helping gain 3cm on each side with the Ramirez technique (Figure 4). The posterior wall was reconstructed using the hernia sac (Figure 5). Anteriorly the fascia could not be completely closed, leaving a mild diastasis of 3cm. He reported significant improvement in quality of life. ConclusionComplex MIH are a challenge for patients and surgeons alike. The use of BTA prior to abdominal wall reconstruction helps achieve better outcomes. This calls for an implementation of standardized technique and patient selection protocols. Lastly, even without achieving complete fascial closure, the patient’s situation was considerably improved. 
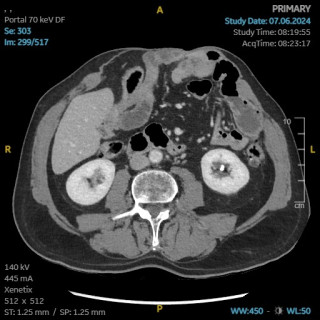
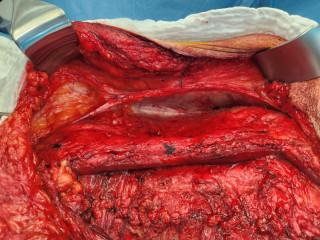
|
||
|
PSGVC80
Acute Appendicitis in an Obturator Hernia: A Case Report of a Two-Staged Surgical Treatment With a Literature Review
Maëlle Thiry, Villars-sur-Glâne / 1708 Fribourg
AbstractBackgroundObturator hernia is a rare condition, accounting for 0.07–1% of all abdominal hernias. Acute appendicitis within an obturator hernia is extremely rare, with only seven reported cases on PubMed. Diagnosis is challenging, as abdominal complaints are not always present, increasing the risk of missed diagnosis. Ultrasound is often insufficient, requiring CT scans for confirmation. AimsReport a case of acute appendicitis within an obturator hernia with two-staged minimally invasive surgical treatment of both pathologies. Additionally, we provide a literature review of this rare entity. MethodsA 21-year-old healthy man presented with a two-day history of lower abdominal pain radiating to the right iliac fossa and right testicle accompanied by a fever. While appendicitis was suspected, ultrasound findings were inconclusive, and a CT scan confirmed the diagnosis. ResultsDiagnostic laparoscopy revealed a perforated appendix with a distal fecalith which was located within a right obturator hernia. With appendectomy and 48 hours of antibiotic treatment the patients had an uneventful recovery. Six months later an elective prophylactic robotic transabdominal preperitoneal obturator hernia repair (rTAPP) was scheduled. Case reports published between 1969 and 2023 reported young male and female as well as old female patients suffering from this pathology. In 43% no abdominal complaints were present. A laparoscopic appendectomy was performed as primary surgical intervention in 57% of patients, with 14% requiring conversion to laparotomy. The hernia was repaired in 29% during the first operation. ConclusionWith less than ten case reports on PubMed acute appendicitis within an obturator hernia remains a rare entity. It can present in young and old individuals and is challenging as abdominal complaints are not always present. 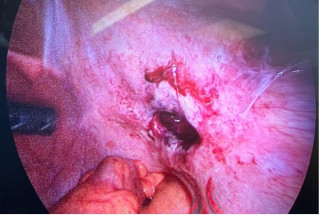
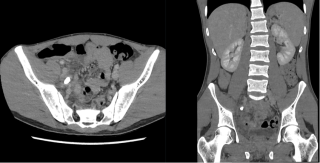
|
||
|
PSGVC81
Traumatic Left Diaphragmatic Hernia of Stomach, Spleen and Left Colon. Laparoscopic Repair and Mesh Placement, 4 Years Ater the Initial Damage Control Open Surgery : A Case Report.
Maëlle Thiry, Villars-sur-Glâne / 1708 Fribourg
AbstractBackgroundTraumatic diaphragmatic hernia (TDH) occurs in 1% to 7% of blunt trauma and is mostly diagnosed by chest X-ray or CT. Treatment prioritizes airway and breathing stabilization, with damage control open surgery for unstable patients. For stable patients, laparoscopic surgical repair is considered the gold standard, offering benefits such as reduced pain, fewer wound complications, and faster recovery. The American Association for the Surgery of Trauma (AAST) recommends mesh reinforcement on the peritoneal surface for grade IV injuries (>10 cm, tissue loss ≤25 cm²). Without mesh, the recurrence rate is significantly high (42%), as demonstrated by our case report. AimsThis case report highlights the recurrence of a diaphragmatic hernia (DH) following primary direct suture of a grade IV diaphragmatic injury without mesh reinforcement. As a secondary aim, we illustrate the feasibility of laparoscopic surgery performed four years after the initial damage control open surgery. MethodsA 54-year-old male with polytrauma, including a left diaphragmatic rupture, underwent primary direct suture of the hernia. Four years later, he complained of a recurrent left grade IV diaphragmatic hernia (10.5x5cm). The patient was referred to our surgical consultation, and we scheduled laparoscopic surgical repair of the hernia. ResultsSignificant adhesions were found between the liver, the spleen and the diaphragm. We performed extensive adhesiolysis for 180 minutes, followed by hernia reduction. The defect was closed with a PDS V-Loc 2-0, and a 10x15 cm Parietex composite mesh was placed. The entire surgery was performed laparoscopically. The patient was hospitalized for 4 days. ConclusionThe recurrence of grade IV diaphragmatic hernia after direct suture is high and often leads to significant adhesions. Laparoscopic adhesiolysis and hernia repair are feasible following primary open surgery. To prevent recurrence, mesh reinforcement should be used even in primary repair of grade IV injuries. 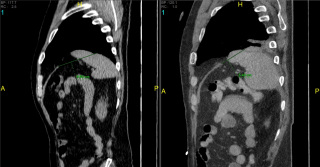
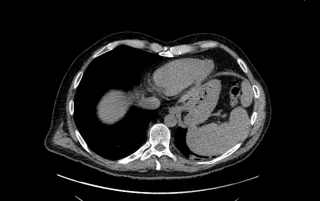

|
||
|
PSGVC82
Umbilical Pilonidal Sinus: A Rare Case, its Diagnosis and Management
Mihail-Ioan Popa, Lachen / Zürich
AbstractBackgroundA rare and frequently overlooked disease, umbilical pilonidal sinus (UPS) typically affects young adults and is more common in men. Seldom seen in the umbilicus or interdigital spaces, the pilonidal sinus normally develops in the sacrococcygeal region. AimsIn an effort to raise awareness among medical professionals and share our viewpoint on the proper diagnosis and successful treatment of UPS, this case illustrates the diagnostic difficulties and successful surgical therapy of the condition. MethodsWe describe a 35-year-old woman who has experienced pruritus and occasional serous umbilical discharge for 6–7 months, which are made worse by physical exercise. Clinical examination showed no signs of granulation tissue or periumbilical dermatitis, but rather a deep-seated umbilicus with serous discharge, slight erythema, and sparse hair. There was no indication of a pore with the obvious entrance, exit, or exterior opening of a UPS. While MRI revealed a limited sinus tract compatible with pilonidal sinus illness, sonography ruled out deeper structural connection. Surgical therapy included refashioning the umbilicus and layered closure after the sinus tract was removed through a periumbilical incision. Fibrolipomatous soft tissue was confirmed by histopathological investigation, although no noteworthy pathological abnormalities were seen. ResultsFollow-ups at one and six weeks showed no evidence of infection, wound secretion, or recurrence, indicating a smooth postoperative recovery. The patient reported no problems and full symptom relief. ConclusionA rare illness that is frequently misdiagnosed because it resembles other umbilical pathologies is the umbilical pilonidal sinus (UPS). The best course of treatment for chronic patients is surgical excision with umbilical reconstruction, which ensures symptom relief and good esthetic results, even when conservative treatments may be adequate at first. |
||
|
PSGVC83
Nuck's Canal Cyst: A Rare Case of Inguinal Pain in Women.
Orianne Lobel, Vevey / Rennaz
AbstractBackgroundNuck's canal cysts are rare, benign lesions resulting from the persistence of the processus vaginalis in females. Although more common in children, they can also appear in adult women. Their rarity and limited awareness among healthcare providers often lead to misdiagnosis. These cysts may cause inguinal pain, swelling, and discomfort, making them an important, though uncommon, differential diagnosis for inguinal pain in women. Accurate diagnosis requires careful clinical evaluation supported by imaging studies, with surgical excision being the most effective treatment. AimsTo raise awareness of this rare condition and highlight its diagnostic challenges. MethodsWe present two cases of Nuck's canal cysts, detailing their clinical presentation, diagnosis and surgical treatment. ResultsThe first case involved a 62-year-old woman with a progressively enlarging, occasionally painful right inguinal bulge over several months. Clinical examination revealed a mobile, homogeneous lesion measuring approximately 4 to 5 cm in the distal and medial right inguinal fold, without signs of a true hernia. A CT scan supported the suspicion of a Nuck's canal cyst. The second case concerned a 46-year-old woman experiencing prolonged discomfort and swelling in the right inguinal region. Examination showed a fusiform, tender swelling extending toward the base of the labium majus. Imaging via ultrasonography and MRI revealed a 50 mm cystic lesion consistent with a Nuck's canal hydrocele. In both cases, surgical exploration confirmed the presence of a cystic formation in the canal of Nuck. The cysts were excised without complications, and both patients experienced uncomplicated recoveries with no recurrence. ConclusionDespite their rarity, Nuck's canal cysts should be considered in the differential diagnosis of inguinal pain in women. Imaging is crucial for diagnosis, and surgical excision remains the definitive treatment with excellent outcomes and low recurrence. Recognizing this rare condition can prevent misdiagnosis and ensure proper management. |
||
|
PSGVC84
The Utility of Intraoperative Ultrasound in the Localization of Post-Open Appendectomy Interstitial Incisional Hernia: A Case Report
Eunice Patricia Santos, Manila PH
AbstractBackgroundAppendectomy is one of the most commonly performed surgical procedures, with incisional hernias occurring as a rare complication in 0.12% of cases. Interstitial incisional hernia is a specific type of hernia wherein the hernial sac protrudes through a defect in the transversus abdominis and internal oblique muscles, but not through the intact external oblique aponeurosis, often posing a diagnostic challenge. Case_presentationWe present the case of a 59-year-old woman who came in with a painful bulge in the right hemiabdomen, located above her previous McBurney incision, following an appendectomy eight months earlier. Ultrasound and CT scans (Figure 1) led to a diagnosis of an interstitial hernia. During surgery, the exact location of the defect was difficult to pinpoint, so an intraoperative ultrasound was conducted (Figure 2). The defect was then repaired with mesh through an open surgical approach (Figure 3). ConclusionIncisional hernias following an open appendectomy via the McBurney incision are uncommon. Two types of incisional hernias can occur post-appendectomy. The more common type involves the hernia traversing all layers of the abdominal wall. The less common type, known as the interstitial hernia, occurs when the hernia passes through a defect in the transversus abdominis and internal oblique muscles, while the aponeurosis and muscles of the external oblique remain intact. One anatomical factor contributing to the development of the latter is the obliteration of the transversalis fascia in the area. Interstitial hernias can be easily missed, and ultrasonography of the abdomen or non-contrast CT of the abdomen can help confirm the diagnosis. However, in cases where there is no noticeable bulge or palpable defect in the external oblique aponeurosis, intraoperative ultrasound can help locate the defect and hernial sac, preventing incorrectly placed incisions and ensuring proper repair. 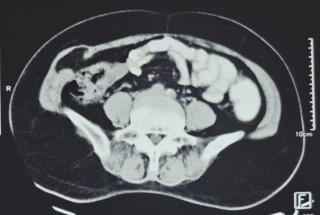
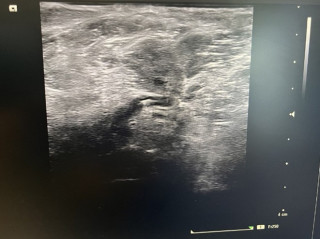
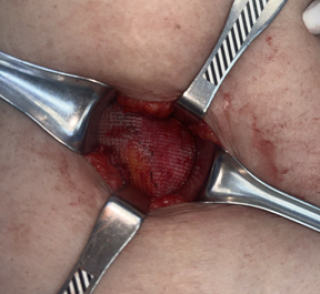
|
||
|
PSGVC85
Retromuscular Prophylactic Mesh Reinforcement After Elective and Emergency Laparotomy: a systematic review and meta-analysis
Melissa Lagger, Fribourg / Villars-sur-Glane
AbstractBackgroundIncisional hernias, occurring in 5–30% of laparotomies, cause substantial morbidity and healthcare costs. Current guidelines recommend prophylactic mesh reinforcement (PMR) in laparotomy closures for high-risk patients; no clear recommendations exist for emergency surgery. Mesh placement in the retromuscular plane is recognized as the most effective technique for preventing hernias and minimizing complications, but the evidence supporting its use, particularly in emergency laparotomies, remains inconsistent. AimsThis systematic review and meta-analysis seeks to assess the effectiveness and safety of retromuscular PMR compared to primary suture closure in reducing incisional hernia rates following laparotomy. Subgroup analyses examine differences between elective and emergency settings. MethodsThis systematic review and meta-analysis was conducted according to the PRISMA guidelines and registered in PROSPERO. Relevant studies were identified through searches in Medline, Embase, and the Cochrane Library (Table 1). Utilizing the PICO framework, studies on elective or emergency laparotomies comparing retromuscular PMR with primary suture closure were included. The primary outcome measured was the incidence of incisional hernias. Data were pooled using the Mantel-Haenszel method (M-H) with a fixed-effects model and presented as odds ratios (ORs) with 95% confidence intervals (CIs). Meta-analysis results at 6, 12, and 24 months were shown in Figures 1-3. ResultsThe analysis included six studies, with only one evaluating patients undergoing emergency laparotomy. Meta-analysis showed significant reductions in incisional hernia rates with retromuscular PMR compared to primary suture closure at 6 months (OR = 0.52, 95% CI: 0.27-1-01), 12 months (OR = 0.62, 95% CI: 0.4-0.95), and 24 months (OR = 0.49, 95% CI: 0.35-0.68). ConclusionRetromuscular PMR significantly reduces incisional hernia rates and improves surgical outcomes following laparotomy, particularly in elective settings. Further research is necessary to clarify its role in emergency laparotomies. 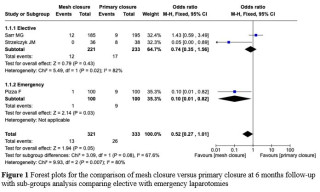
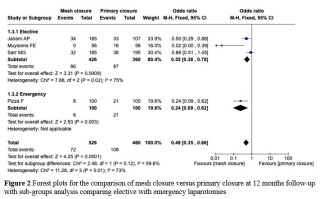
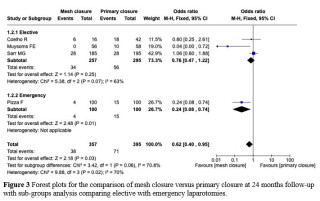
|
||
|
PSGVC86
Coccygeal Hernia: A Rare but Challenging Clinical Condition
Lorenzo Viggiani D'avalos, Bern / Zurich
AbstractBackgroundCoccygeal hernia is a rare condition where tissues or organs, such as fat or intestines, protrude through a defect or weakness in the coccyx. It can result from congenital defects, trauma including the surgical removal of the coccyx, increased abdominal pressure or degenerative changes. Only few cases have been reported, leaving its optimal treatment largely unclear. Case_presentationA 47-year-old woman presented with progressive coccygodynia over the past three years. Pelvic MRI revealed signs of coccygitis. Conservative treatment with pain medications, physiotherapy and cortisone injections was attempted, but only resulted in temporary relief. Therefore, coccygectomy was performed through a longitudinal incision. One year after the procedure she complained of a small lump beneath her scar, increasing pain when sitting including defecation disorders. Clinical examination revealed a tender swelling at incision site. During Vasalva, the pelvic floor bulged through the incision site. A dynamic MRI confirmed pelvic floor descent with subsacral prolapse of the rectum. Surgery was planned. To ensure optimal stabilization, we opted for an open repair technique using a synthetic, non-absorbable mesh (Ultrapro DynaMesh®). Surgery was performed in Heidelberg position through a Kraske approach (Fig.1). The tailored mesh was placed in sublay technique, secured with Ethibond sutures (Fig. 2). The fascia, subcutaneous tissue, and skin were closed separately after placing a wound drain. Post-operative recovery was uneventful. The drain was removed on day 3 post-operatively and the patient was discharged the following day. At six-month follow-up, the defecation disorder fully resolved, although moderate coccygodynia persisted. ConclusionVarious techniques such as primary herniorrhaphy, mesh repair, muscle transposition and repair with de-epithelialized musculocutaneous flaps via sacral, abdominal, or laparoscopic approaches have been described. We opted for an open sacral approach with synthetic mesh to ensure maximum stabilization of the pelvic floor and minimize risk of recurrence. 
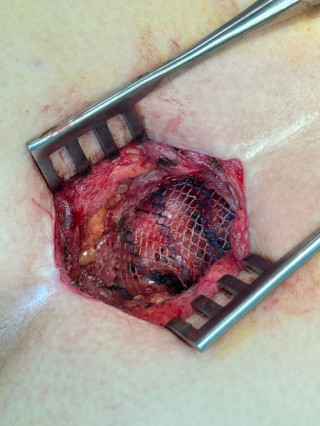
|
||
|
PSGVC87
Loss of domain giant incisional hernia with skin tension lesions: A case report
Philippe Di Cicco, Villars-sur-Glâne / Fribourg
AbstractBackgroundGiant hernias with loss of domain (LOD) are complex pathologies characterized by major intestinal prolapse in the hernia sac, only composed of the peritoneum and the skin. This may lead in the case of a voluminous and heavy hernia to tension lesions of the skin. Skin perforation needs in these cases often challenging operations with high mortality and morbidity. Case_presentationAn 81-year-old female presented with a long-standing incisional hernia complicated by recent bleeding from a 2 cm² lesion at the lowest point of the hernia sac and the presence of a second, non-bleeding ulcer. CT imaging (Figure 1) revealed a large hernia sac containing most of the small intestine in the upright position. The overlying skin shows a skip lesion. The peritoneum cannot be identified, but there are no signs of peritonitis. Conservative management, including specialized care in a wound center and use of an abdominal belt, was initiated to support the skin of the hernia. The patient tolerated the abdominal belt well, which helped reduce the tension on the skin. At 1-month follow-up, the wounds showed granulation tissue, reduced size, and calm edges. The evolution was favorable (Figure 2) with complete closure of the cutaneous wounds at 3-month follow-up. ConclusionThis case highlights the importance of managing cutaneous lesions in LOD hernias, where surgical intervention is not viable. A specially designed abdominal belt reduced skin tension and allowed, together with standard wound care, healing of the wounds. Despite the high-risk location of these declivous lesions, complete wound closure was achieved with specialized wound center care. It demonstrates the potential for conservative management to prevent severe complications in cases of LOD hernia where surgery is too risky. 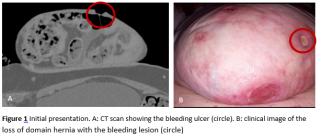
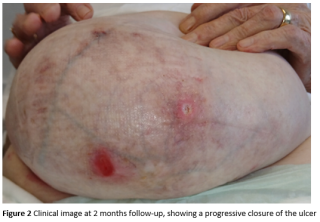
|
||
|
PSGVC89
Buschke-Löwenstein Tumour Surgical Management: A Case Report and Literature Review
Chiara Maria Fragati, Locarno
AbstractBackgroundGiant Condyloma Acuminatum (GCA) represents a rare sexually transmitted disease caused by the human papillomavirus (HPV) subtypes 6 and 11. It is a rare exophytic lesion with a tendency to infiltrate adjacent tissues. It is characterised by a high recurrence rate and associated with the potential for malignant transformation. AimsThe aim of our case report is to highlight the complexity and importance of surgical intervention in the case of Giant Condyloma Acuminatum. MethodsThe case concerns a 61-year-old patient known to have metastatic carcinoma of the larynx. He was known to have a peri-anal lesion for roughly 40 years without ever having consulted a physician. A routine follow up CT scan of the abdomen, showed a thickening at the intergluteal site for which, following a proctological examination, a diagnosis is made of GCA. The anoscopy showed the absence of inter-anal mucosal involvement and therefore surgical resection was indicated. ResultsCytology confirmed the HPV 6 and 11 phenotypes. In the immediate post operative period there was a wound dehiscence that was subsequently treated conservatively through healing by secondary intention. At two-months follow-up, we observed almost complete epithelisation of the surgical wound in the absence of local recurrence. ConclusionThere are several therapies for the management of the disease. The choice of therapy must be individualised based on the extent of the disease, patient preference, cost, adverse effects, treatment availability and response to previous treatments. Complete surgical excision is the treatment of choice for GCA. 


|
||
|
PSGVC90
Retrorectal tumors: single-center experience
Cinzia Tanda, Yverdon-les-Bains
AbstractBackgroundRetrorectal tumors are rare and present significant challenges in terms of diagnosis, surgical treatment, and follow-up, particularly in cases of local recurrence. This study aimed to report a single-center experience in managing retrorectal tumors, with a focus on surgical techniques, outcomes, and follow-up strategies. AimsThe aim of this study was to share a single-center experience in the treatment of retrorectal tumors. MethodsBetween 2018 and 2024, patients diagnosed with retrorectal tumors and treated at eHnv Hospital were retrospectively analyzed. Six patients were included in the review, with a median follow-up period of 18 months. ResultsThe posterior approach, using intersphincteric excisions, was preferred due to its advantages in achieving complete resection, minimizing morbidity, and preserving anal function. The median age was 41 years. All patients underwent clinical examinations, endorectal 3D ultrasonography, and perineal MRI as part of their diagnostic and follow-up protocol. Among the six patients, two presented with symptoms: one reported dyschezia, while the other experienced anal soiling. One patient developed a recurrence three months postoperatively, manifesting as a fistula. After undergoing a second intersphincteric resection, this patient remained disease-free. Another patient reported perineal pain and dyschezia, which resolved completely after 18 sessions of biofeedback physiotherapy. No cases of incontinence were observed during the follow-up period. At a median follow-up of 18 months, five patients were confirmed to be disease-free. ConclusionAlthough retrorectal tumors are rare, their management remains complex. This study highlights potential risk factors for local recurrence, including patient-related factors (e.g., the presence of a perineal mass), tumor characteristics (e.g., size), and surgical factors (e.g., incomplete resection). The posterior approach is recommended for low retrorectal tumors. A follow-up protocol is proposed, including clinical examinations, endorectal 3D ultrasonography, and pelvic MRI performed annually up to 5 years.
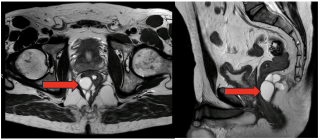
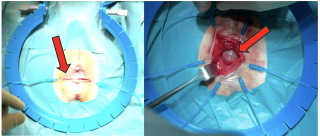
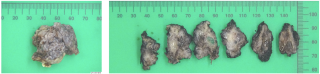
|
||
|
PSGVC91
A Comprehensive Review of Artificial Anal Sphincters for Faecal Incontinence: Comparisons with Urinary Incontinence Devices and Future Directions
Axelle Lavigne, Geneve
AbstractBackgroundFaecal and urinary incontinence are both prevalent conditions worldwide, leading to significant negative impact on quality of life. Artificial sphincters offer a bioengineered solution to replicate the function of biological sphincters. Although designed to imitate the biological function closely, these devices exhibit limitations and are sometimes suboptimal in performance. Advancements in anal sphincter technology remains limited in comparison to urinary sphincters. AimsThis review aims to systematically evaluate the existing research on artificial anal sphincters for faecal incontinence. MethodsA total of 105 relevant studies, including 3 RCTs, 8 clinical trials, 3 meta-analyses and 91 reviews, were retrieved from online databases and analysed. ResultsWe describe an overview of current anal sphincter technology being used for faecal incontinence, describing their mechanisms, functionalities, success rates and complications profile. To contextualise these findings, we compare them with urinary incontinence treated with implantable devices research, such as the artificial urinary sphincter or transobturator tapes, which has seen more extensive development and positive outcomes. Similar keywords retrieve over 300 RCTs, 575 clinical trials, 128 meta analyses and 990 reviews. Finally, we explore future directions for biomedical innovation, including potential applications in stoma care and endoluminal devices. ConclusionThis review underscores the need for continued advancements in anal sphincter technology to improve outcomes for patients with faecal incontinence. |
||
|
PSGVC92
Bubbles in the Bowel: A Pneumatosis Intestinalis Case Report
Kowsar Abdullahi, Biel
AbstractBackgroundPneumatosis intestinalis (PI), a radiological finding of gas within the intestinal wall, is increasingly detected due to Computed tomography scans. It may be a primary idiopathic condition or secondary to benign (e.g., pulmonary diseases, corticosteroid use) or life-threatening causes (e.g., obstruction, ischemia). The challenge lies in identifying cases that require surgical intervention. Case_presentationWe report a case of a 50-year-old male who presented with acute epigastric pain and abdominal distension. Clinical examination revealed a tense abdomen with tenderness in the epigastric region. Laboratory findings showed mildly elevated inflammatory markers. Computed tomography of the abdomen with contrast (Figure 1) showed distended small bowel loops, free fluid interenteric and in the upper abdomen as well as signs of hollow organ perforation with free air predominantly interenteric and in the mesenteric fatty tissue. Given these findings, surgical exploration was performed. A 15 cm midline laparotomy revealed pneumatosis (Figure 2) affecting approximately 80% of the proximal 280 cm of the jejunum, interspersed with normal areas. The remaining bowel appeared healthy. No perforation or peritonitis was identified. The abdomen was irrigated, no resection was done and closure was performed. ConclusionPneumatosis intestinalis may indicate life-threatening conditions like bowel ischemia or benign causes. Signs like portal venous gas and pneumoperitoneum should be interpreted with caution, as they may arise from benign Pneumatosis intestinalis rather than perforation. Management should be guided by the clinical status of the patient and laboratory findings. Conservative treatment is appropriate for benign cases, while surgical intervention is reserved for suspected perforation or ischemia. 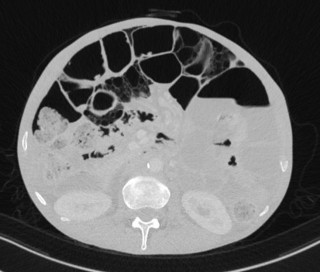

|
||
|
PSGVC93
Patient clusters and compliance to enhanced recovery items – time for a tailored perioperative care protocol?
Philip Deslarzes, Lausanne
AbstractBackgroundPerioperative enhanced recovery care (ERAS) protocols for a given procedure apply to all patients, regardless of comorbidities, surgical difficulty, or functional recovery. Therefore, there is a need to refine protocols towards a more personalized, tailored approach. The aim of the present study was to use machine learning techniques to define patient clusters and tailor intra- and perioperative care protocols to anticipate challenges and improve postoperative recovery and outcomes. AimsThe aim of the present study was to use machine learning techniques to define patient clusters and tailor intra- and perioperative care protocols to anticipate challenges and improve postoperative recovery and outcomes. MethodsThis is a monocentric retrospective cohort study including consecutive patients who underwent elective colorectal surgery in the visceral surgery department at CHUV between 1st May 2011 and 31st December 2021. Preoperative data, surgical details, and ERAS compliance were collected. Unsupervised machine learning techniques, specifically K-Means clustering, were used to identify patient subgroups. These clusters were then analyzed to predict and anticipate patient trajectories. ResultsIn total, 1381 patients were available for final analysis. For demographic variables, 3 clusters were identified. After analysis of the demographic and the perioperative variables, two different clusters corresponded to high and low compliance. Finally, outcome variables were grouped in 3 distinct clusters, while 2 clusters appeared for the top functional and clinical outcomes. 99.6% of the low-risk demographic cluster had high perioperative compliance, and over 90% of them had favorable functional and clinical outcomes. Only 370/1381 patients (27%) were in the cluster high perioperative compliance. 100% of the high-risk demographic group had low perioperative compliance: Furthermore, patients with low perioperative compliance had adverse functional outcomes in over 40%.
ConclusionPreoperative knowledge of patient clusters helps to trigger efforts to optimize modifiable demographic risk factors prior to surgery and to intensify efforts to increase perioperative compliance in the sense of a tailored pathway. |
||
|
PSGVC94
Ileocecal Intussusception as a Rare Presentation of Appendiceal Mucinous Neoplasm: A Case Report
Oscar Feusi, Uster
AbstractBackgroundIleocecal intussusception in adults is rare. Most cases are associated with a mass, which is often malignant. This case highlights the diagnostic and surgical management of a patient presenting with ileocecal intussusception secondary to a metastatic low-grade appendiceal mucinous neoplasm (LAMN). Case_presentationA 55-year-old male presented to the emergency department with acute abdominal pain. A computed tomography (CT) scan was conducted, which revealed an intussusception involving the ileocecal segment of the bowel and decision for surgery was made. Intraoperatively disseminated mucinous nodules were detected, suggestive for peritoneal carcinomatosis. Laparoscopic right hemicolectomy was performed. Histopathology confirmed the presence of a low-grade appendiceal mucinous neoplasm (LAMN) with peritoneal metastasis, consistent with pseudomyxoma peritonei. After an uneventful recovery, the patient was subsequently referred to cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC), as decided during multi-disciplinary team meeting (MDT). ConclusionThis case underscores the importance of maintaining a high index of suspicion for malignant processes in a case with intestinal intussusception in adults. It also highlights the critical role of histopathological analysis in identifying underlying malignancies and guiding postoperative management. Early recognition and a multidisciplinary approach are essential for a preferable outcome in similar presentations. |
||
|
PSGVC95
Perineal Defect Reconstruction: An Overview of Standard Approaches and Emerging Techniques
Joëlle V. Hüppi, Winterthur
AbstractBackgroundNumerous surgical techniques have been described for the reconstruction of perineal defects. The selection of the reconstructive procedure is largely determined by the characteristics of the defect, including its size, shape, and the involvement of underlying anatomical structures. In addition to well-established methods, emerging techniques have shown promise, offering advantages in certain clinical scenarios. AimsThis illustrative presentation aims to provide an overview of the most commonly employed methods for perineal defect reconstruction. Additionally, we will present novel or less frequently utilized approaches based on our clinical experience. MethodsA review of the literature is conducted to identify prevalent surgical techniques for perineal defect repair. Clinical cases involving perineal defects are collected, and corresponding operative approaches evaluated. Furthermore, unconventional and patient-tailored techniques for perineal defect reconstruction from our own experience are described. ResultsIn our experience, successful healing and favorable functional outcome can be achieved with both conventional and new approaches, provided the prerequisites for undisturbed healing are respected. These include well perfused, non-infected tissue, tension-free closures and clean wound conditions. Given the proximity to the anus and the increased risk of infection, the option of stoma creation should be discussed preoperatively for larger defects to minimize complications. ConclusionPerineal defect reconstruction is a significant challenge for plastic and reconstructive surgeons. Due to the complex underlying anatomy and the proximity to the anus, the complication rate remains high regardless of the surgical approach. New techniques are continually introduced with the aim of improving both functional and aesthetic outcomes. Their long-term reliability and potential superiority must be assessed over time in various scenarios and further evaluated based on surgeons' experience. |
||
|
PSGVC96
LASER HEMORRHOIDOPLASTY (LHP) FOR THE TREATMENT OF HEMORROIDAL DISEASE. ALWAYS MUCOPEXY ? CONSIDERATIONS, TIPS AND TRICKS AFTER MORE THAN 1000 CASES PERFORMED BY A SINGLE SURGEON
IONEL HORIA Roman, La Conversion
AbstractBackgroundLaser hemorrhoidal procedure (LHP) is still considered a new minimally invasive technique to treat symptomatic hemorrhoids.It is not uniformely standardized, therefore after 1000+ cases we drew some conclusions and formulated some recommendations. AimsTo find the right technical solutions in the treatment of hemorrhoidal disease by LASER, using the LHP technique, after performing more than 1000 interventions of this type, by a single surgeon, with or without associating a short - mucopexy To establish what grade of hemorrhoids are suitable for the best results, and wether the mucopexy is getting an advantage or not. MethodsIndications for LHP included patients with symptomatic hemorrhoids resistant to medical therapy, with low- medium-high grade of prolapse. Clinical efficiency was evaluated assessing resolution of symptoms and patient satisfaction. We compared the acceptability, postoperative evolution and levels of pain, hospitalization, and overall short time results after more than seven years of experience with LHP. As not enough standard recommendations, we tried to compare several technical approaches and we formulated some tips and tricks. ResultsExcellent re-integration of the patients after only several days, ZERO PAIN for more than 30 % of the patients postoperatively, and 2-5 days of moderate pain for the majority. The good short term results, confirmed also by other studies already published, suggest that LHP is an interesting option in the treatment of hemorrhoidal disease, especially if associated to mucopexy, largely preferred by the author. ConclusionThe LHP procedure seems to be safe and effective in patients with symptomatic hemorrhoids, even high graded, especially when short mucopexy is associated.. It is simple, minimally invasive, and relatively pain free. It can be performed in an ambulatory setting, and it achieves high patient satisfaction. |
||
|
PSGVC97
MASSIVE OGILVIE SYNDROME WITH CRI-DRU-CHAT SYNDROME: A RARE CASE OF GASTROINTESTINAL DYSREGULATION IN OLDER PATIENT
Senta Faulhaber, Schlieren
AbstractBackgroundOgilvie syndrome, a rare condition of acute colonic pseudo-obstruction, poses significant risks of ischemia and perforation without mechanical blockage. Cri-du-Chat syndrome, caused by a deletion on chromosome 5p, is associated with intellectual disability and developmental delays but rarely with gastrointestinal issues. This report examines an unusual case of massive Ogilvie syndrome in a patient with Cri-du-Chat syndrome, suggesting potential neurological and physiological links. Case_presentationA 62-year-old female with Cri-du-Chat syndrome presented to the emergency department with severe abdominal distension and pain lasting two days. The caregiver reported no bowel movements in the previous 24 hours. Apart from a known allergy to doxycycline, no other medical history was available. Examination revealed a grotesquely distended, tympanic, and tender abdomen. Laboratory tests showed no infection or metabolic disturbances. CT imaging revealed significant sigmoid colon dilatation (23 cm), indicating Ogilvie syndrome with a risk of ischemia or perforation. Initial treatment included digital rectal evacuation and endoscopic decompression under anesthesia, which showed good bowel perfusion. Due to persistent severe distension and high risk of perforation, surgical intervention was required. A laparotomy with double-barrel transverse colostomy successfully decompressed the colon and ensured bowel viability. Outcome: Postoperative recovery was uneventful, except for a transient right-sided pneumonia. The patient resumed dietary intake without complications, and the stoma exhibited good output.
ConclusionThis case emphasizes the need for prompt diagnosis and intervention in intellectually disabled patients to prevent life-threatening complications. The potential association between Cri-du-Chat syndrome and Ogilvie syndrome underscores the importance of individualized, multidisciplinary care for this unique patient population. 
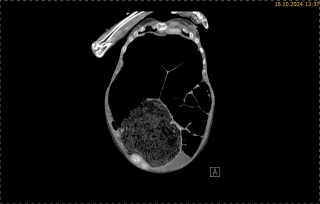
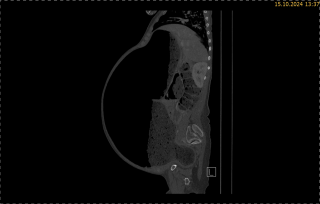
|
||
|
PSGVC99
Acute Perforated Appendiceal Diverticulitis: A Case Report and Overview of the Literature
Elisabeth Brändle, Winterthur
AbstractBackgroundDiverticulum and diverticulitis of the appendix are rare and usually diagnosed retrospectively by the pathologist in patients with suspected acute appendicitis undergoing appendectomy. Case_presentationA 55-year-old patient presented to the emergency department with a 4-day history of abdominal pain, typical symptoms of appendicitis and elevated inflammatory markers. Computed tomography revealed signs of acute appendicitis. The patient underwent laparoscopic appendectomy and the histopathological examination revealed a perforated acute appendiceal diverticulitis. ConclusionAppendiceal diverticulitis is a rare finding in clinical practice. It is important to be aware of this entity since appendiceal diverticulitis is associated with a higher rate of complications as perforation and an increased risk of appendiceal neoplasm. We report a rare case of perforated appendiceal diverticulitis and a brief discussion about the histopathological features, clinical behavior, treatment and overview of the literature are presented. |
||
|
PSGVC100
Crucial Multidisciplinary Management of Hemorrhagic Shock Due to Arteriodigestive Fistula
Hassan Youssef, Genève / Geneva
AbstractBackgroundArteriodigestive fistulas represent an uncommon but life-threatening complication of cancer treatment, often resulting from radiation-induced tissue damage, chronic inflammation, or iatrogenic trauma. Such conditions require timely recognition and a comprehensive, multidisciplinary approach for optimal management. This report describes a case of hemorrhagic shock due to an iliac-sigmoid fistula in a patient with a complex oncological and comorbid profile, highlighting the diagnostic challenges and therapeutic strategies involved in prompt recognition and management to prevent fatal outcomes.
Case_presentationWe herein report the case of a 77-year-old female with a history of FIGO stage IIIC2 serous endometrial adenocarcinoma treated with neoadjuvant chemotherapy, hysterectomy, and adjuvant radiotherapy, who presented with acute hematochezia and hemodynamic instability. Laboratory investigations revealed severe anemia (hemoglobin 70 g/L), while CT imaging identified a pseudoaneurysm of the left external iliac artery adjacent to the sigmoid colon, with findings consistent with an arteriodigestive fistula and associated retroperitoneal collection.
Management involved an initial endovascular stenting of the left external iliac artery to control active bleeding, followed by a Hartmann’s sigmoidectomy to address the fistula. Postoperative care included CT-guided drainage of the retroperitoneal abscess, microbiologically confirmed to contain multidrug-resistant Proteus vulgaris and Streptococcus anginosus. Antibiotic therapy was initiated with meropenem, followed by a six-week course of oral co-amoxicillin. Nutritional optimization was achieved with parenteral nutrition and progressively transitioned to oral intake supplemented by high-protein nutritional formulas. Follow-up imaging showed resolution of the collection and absence of active bleeding, enabling discharge with outpatient multidisciplinary follow-up.
ConclusionThis case underscores the importance of a multidisciplinary approach to managing complex post-radiotherapy complications such as arteriodigestive fistulas. Early diagnosis, timely surgical and radiological interventions, and tailored infection control were essential in achieving a favorable outcome. This case highlights the critical need for coordinated multidisciplinary care in patients with cancer-related complications to optimize recovery and prevent mortality. 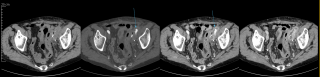
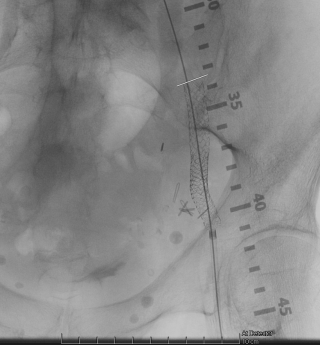
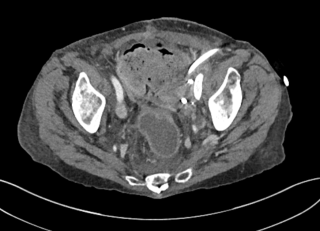
|
||
|
PSGVC101
Internal Pudendal Artery Injury Following Pudendal Block: A Case Report
Elena Patanè, Geneva / Genève
AbstractBackgroundLiterature shows significant advantages of pudendal nerve block (PNB) in reducing pain in coloproctology. Complications related to PNB include intravenous injection of the anesthetic, urinary retention, hematoma, and abscess formation. The pudendal nerve arises from the spinal rami S2-S4, exits the pelvis, and reenters the perineum to course through the ischiorectal fossa and Alcock’s canal. Here, the internal pudendal artery and vein course near the pudendal nerve. In case a vascular injury is suspected, a computed tomography (CT) scan should be performed, and if active bleeding is found, an interventional radiology procedure is necessary.
Case_presentationWe report a case of internal pudendal artery injury following a pudendal block for posterior colporrhaphy in a 57-year-old woman with Hemophilia C. We performed a pudendal nerve block with an injection of 20 milliliters of ropivacaine 5 mg/ml after negative aspiration. On the second postoperative day, the patient reported sudden pain in the left buttock, associated with a painful hardening of the area (figure1). An abdomen-to-pelvis CT scan revealed a massive hematoma in the Alcock canal with contrast extravasation from the left internal pudendal artery(figure2).Angiography with transcatheter arterial embolization was performed(figure3). No blood transfusion or surgical evacuation was needed. The patient received three units of fresh frozen plasma and tranexamic acid 1.5 g intravenously every 8 hours for ten days, as per hematologists' recommendations. The patient was discharged eleven days after surgery, and the hematoma was followed up at an outpatient clinic with spontaneous resolution.
ConclusionPudendal artery injury is a rare but possible complication due to the close anatomical proximity of the artery and nerve. This must be considered in cases of perineal or gluteal hematoma after PNB. Quick diagnosis with CT scan is essential, and in some cases, embolization is necessary.


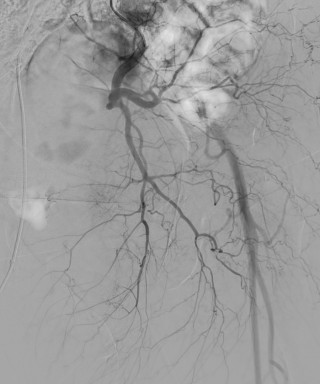
|
||
|
PSGVC102
Terminal Ileitis With Perforation Due to Enterotoxigenic Escherichia coli: Diagnostic Challenges and Surgical Management
Michal Misurda, Winterthur / Schaffhausen
AbstractBackgroundTerminal ileitis can pose significant diagnostic challenges due to its association with various etiologies, including Crohn's disease, infectious diseases, ischemia, and NSAID-induced conditions. Accurate identification of the underlying cause is essential for appropriate management. Case_presentationA 32-year-old female with no previous symptoms or history of inflammatory bowel disease presented with acute lower abdominal pain and signs of systemic infection. A detailed travel anamnesis revealed several months spent in Africa. Emergency sonography and CT imaging demonstrated significant thickening of the terminal ileum and ascites (Fig. 1), indicative of potential bowel perforation, thereby necessitating immediate surgical intervention over diagnostic colonoscopy. During surgery, four-quadrant peritonitis and two ileal perforations approximately 10-15 cm proximal to the ileocecal valve were discovered. These findings led to an ileocecal resection with end-to-end ileoascendostomy. Histopathological analysis revealed deep ulcerations and transmural inflammation, without granulomas, consistent with an acute infectious process. Laboratory tests confirmed the presence of Enterotoxigenic Escherichia coli (ETEC), establishing it as the causative agent for the perforations. The patient’s recovery was complicated by ileus and aspiration pneumonia, yet effectively managed with antibiotics and supportive care. Subsequent colonoscopy and follow-up evaluations confirmed the absence of chronic IBD. ConclusionThis case highlights the diagnostic complexities in acute gastrointestinal presentations, particularly in differentiating between chronic inflammatory diseases and acute infectious causes. The presence of ETEC, identified through stool culture, underlines the importance of considering travel history and less common pathogens in the differential diagnosis. Comprehensive intraoperative assessments and detailed histological studies are pivotal in guiding effective treatment strategies, emphasizing the necessity for a broad differential diagnosis in acute cases of terminal ileitis. 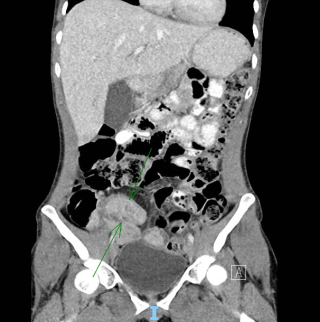
|
||
|
PSGVC103
Beyond the Scope: A Rare Case of Retroperitoneal Perforation Following Colonoscopy
Stefano Gussago, Nyon
AbstractBackgroundIatrogenic colonic perforation occurs in up to 0.03 to 0.8% of colonoscopy procedures, with a mortality rate as high as 25%. The incidence is increased in therapeutic colonoscopies compared to diagnostic ones. The cecum is the second most common site of perforation. Pneumoperitoneum often signals perforation and requires urgent surgical intervention in case of peritonitis. Pneumoscrotum is a rare complication, and suggest retroperitoneal perforation. Pneumoscrotum generally has a benign outcome and is managed with observation and antibiotics. This case highlights the importance of prompt recognition and vigilant post-procedural monitoring. Case_presentationAims : A 77 y/o male patient underwent a screening colonoscopy, during which multiples cold snare polypectomies were performed. Notably, the resection of one 5 mm polyp (Paris 0-IIa / NICE I) of the ascending colon was complicated by a submucosal breach, without any hemorrhagic complications or post-procedural subcutaneous emphysema. The patient presented an isolated episode of fever of 38.5°C, without any others complains. Two day later, after discharge, he complained of a swelling of the genitals. Physical examination showed subcutaneous emphysema at the prepubic, scrotal, and penile levels.
Methods : Blood samples revealed mild leucocytosis (8.1 G/l) and an elevated C-reactive protein (97.6 mg/l). A subsequent abdominal CT scan showed a large retroperitoneum, extending from the mediastinum to the genital area, with an important pneumoscrotum and pneumopenis. Medical treatment was decided with IV antibiotic therapy (Piperacillin/Tazobactam 4.5 g three times daily).
Results : The patient was discharged on day 4. Antibiotic therapy was switched to Ciprofloxacin 500 mg twice daily and Metronidazole 500 mg three times daily during 7 days. Outpatient follow-up was uneventful. ConclusionAlthough rare, retroperitoneal perforation during operative colonoscopy may presents as a pneumoscrotum and pneumopenis. In stable patients, conservative treatment may be an appropriate strategy.
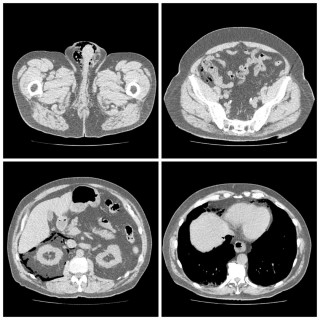
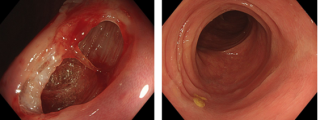
|
||
|
PSGVC104
A Rare Presentation of Giant Cell Arteritis: Small Bowel Stenosis Leading to Intestinal Obstruction
Ana Cristina Da Silva Costa, Vevey
AbstractBackgroundGiant cell arteritis (GCA) primarily affects medium- and large-sized arteries, most commonly the temporal arteries, but also the carotid arteries, vertebral arteries, and the aorta. However, involvement of the gastrointestinal vasculature is rare, making diagnosis particularly challenging. Case_presentationWe present the case of a 76-year-old woman with a history of atrial fibrillation, COPD, and Takotsubo syndrome who was hospitalized several months prior, with symptoms raising suspicion for GCA, however, diagnostic evaluations at that time were inconclusive. On this admission, she presented with worsening chronic abdominal pain over two weeks, associated with vomiting, and significant unintentional weight loss. She was hemodynamically stable and afebrile. Physical examination revealed epigastric tenderness without guarding. Laboratory findings showed mild leukocytosis and elevated C-reactive protein. Abdominal CT imaging indicated mechanical small bowel ileus without worrisome features. Gradual refeeding was initiated to optimize her nutritional status before surgery. On day 12, she underwent surgical exploration during which three areas of macroscopic stenosis were identified, leading to segmental resection of the distal jejunum and proximal ileum followed by anastomosis. Histopathological analysis identified few giant cells within a mesenteric artery wall, supporting a potential diagnosis of vasculitis. Postoperative recovery was successful with improvement of abdominal pain and early refeeding, and the patient was discharged on day 20. Two months later, a PET-CT showed multifocal large-vessel vasculitis suggestive of GCA, associated with polymyalgia rheumatica. Corticosteroid therapy was promptly initiated. ConclusionExtra-temporal manifestations of GCA, such as gastrointestinal vessel involvement, are rare and challenging to diagnose. Awareness of these atypical presentations is crucial for early systemic treatment and improved patient outcomes.
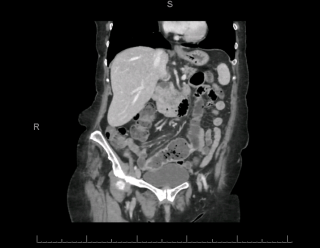
|
||
|
PSGVC105
Seeing beyond the biopsy: diagnostic challenges in a colonic MALT lymphoma
Christian Herber, Uznach
AbstractBackgroundNon-Hodgkin lymphoma (NHL) exhibits extranodal involvement in about one-third of cases, with the gastrointestinal (GI) tract being a common site 1–5. While mucosa-associated lymphoid tissue (MALT) lymphoma most frequently arises in the stomach 6–11, colonic MALT lymphoma accounts for only about 2.5% of all MALT lymphomas 8,12,13. The pathogenesis in the colon is not well-defined, and no clear infectious trigger, similar to Helicobacter pylori in gastric MALT lymphoma, has been identified 1,7. Case_presentationWe present the case of a 66-year-old female patient with a cecal mass detected during routine screening colonoscopy. Despite inconclusive biopsies, imaging findings raised suspicion of malignancy, prompting surgical resection. Histopathology revealed a colonic MALT lymphoma measuring up to 4 cm, with transmural infiltration and extension into the base of the appendix. Regional lymph nodes were tumor-free. Postoperatively, the patient recovered uneventfully. ConclusionThis case underscores the rarity of colonic MALT lymphoma and highlights the importance of thorough endoscopic evaluation, imaging-based staging, and surgical resection in achieving favorable outcomes for patients with colonic MALT lymphoma. While guidelines for managing colonic MALT lymphoma remain less clearly defined than those for gastric MALT lymphoma, prompt detection and resection in localized disease appear critical to successful treatment 14–19. Further research is needed to elucidate possible etiologic factors and to optimize treatment strategies for this uncommon presentation. |
||
|
PSGVC106
Low-Grade Fibromyxoid Sarcoma of the Ileocecal Region: A Rare and Challenging Diagnosis
Amandine Chavanon, Biel/Bienne / Biel
AbstractBackgroundLow-grade fibromyxoid sarcoma (LGFMS) is a rare, indolent soft tissue tumor with a significant risk of distant metastasis, despite its low-grade nature. The nonspecific clinical presentation and inconclusive biopsy results often delay diagnosis and management, emphasizing the need for awareness of this entity. Case_presentationA 78-year-old male presented with persistent left-sided pain localized to the Th11 region. Notably, the patient denied systemic symptoms such as weight loss, abdominal pain, or bowel habit changes. Imaging studies, including a CT scan, identified a progressively enlarging mass adjacent to the cecum and terminal ileum, raising suspicion of malignancy (Figures 1 and 29. Colonoscopy with multiple biopsies failed to yield a definitive diagnosis. A diagnostic laparoscopy was subsequently performed, during which the mass was successfully resected. Histopathological evaluation confirmed LGFMS, characterized by alternating fibrous and myxoid stroma, low mitotic activity and absence of significant necrosis. Immunohistochemical analysis showed diffuse positivity for MUC4, a hallmark feature of LGFMS, solidifying the diagnosis.
ConclusionThis case underscores the importance of considering rare soft tissue sarcomas like LGFMS in the differential diagnosis of abdominal masses, especially when initial biopsies are inconclusive. Early identification, complete surgical resection, and meticulous histopathological evaluation, including immunohistochemistry are pivotal in achieving optimal outcomes. Long-term follow-up remains critical to monitor for recurrence or distant metastasis.

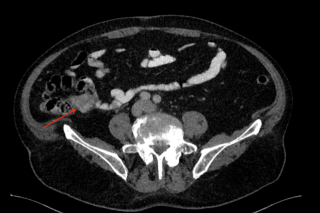
|
||
|
PSGVC107
The Impact of Spinal Anesthesia in Laparoscopic Colorectal Surgery on Bowel Function and Pain Relief - a Systematic Review and Meta-Analysis of Randomized Controlled Studies
Eleonora Bianchi, Baden
AbstractBackgroundRecently, the Enhanced Recovery After Surgery (ERAS) society recommended spinal anesthesia as a valuable adjunct to colorectal surgery with its primary advantages being enhanced pain control and reduced opioid use. Given that opioids can adversely affect bowel function, we hypothesized that spinal anesthesia may be associated with a reduction in postoperative ileus. AimsThis systematic review aims to examine the existing literature on the effect of spinal anesthesia on postoperative bowel function following colorectal surgery. MethodsRelevant articles were identified by searching central libraries from the time of inception to October 2023. Inclusion criteria were studies comparing outcomes of colorectal surgery with and without spinal anesthesia. Primary outcomes of interest were bowel function, pain management 24 hours after surgery. The quality of the included articles was assessed using the Cochrane risk-of-bias tool for randomized trials (RoB 2). ResultsFive randomized controlled trials were identified from a total of 790 published articles, encompassing 338 patients who underwent laparoscopic colorectal surgery under general anesthesia, with or without spinal anesthesia. Spinal anesthesia was administered to 168 patients. No significant demographic differences were noted between the control and intervention groups. Spinal anesthesia was associated with improved postoperative pain control and a significant reduction in opioid consumption (MD: -0.749; CI -1.219 to -0.279, p-value: 0.002 and MD: -1.994; CI -2.315 to -1.673, p-value: <0.001, respectively). However, no significant difference were observed between the groups in terms of postoperative bowel function: time to flatus MD: -0. 054; 95% CI -0.268 to 0.160; p-value: 0.62; time to stool MD: -0.254; CI -0.526 to 0.018, p-value: 0.07; or time to resumption of a normal diet MD: -0.230; CI -0.490 to 0.031, p-value: 0.08. ConclusionSpinal anesthesia in laparoscopic colorectal surgery significantly improves postoperative pain control and reduces opioids. However, it does modify postoperative bowel function. 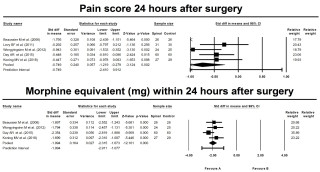
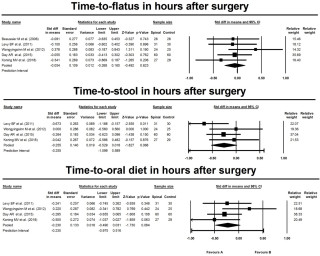
|
||
|
PSGVC108
Allergy transfer from donor to recipient in lung transplantation – a case report
Bianca Battilana, Zurich
AbstractBackgroundAllergy transfer from donor to recipient is an extremely rare phenomenon, with few peanut allergies reported. Only one case of drug allergy transfer was published after lung transplantation. We report a case of severe anaphylaxis-type drug allergy transfer during lung transplantation. Case_presentationA 62-year-old female with end-stage COPD GOLD 4 without any history of allergy was listed for lung transplantation. The 57-year-old female donor with moderate asthma, died of an anaphylactic reaction to ciprofloxacin treatment with severe bronchospasm. Initial assessments of the donor lungs were promising with a P/F-ratio of 368, unremarkable bronchoscopy and good compliance. Following implantation of the first (right) lung, there was an inability to ventilate the graft, characterized by persistent hyperinflation and strongly reduced compliance, prompting the decision for unilateral transplantation. Afterwards, unilateral left-sided ex-vivo lung perfusion (EVLP) was performed for further investigation and poor compliance persisted over the evaluation period. Post-transplant, the patient experienced multiple allergic reactions to Amphotericin B causing bronchospasm. Respiratory decompensation required reintubation, tracheostoma placement, vv-ECMO, and ultimately due to weaning failure unilateral left-sided lung transplantation on the POD 52. After the second transplantation, the patient was weaned promptly. In the most recent follow-up (5-months post-transplantation) she is mobile without oxygen supplementation in the outpatient rehabilitation process. Aside from lethal ciprofloxacin allergy the donor showed high spec. IgE to tropomyosin, arginin kinase and peanut storage proteins. The recipient’s ciprofloxacin sensitivity results were inconclusive, however, total IgE-levels remained elevated. There were no specific IgE detected pre-or 1-month post transplantation. Examination of the left donor lung from the first transplantation revealed significant edema, bronchial changes, and eosinophilia. A complete allergy work up is in progress. ConclusionAllergy transfer in organ transplantation is rare but can have detrimental consequences. Donors with a history of anaphylaxis require careful evaluation and should undergo thorough evaluation in an EVLP setting. 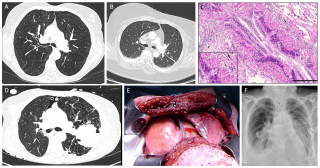
|
||
|
PSGVC110
Clinical outcomes of kidney transplant in obese recipients: a retrospective study
Eliot Melera, Lausanne
AbstractBackgroundThe prevalence of obesity worldwide has steadily increased in recent decades. The impact of recipient obesity on kidney transplant outcomes remains unclear. AimsThe study aims were to determine the effect of recipient obesity on surgical and graft outcomes. MethodsA single-institution retrospective study was performed on adult kidney transplant recipients from 01/2000 to 12/2023. Recipients were classified based on body mass index (BMI) at the time of transplantation: obese (BMI ≥ 30 kg/m2) and nonobese recipients (BMI < 30 kg/m2). The analysis included surgical complications, delayed graft function (DGF), and 1-year estimated glomerular filtration rate (eGFR). ResultsOverall, 941 recipients were studied, including 153 (16.3 %) with BMI ≥ 30 kg/m2. Mean age was 52 years, mean BMI was 24.9 kg/m2, 627 (66.6%) were men, and 362 (38.5%) received a kidney from a living donor. Obese patients had comparable postoperative major complication (Clavien > 3a) rates (26.6 vs 33.3%, p=0.221) and mean comprehensive complication index (21.9 vs 20.2, p=0.092). DGF (20.0% vs 14.0%, p=0.082) and eGFR (52 vs 51 ml/min/1,73m2, p=0.541) were not statistically different in obese and nonobese recipients. ConclusionPostoperative surgical outcomes and 1-year graft function were comparable between obese and nonobese recipients. Consequently, kidney transplantation should be considered in obese recipients. |
||
|
PSGVC111
Extended Storage of Rat Lungs at 4°C and 10°C Exhibits Differential Effects on the Vascular Reactivity of Pulmonary Arteries and Veins
Manon Allouche, Epalinges / Lausanne
AbstractBackgroundBackground: Cold storage at 4°C has been the gold standard for organ preservation, but recent studies suggest that storage at 10°C may offer superior protection by reducing cold-induced damage. However, the effects of these temperatures on pulmonary vascular reactivity are still underexplored.
AimsPurpose: To evaluate the impact of lung preservation at 4°C vs. 10°C on pulmonary vessel vascular reactivity in a rat model. MethodsMethods: Lungs from male Sprague-Dawley rats (n=6-7) were stored at 4°C or 10°C in Perfadex® for 17 hours. Segments (n=2/vessel, 2 mm) of pulmonary artery (PA) and vein (PV) were mounted in organ chambers with oxygenated Krebs-Ringer solution. Isometric tension was measured using a strain gauge connected to an amplifier. Maximal tension to potassium (100 mM) was recorded, followed by concentration-response curves for PA (phenylephrine, U46619) and PV (U46619, serotonin). Endothelium-dependent (acetylcholine) and independent (diethylamine NONOate) relaxation responses were recorded in PA and PV precontracted with U46619. Data were compared between storage groups using analysis of variance, with control vessels (n=3) for control purposes. Statistical significance was set at 0.05. ResultsResults: Prolonged storage at 4°C significantly reduced PA contractility to phenylephrine, whereas PA from the 10°C group showed better preservation of contractility. Veins from both groups showed similar reductions in contraction to all agents. Endothelium-dependent relaxation of PA was similar across all groups. Endothelium-independent relaxation of PV was higher in the 4°C group compared to controls and 10°C group.
ConclusionConclusion: Both 4°C and 10°C storage reduce pulmonary vessel contractility, with better preservation at 10°C for PA. Neither temperature affects endothelium-dependent relaxation. Further studies are needed to explore the underlying mechanisms and assess pulmonary vasoreactivity after transplantation following cold storage at 4°C or 10°C. 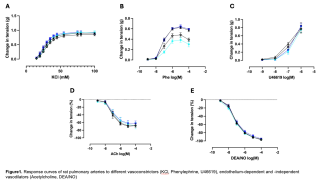
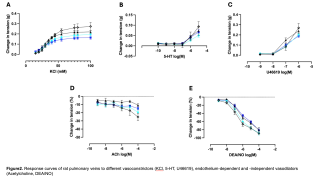
|
||
|
PSGVC112
Peritoneal Recurrence Following Laparoscopic vs. Open Gastrectomy for Gastric Adenocarcinoma
Laura Didisheim, Lausanne
AbstractBackgroundDespite surgical resection representing the mainstay of curative treatment for gastric adenocarcinoma, the risk of postoperative recurrence remains substantial. Among the various patterns of relapse, peritoneal recurrence is often associated with poor outcomes. Although laparoscopic gastrectomy (LG) has become increasingly adopted in clinical practice, its specific impact on peritoneal recurrence rates compared to open gastrectomy (OG) remains to be fully elucidated. AimsThe aim of this study was to evaluate the risk of peritoneal recurrence following curative-intent LG versus OG. MethodsAll consecutive patients with gastric adenocarcinoma undergoing oncologic gastrectomy with curative intent between January 2007 and December 2021 were retrospectively analyzed. Clinico-pathological characteristics, survival and recurrence were compared between LG and OG patients. The x2 test was used for categorical variables and the t-test for continuous ones. Survival was assessed with the Kaplan-Meier method and log-rank test, as well as a multivariable Cox regression analysis. ResultsA total of 145 patients were included in the study, 99 (68.3%) in the OG group and 46 (31.7%) in the LG group. Baseline demographics, surgical and staging characteristics were similar in both groups. There was no significant difference in 5 year overall survival (59.2% for OG, 39.5% for LG, p=0.976) and recurrence rate (44.3% for OG and 28.3% for LG, p=0.066). Recurrence patterns were likewise comparable, with locoregional recurrence in 7.7% after LG versus 9.3%, and distant recurrence in 84.6% versus 76.7%. Mixed types of recurrences were found in 7.7% versus 14% (p=0.810). However, a significant difference emerged in the rate of peritoneal recurrence, which was higher after OG (31.3%) compared to LG (15.2%, p=0.040). ConclusionOur findings indicate a potential benefit of laparoscopic gastrectomy in reducing peritoneal recurrence compared with open gastrectomy. Further studies are warranted to confirm these preliminary observations and clarify the underlying mechanisms. |
||
|
PSGVC114
Feasibility and Procedural Evaluation of Converting Prior Antireflux Surgery to RefluxStop in Gastroesophageal Reflux Disease: Experience from 24 Clinical Cases
Thorsten G. Lehmann, Friedrichshafen DE
AbstractBackgroundFailure of anti-reflux surgery (ARS) necessitating repeated intervention is common and ranges between 10-60% depending on follow-up time and procedure used. Resurgence of reflux symptoms, dysphagia, migration/erosion, or device explant are the most common reasons for re-surgery, often including recurrence of hiatal hernia. However, technical characteristics inherent to ARS may restrict subsequent options, presenting challenges in determining the most appropriate course after ARS failure. AimsFeasibility and surgical considerations of failed ARS conversion to RefluxStop surgery were evaluated. MethodsThis retrospective two-centres study utilized data from patients experiencing different ARS failures converted to the RefluxStop procedure (n=24). ResultsPatients (n=24) underwent RefluxStop surgery after failed ARS, including magnetic sphincter augmentation (MSA) (38%), Toupet fundoplication (29%), Nissen fundoplication (13%), Dor fundoplication (8%), BICORN (8%), and EndoStim (4%) (Table 1). RefluxStop surgery was feasible, irrespective of the type of prior ARS in all cases. When indicated, hernia repair precedes conversion. At 1-year follow-up all patients had discontinued regular daily PPI use. In one case, the RefluxStop device asymptomatically early penetrated into the stomach cavity and was naturally expelled through the digestive tract; no re-intervention needed. It is known from the learning curve of the RefluxStop procedure that a too tight sutured pouch may force early penetration through the stomach wall, which is why extended fundal dissection is recommended if the fundus is small. However, this particular case was presumably caused by weakened fundic musculature with very thin fundus wall without muscles, and further experience of such cases with extremely thin fundus wall is recommended. ConclusionConversion to RefluxStop is feasible irrespective of type of prior ARS failure of which fundoplication often requires careful vagal nerve handling, hiatal repair, and plication dissection. Although conversion from fundoplication may be more challenging due to fundus tissue fibrosis, conversion from both fundoplication and MSA are straightforward. 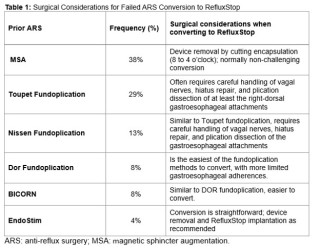
|
||
|
PSGVC115
The impact of staging laparoscopy and peritoneal washing in gastric cancer – state of the art or outdated?
Kerstin Neuschütz, Lucerne
AbstractBackgroundAccording to some guidelines staging laparoscopy can aid in decision-making in gastric cancer and is recommended prior to neoadjuvant chemotherapy. However, diagnostic laparoscopy is not routinely performed and its impact on treatment regimens is questionable. AimsThe aim of this study is to assess the implementation and impact of a staging laparoscopy and peritoneal washing in patients surgically treated for gastric cancer and Siewert III carcinomas at our institution. MethodsThis is a single-center retrospective cohort study. Patients who underwent surgical treatment for gastric cancer between 2011 and 2023 were included. The incidence and consequence of staging laparoscopy and peritoneal washing were analyzed. ResultsIn total 184 patients underwent surgical treatment for gastric cancer. 110 (60%) received a staging laparoscopy. In 57 (52%) a peritoneal washing was performed, of which 6 (11%) revealed a positive cytology. Staging laparoscopy revealed 10 patients (9%) with macroscopic peritoneal tumor lesions. 6 of these patients additionally received peritoneal washing and despite macroscopic tumor lesions, only 3 (50%) had a positive cytology. The chosen therapeutic pathway of the 10 patients with macroscopic lesions drastically varied - from palliative gastroenterostomy, to palliative gastrectomy, to chemotherapy and a form of gastrectomy with or without HIPEC. The 3 patients with no macroscopic lesions but positive cytology were all treated with chemotherapy followed by gastrectomy. Survival of patients with macroscopic and/or microscopic tumor lesions also varied - from deceased within the first 90 days postoperatively to alive and without tumor recurrence at 5-year follow-up. ConclusionIn our experience, performing a diagnostic laparoscopy does not commonly have therapeutic consequences. Furthermore, peritoneal washing and its cytology findings do not correlate with macroscopic peritoneal lesions. The diagnostic value of a staging laparoscopy is questionable and should be reserved for individual cases. |
||
|
PSGVC116
Learning Curve of Robotic-Assisted Hiatal Hernia Repair: A Cumulative Summation Retrospective Analysis of Adjusted Operative Times
Francesco Mongelli, Bellinzona
AbstractBackgroundIn surgery, the learning curve refers to the period during which a surgeon attains proficiency in a specific surgical procedure. The widespread adoption of robotic systems has posed new challenges to surgeons and surgical trainees. Surgeons have had to learn new techniques and instrumentation, requiring significant time and the development of new surgical skills. To date, few articles have been published regarding learning curves of robotic-assisted hiatal hernia repair. AimsThe aim of this study was to assess the learning curve of robotic-assisted hiatal hernia repair. MethodsPatients undergoing robotic-assisted hiatal hernia repair from May 2018 to April 2024 were retrospectively included. Clinical characteristics, operative times, and postoperative data were collected. A cumulative summation (CUSUM) analysis of operative times, adjusted for surgical complexity, was conducted. ResultsWe selected 101 patients who underwent robotic-assisted hiatal hernia repair performed by three surgeons. The mean age was 65.7±14.3 years, with 69 (68.3%) female patients. Fig1. Adjusted operative times were calculated based on hernia type, age, sex, BMI, and ASA score. The CUSUM analysis estimated the learning curve to be between 15 and 21 cases. Fig2. Only one minor intraoperative complication occurred. Postoperatively, 19 (18.8%) complications were observed, with only 3 (3.0%) classified as grade 3 according to the Clavien-Dindo classification. Fig3. Complications were evenly distributed between the learning and post-learning phases. After a mean follow-up of 26.5±18.0 months, 13 (12.9%) cases of recurrence were recorded, none of which required surgical revision. ConclusionOur findings showed that experienced surgeons performing robotic-assisted hiatal hernia repair have a rapid learning curve. Specifically, we observed a significant reduction in operative time after completing an estimated 15 to 21 cases. Intraoperative and postoperative complication rates were low and evenly distributed during and after the learning phase, underscoring the procedure's safety and effectiveness in experienced surgical teams. 
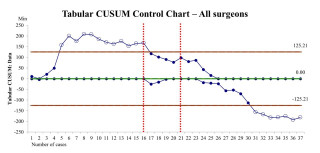
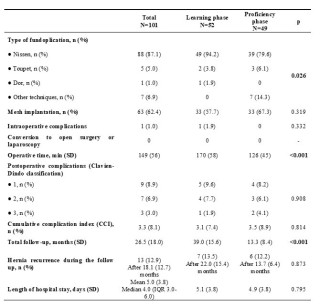
|
||
|
PSGVC117
Giant Duodenal Brunneroma: Report of a Rare Case and Review of the Literature
Dimitrios Chatziisaak, St.Gallen / St. Gallen, Lausanne / Lausanne, St. Gallen
AbstractBackgroundBrunneromas are exceedingly rare benign tumors originating from Brunner’s glands in the duodenum. These lesions often remain asymptomatic or present vague symptoms, making diagnosis challenging. While typically benign, their differentiation from malignant lesions is crucial. Timely surgical or endoscopic management ensures an excellent prognosis. This report highlights a case of a giant Brunneroma causing gastrointestinal bleeding and anemia, managed with duodenum-preserving excision. Case_presentationA 39-year-old male presented with a 2-month history of melena, intermittent epigastric pain, and anemia. A CT scan revealed a large (8 cm) tumor in the second segment of the duodenum (Image 1.). Endoscopy confirmed a polypoid mass, with biopsies suggesting a hypertrophic Brunner’s gland polyp (Image 2.). The multidisciplinary team recommended duodenotomy with radical tumor excision. Surgery involved resection of a 7.5×5.1×4.1 cm tumor near the ampulla of Vater, preserving duodenal integrity (Image 3.). Postoperative recovery was uneventful, requiring only a single-unit blood transfusion. Histopathology confirmed a benign Brunneroma without malignant features. Follow-up endoscopy at 3 months showed no recurrence. ConclusionGiant Brunneromas, although rare, should be considered in the differential diagnosis of upper gastrointestinal lesions causing bleeding or obstruction. Accurate diagnosis through imaging, endoscopy, and multidisciplinary evaluation is essential. Surgical excision remains the definitive treatment for large or symptomatic lesions, ensuring excellent outcomes and minimal recurrence risk. This case emphasizes the importance of interdisciplinary collaboration and tailored surgical approaches for optimal patient care 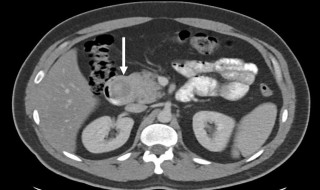


|
||
|
PSGVC118
Twelve-month Clinical Outcomes Following RefluxStop Surgery: First 100 Patients from a Swiss Institution
Yannick Fringeli, Bern
AbstractBackgroundThe RefluxStop procedure for the treatment of gastroesophageal reflux disease (GERD) restores key components of the antireflux barrier without encircling the food passageway, thereby avoiding adverse effects common to traditional antireflux surgical techniques. This procedure is offered at our clinic, following the excellent outcomes reported in clinical trial. However, many of the patients seen in clinical practice have more complex clinical characteristics, such as large hernias or comorbid motility disorders, which may influence outcomes. AimsTo provide real-world outcome data on patients undergoing RefluxStop surgery, inclusive of a complex patient population. MethodsThis retrospective study analyzed outcomes at 12 months in 100 consecutive patients to undergo RefluxStop surgery at a single Swiss institution. The primary effectiveness outcome was GERD Health-Related Quality of Life (GERD-HRQL) score. Secondary outcomes included patient satisfaction, proton pump inhibitor (PPI) use, and adverse events (AEs). ResultsTable 1 shows patient characteristics. Total GERD-HRQL score (0-75 points) decreased from a median (IQR) of 41 (28.75-50) preoperatively to 1 (0-5) at 12 months (p<0.001), with 92% of patients reporting satisfaction. PPI usage was discontinued in 92%, whereas preoperatively 95% required PPIs. AEs included: early device penetration to the stomach (n=1) ascribed to overly tight suturing of the invagination pouch, no intervention required; device dislocation (n=1) ascribed to insufficient closure of the pouch/deployment tool channel; and re-do hiatal repair unrelated to the device sitting intact in its pouch (n=3), all three in patients with very large (>7 cm) hiatal hernia. ConclusionThis study provides favorable real-world evidence on the RefluxStop procedure in a population of substantially severe sufferers that included esophageal motility disorder (66%) and hiatal hernia >3 cm (55%), with excellent effectiveness quantified by GERD-HRQL score and supported by patient satisfaction and PPI discontinuation in the context of a low rate of AEs. 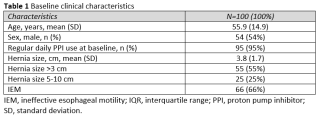
|
||
|
PSGVC119
Dedifferentiated Liposarcoma of the Esophagus: A Case Report
Noemi Fischer, Bern / 3010
AbstractBackgroundLiposarcomas represent the most common soft tissue tumors, accounting for one in five mesenchymal malignancies. While these tumors are typically found in the retroperitoneum and extremities, gastrointestinal liposarcomas are exceedingly rare with an incidence from 0.1% to 5.8% at autopsy. Case_presentationThis case report details a 73-year-old female patient who presented with a foreign body sensation, dysphagia, and an inability to sing, symptoms that had progressively worsened over the past year, culminating in an episode of airway obstruction. An initial investigation with a fiber-endoscopy yielded normal results, but a barium swallow suggested a possible Zenker’s diverticulum. Subsequent gastroscopy revealed an obstructing subendothelial lesion in the proximal esophagus, leading to a differential diagnosis that included gastrointestinal stromal tumor (GIST), lipoma, and leiomyoma. Surgical intervention via cervicotomy and local excision in toto was performed, and histological analysis identified an ulcerated mesenchymal neoplasia measuring 3.5 cm. Despite inconclusive initial molecular analyses, further testing revealed MDM2 FISH gene amplification and mitotic activity, indicating malignant potential. Ultimately, genome-wide DNA methylation analysis confirmed the diagnosis of dedifferentiated liposarcoma. ConclusionOur multidisciplinary tumorboard decided on a low risk scheme follow up with either gastroscopies or CT scans every six months in accordance with the S3 guidelines for adult soft tissue sarcomas, as the mass was graded a histopathological G1. Exact identification and appropriate management are crucial for improving patient outcomes, as exemplified by the timely surgical intervention and subsequent monitoring in this case. 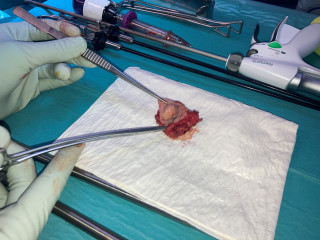

|
||
|
PSGVC120
From Obesity to Oncology Resolution: MALT Lymphoma Healed Post-Bariatric Surgery
Boris Duran, Schaffhausen
AbstractBackgroundNon-Hodgkin lymphomas (NHL) account for 2-3% of all cancers, with mucosa-associated lymphoid tissue (MALT) lymphomas representing approximately 7-8% of NHL cases. Gastric MALT lymphoma is primarily linked to Helicobacter pylori infection, and it is typically managed with non-invasive therapies, including eradication, radiotherapy, and chemotherapy. As a result, surgery is not commonly recommended as a first-line treatment. Case_presentationWe present a case of a 52-year-old male with stable stage I1E gastric MALT lymphoma in the mid and distal gastric corpus who underwent laparoscopic 4/5 gastrectomy with Roux-Y reconstruction as part of a bariatric procedure. The patient, who had a history of obesity (BMI 40 kg/m²) and gastroesophageal reflux disease, initially presented in September 2019 with melena and epigastric pain. Diagnostic gastroscopy and colonoscopy confirmed gastric MALT lymphoma. After successful eradication of H. pylori, follow-up endoscopies revealed persistent lesions without progression. The patient was managed with a watch-and-wait strategy over 4 years, avoiding systemic therapy or radiotherapy. In June 2023, the patient sought bariatric counseling, and a repeat gastroscopy confirmed persistent lymphoma. Given the tumor’s location and potential complications of radio-chemotherapy on future bariatric surgery, we opted for a primary resection via a modified gastric bypass. The lesion was marked endoscopically, and laparoscopic 4/5 gastrectomy with confirmed tumor-free margins and Roux-Y reconstruction was performed. Postoperatively, the patient experienced successful weight loss with no recurrence of the lymphoma. ConclusionThis case suggests that surgical resection may be considered for stable, localized gastric MALT lymphoma, particularly in younger patients, offering the advantage of avoiding lifelong follow-up. Additionally, gastric MALT lymphoma may not be a contraindication to bariatric surgery, depending on tumor location and stage. Further research is needed to evaluate the role of surgery in such cases. |
||
|
PSGVC121
Gastric Leiomyoma: A Case Report
Valérian Tanner, Fribourg
AbstractBackgroundGastric leiomyoma is a benign submucosal tumor, accounting for 2.5% of gastric neoplasms. It is often asymptomatic but can cause bleeding due to mucosal ulceration. On imaging, it appears as a filling defect in the gastric wall, and endoscopy reveals it as a submucosal mass with tenting and loss of gastric folds, known as "Schindler's sign". The standard treatment is leiomyomectomy. This case report presents a gastric leiomyoma treated with laparoscopic gastrotomy and transgastric leiomyomectomy, guided by intraoperative endoscopy. Case_presentationAn overweight 44-year-old male presented with symptoms of bloating and diffuse abdominal pain. A CT scan identified a 3 cm endoluminal mass in the posterior gastric wall near the cardia. Endoscopic examination revealed a 3 cm submucosal mass, with no gastric mucosa abnormalities (Figure 1). Histopathological analysis of endoscopic biopsies diagnosed a leiomyoma, with immunohistochemistry showing sparse expression of c-kit, DOG1, and CD34, consistent with a wild-type gastrointestinal stromal tumor (GIST). Elective laparoscopic gastrotomy and transgastric leiomyomectomy (Figure 2), guided by intraoperative gastroscopy (Figure 3) was performed. Surgical specimen histopathology confirmed the complete resection of a gastric leiomyoma. Expression of c-Kit, DOG1 and CD34 was diagnostic of interstitial Cajal cells. Recovery was uneventful, and the patient was discharged on postoperative day 5. At 6-week follow-up, he reported no pain and he tolerated normal diet well. ConclusionGastric leiomyoma is a rare, paucisymptomatic tumor with GIST as the main differential diagnosis. Diagnosis requires radiological, endoscopic, and specialized pathological analyses. In our experience, endoscopic guided laparoscopic gastrotomy with transgastric leiomyomectomy provided excellent results. 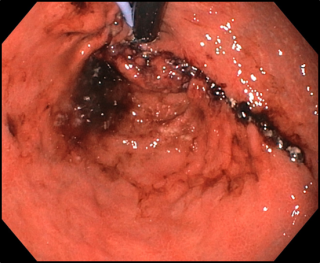
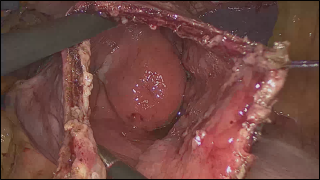
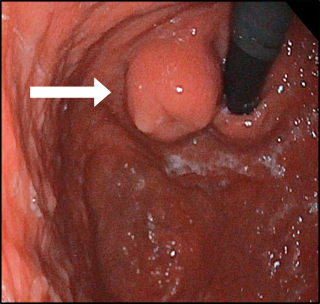
|
||
|
PSGVC122
Jejunal diverticulitis: a case series report
Elise Betz, Schaffhausen
AbstractBackgroundThe incidence of jejunal diverticula (JD) is up to 6%, highest prevalence in the elderly. These pseudodiverticula are typically located near to mesenteric fat and 10% to 30% may develop complications (diverticulitis, hemorrhage, obstruction or perforation). Clinical presentation of JD is often nonspecific (abdominal pain, nausea, vomiting, or acute abdomen). Due to its rarity there are no guidelines. This case series contributes to the limited literature on JD by detailing clinical presentation, diagnostics and management in three patients. Case_presentationCase 1 An 82-year-old male presented with lower abdominal pain, peritonitis and elevated inflammatory markers. CT angiography revealed small bowel wall thickening, mesenteric air, and free fluid, suggesting perforation. Emergency laparotomy confirmed purulent peritonitis and jejunal diverticular perforation; segmental resection and anastomosis were performed, recovery was uneventful. Case 2 An 83-year-old male presented with palpable abdominal mass but otherwise asymptomatic. CT revealed a suspicious jejunal lesion. Explorative laparotomy identified JD with chronic perforation, excluding malignancy; segmental resection with anastomosis was performed. Upper GI bleeding was managed with blood transfusions, discharge was on POD 6. Case 3 An 82-year-old male with history of small and large bowel diverticulosis presented with peritonitis, vomiting, and fever. Imaging suggested diverticular perforation. Laparoscopy revealed jejunal perforation and peritonitis; open segmental resection and anastomosis were performed. The patient required ICU care for septic shock but recovered uneventfully and was discharged on POD 6. ConclusionJejunal diverticulitis poses a diagnostic challenge due to nonspecific symptoms. We described three cases of complicated JD with varying presentations and management: Two required urgent surgery for perforation, while one underwent elective surgery for chronic inflammation. These cases highlight the need of suspicion of JD in acute or chronic abdominal symptoms, with prompt imaging and a tailored approach for optimal outcomes. Our findings contribute to the evidence that JD, though rare, should be considered in the differential diagnosis of abdominal pain. |
||
|
PSGVC123
Comparing Laparoscopic and Robot-Assisted Surgery: A Subjective Evaluation of Surgeon and Assistant Workloads Using the NASA Task Load Index at a Single Center
Hélène Gros, Basel / San Diego
AbstractBackgroundWith the rise of minimally invasive surgery, attention to ergonomic challenges for the operating team has increased, as they can lead to musculoskeletal disorders and decreased performance of surgeons. However, their impact on assistants remains unclear. AimsThis study aims to investigate the correlation of ergonomics and robot-assisted versus laparoscopic surgery for surgeons and assistants. MethodsThis study was conducted prospectively in a single center between 1/5/2024 and 31/12/2024. Procedures routinely performed with both techniques were included (sigmoidectomy, right and left hemicolectomy, fundoplication, left pancreatectomy, rectopexy, and low anterior resection). To assess ergonomics, mental and physical workload were examined using primarily the NASA-TLX score. Information was collected using a postoperative RedCap survey and patient charts. ResultsA total of 108 operations (46.3% laparoscopic, 53.7% robot-assisted) with 243 survey responses (154 as surgeons, 89 as assistants) were included. In the surgeon group, 73.2% were male and 26.8% were female, while in the assistant group, 34.83% were male and 65.2% were female. The mean operation time was shorter for laparoscopic procedures (180.2 vs. 274.2 minutes). Height (centimeter) was 174.48 in the assistant group versus 179.72 in the surgeon group. Prior presence of back pain was significantly higher for assistants than for surgeons (p<0.0001). When comparing laparoscopy and robot-assisted surgery, only physical demand was significantly higher for surgeons (58.26 versus 40.70), p<0.0001). No significant differences were reported by surgeons for mental demand (59.64 vs. 63.60, p=0.7840), temporal demand (50.74 vs. 52.68 p=0.8416), performance (65.90 vs. 70.49, p=0.3322), effort (64.06 versus 69.68, p=0.3322), or frustration (38.24 vs. 40.59, p=0.9078). Similarly, no differences were noted for assistants across both access modes. ConclusionOur preliminary analysis indicates that robot-assisted procedures reduce surgeons' physical workload without affecting assistants' workload. |
||
|
PSGVC124
Another Case of GIST-plus Syndrome?
Eleonora Garosi, Lugano
AbstractBackgroundGIST-plus syndrome or PDGFRA-mutant syndrome is an extremely rare condition related to a germline mutation of PDGFRA which causes sporadic gastrointestinal stromal tumor (GIST) and inflammatory fibroid polyps (IFP). Case_presentationA 44-year old healthy man was referred to out-patient clinic for long-standing, colicky, diffuse abdominal pain, nausea and vomiting. He reported of feeling feverish with night sweats, a weight loss of 8 kg in the last year, and fatigue. Laboratory tests showed carential anemia, thrombocytosis and mild inflammatory syndrome. Abdominal CT scan revealed a distal invagination of the small bowel. After a not-conclusive colonoscopy, a multidisciplinary discussion recommended a surgical resection. The patient underwent exploratory laparoscopy converted into laparotomy finding a large intestinal mass causing invagination and two implants in the lesser gastric curvature. Other multiple smaller intestinal lesions were found after enterotomy. The major lesion and one of the gastric implants were resected. An ileal end-to-end anastomosis and a regional lymphadenectomy were performed. The patient developed a post-operative paralytic ileus that was conservatively treated and had finally a full recover. Final pathology revealed a gastric GIST and an ileal IFP which both consisted of densely cellular areas of spindle cells without necrosis. Next Generation Sequencing analisys found a Variant of Unknown Significance (VUS) for PDGFRA gene, although exons 12, 14, 18, which are usually mutated in GIST-plus syndrome, were wild-type. The patient is waiting for formal genetic workup with germline testing and gastroscopy. ConclusionGenetic testing in case of concomitant GIST and IFP is mandatory for assessing if mutation of PDGFRA gene is present and if it is germline. Besides some renowned mutations, other genetic variants might be culprits, being potentially targeted by immunomodulation therapies. |
||
|
PSGVC125
A Case Report on the DAVOS Approach for Sacroiliac Bone Sarcoma Resection
Theodoros Loupasis, Zürich / Zurich
AbstractBackgroundResecting sacroiliac sarcomas is challenging due to complex anatomy, proximity to critical neurovascular structures, and the need for multidisciplinary coordination. Achieving clear margins, functional preservation, and stable reconstruction demands meticulous planning AimsThis case highlights a rare sacroiliac bone sarcoma and the successful application of the DAVOS (Direct, Adaptable, Vigilant, Oriented, Specialized) surgical approach for R0 resection. It underscores the importance of preoperative planning and precise techniques for favorable outcomes. MethodsA 34-year-old female with mesenchymal chondrosarcoma in the sacroiliac region underwent neoadjuvant chemotherapy and proton beam therapy. ResultsThe DAVOS Approach enabled a left internal sacroiliac hemipelvectomy in floppy lateral decubitus and jackknife positioning for optimal visualization. A T-shaped incision allowed retroperitoneal access by dissecting abdominal wall musculature, thoracolumbar fascia, and paraspinal muscles. The internal iliac vessels were ligated, and the rectum mobilized. The surgical team performed sacral laminectomy with ligation of ipsilateral S1–S3 nerve roots. Osteotomies extended from the greater sciatic foramen to the iliac crest and through the sacrum, exiting caudally at S4 and cranially below the S1 endplate. Reconstruction included lumbopelvic stabilization and fibula allograft reinforcement. A biologic mesh protected the rectum and minimized herniation risks. Wound closure was completed with a multilayer technique. ConclusionThe DAVOS Approach allows full exposuere for the precise resection with enhanced visualization, achieving clear margins while preserving function. Its adaptability makes it a valuable technique for complex tumor resections. 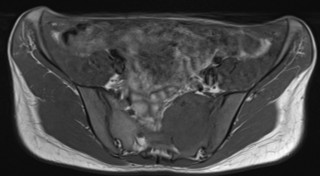

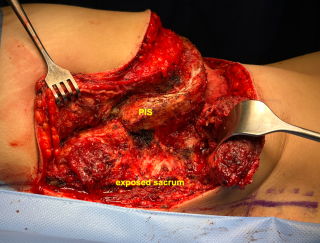
|
||
|
PSGVC126
Comparative Study of Tensile Strength in Vicryl™ vs. Prolene™ 5-0 Knots: Impact of Throw Type and Count
Clelia Dogny, Grand-Saconnex / genève
AbstractBackgroundKnots are the weakest point of sutures, making their security and tensile strength critical. While suture material and the number of throws substantially affect knot strength, surgeon’s knots and suture size appear less influential. To our knowledge, however, there has been no study investigating the effect of multiple consecutive surgeon’s knots on tensile strength. AimsTo determine whether the use of multiple throws of double overhand (surgeon’s) knots or single overhand knots affects the knot's tensile strength and the elongation of the suture’s loop with Vicryl™ and Prolene™ sutures. MethodsVicryl™ and Prolene™ 5-0 sutures were tied in knots of three, four, and five throws, across twelve different knot sequences: single knots only, surgeon’s knots only, and an increasing number of surgeon’s knots. Samples were tested using a tensiometer applying a constant force until knot failure or slippage. ResultsThe tensile strength of the knots increased significantly with the number of throws and the presence of surgeon’s knots (p<0.005). Five-throw knots were stronger than three-throw knots regardless of the number of surgeon’s knots for both types of sutures. The use of surgeon’s knots only significantly increased strength in the three-throw series for both Prolene™ and Vicryl™ sutures. For both sutures, a three-throw surgeon’s knot showed the same tensile strength as a five-throw simple knot. Loop elongation depended on the number of throws and surgeon’s knots. ConclusionThe use of surgeon’s knots alone increased knot’s breaking resistance without needing additional throws of simple knots. A three-throw surgeon’s knot provides breaking resistance equivalent to a knot with more throws. If reduced loop elongation is desired, the choices would be four surgeon’s throws for Vicryl™ and five simple throws for Prolene™ |
||
|
PSGVC128
Complications of Prosthetic Breast Reconstruction in Prophylactic Versus Therapeutic Mastectomy: A Systematic Review and Meta-Analysis
Marlene Schelletter, Genève AF / Geneva AF
AbstractBackgroundAlthough not routinely advocated for average-risk patients, contralateral prophylactic mastectomy (CPM) is recommended by current guidelines to reduce mortality in high-risk patients with unilateral breast cancer. AimsThis systematic review and meta-analysis aims to provide a comprehensive quantitative assessment on the risk associated with implant-based reconstruction in CPM versus therapeutic mastectomy (TM). MethodsA priori criteria were applied to perform a systematic review and meta-analysis of all existing comparative studies on postoperative complications associated with implant-based breast reconstruction after CPM or TM. The fixed-effects model was used to calculate Odds Ratios (ORs) and 95% confidence intervals (CIs). ResultsFive studies were included in the final analysis, representing 3543 patients who underwent 6401 mastectomies (3260 TM and 3141 CPM), followed by prosthetic breast reconstruction including Tissue Expanders and Direct-to-implants (Table 1, Figure 1). Reconstructions after TM were associated with a statistically significant higher risk of postoperative infections [I; OR = 2.03 (CI: 1.50, 2.73)] (Figure 2) and explantation rates [EX; OR = 2.41 (CI: 1.77, 3.28)] (Figure 3). No significant differences were observed between the two groups in the occurrence of hematoma, seroma, necrosis and capsular contracture (Figure 4-7). ConclusionCPM demonstrates a lower risk of postoperative complications compared to TM for implant-based breast reconstruction. This knowledge and the quantification of risk summarized in this paper should be integrated in the shared decision making with patients and in pre-operative information. 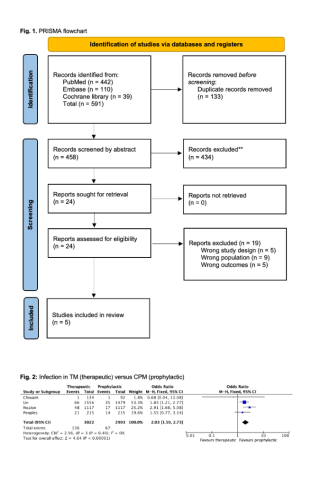
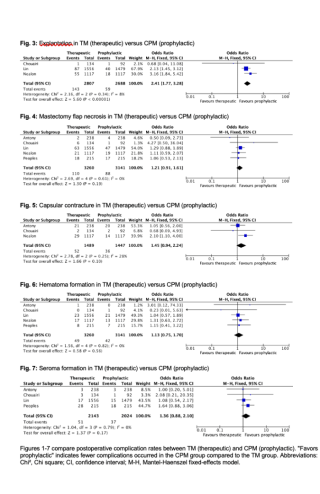
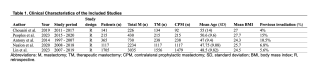
|
||
|
PSGVC129
Safety and efficacy of cisplatin and nab-paclitaxel pressurized intraperitoneal aerosol chemotherapy (PIPAC) in patients with peritoneal carcinomatosis: Nab-PIPAC phase IB study
Frédéric Ris, Geneva
AbstractBackgroundPlatinum and taxanes are backbone chemotherapy in multiple solid tumors but their combination through PIPAC has not been investigated in peritoneal carcinomatosis. AimsTo investigate the use of Nab Paclitaxel and Cisplatine in PIAC, as the first phase 1 study in the world. MethodsNab-PIPAC is a phase IB trial investigating PIPAC administration of cisplatin at 10.5 mg/m2 and escalating dose of nab-paclitaxel with a 3+3 design (7.5, 15, 25, 37.5, 52.5 and 70 mg/m2). PIPAC was repeated at 4-6 weeks intervals for up to three courses. ResultsWe enrolled 22 patients with previously treated peritoneal carcinomatosis, of whom 18 received at least one PIPAC: 6 ovarian, 9 gastric and 3 pancreatic cancers. Three patients did not receive PIPAC due to ileus (n=1) or no access to peritoneal cavity (n=2). Median age was 67 years (43-81). In total, 47 PIPAC procedures were administered and 12 of 18 (67%) patients completed three PIPAC cycles. There was no dose limiting toxicity. One patient had grade 3 treatment related adverse event (asthenia). One patient had bladder lesion during a PIPAC procedure and needed surgical reintervention. Median progression-free survival was 3.1 months. Median overall survival (OS) was 9.4 months and OS rate at 1 year was 47.1%. Pharmacokinetic analyses showed good linearity between nab-paclitaxel dose and the exposure i.e., AUC0-last (R2=0.90), and the maximum concentration (R2=0.77). ConclusionThe combination of nab-paclitaxel and cisplatin administered by PIPAC was safe and well tolerated in patients with previously treated peritoneal carcinomatosis. |
||
|
PSGVC130
Comparative Analysis of 2D and 3D Visualization Techniques in Minimal Invasive and Robotic Surgery: A Systematic Review
Dimitrios Chatziisaak, St.Gallen / St. Gallen, Lausanne / Lausanne, St. Gallen
AbstractBackgroundMinimally invasive surgery (MIS) is used due to its advantages and reduced complications in patient recovery compared to open surgery. Visualization during surgery is crucial, and both two-(2D) and three-dimensional (3D) technologies can be employed. However, the comparative effectiveness of these technologies in improving surgical outcomes, particularly in robotic surgery, remains debated. AimsThis systematic review evaluates the impact of 2D versus 3D visualization on safety and performance metrics in robotic and minimally invasive surgery, emphasizing intraoperative blood loss, complication rates, and operative efficiency. MethodsA systematic review was conducted, searching databases including MEDLINE and Cochrane for peer-reviewed studies published from 2015 to 2024. Studies comparing 2D and 3D visualization in laparoscopic and robotic surgery were included, focusing on outcomes such as operative time, blood loss, complication rates, length of hospitalization and task performance. ResultsWe identified a modest reduction in operative time with 3D visualization, particularly in specific procedures like hernia, colorectal surgery, bariatrics and minimal invasive gastrectomy. 3D visualization also improved depth perception, especially for novice surgeons, in robotic setting. However, findings regarding blood loss and complication rates were inconsistent across studies, with no clear consensus regarding on its benefits. ConclusionWhile 3D visualization offers certain performance improvements, particularly in surgical time reduction and depth perception for novice surgeons to some extent, the overall clinical advantages remain variable. The high cost of 3D systems may not always justify their routine use, especially when 2D systems can achieve comparable outcomes. Further research is needed to fully assess the long-term clinical and economic impact of 3D visualization in MIS and robotic surgery. |
||
|
PSGVC131
Multimodal Machine Learning Models for Survival Prediction in Surgical Oncology
Jan Liechti, Allschwil / Basel
AbstractBackgroundIn medicine, machine learning (ML) has demonstrated superior performance for risk prediction compared to conventional statistics. To estimate efficiency of treatments, the prediction of survival is fundamental in surgical oncology. Although data from various sources is available, the prediction models are often limited by single modality input (e.g. medical imaging, text, etc.). While the added value of multimodal analysis remains to be demonstrated, increasing efforts are made to include multimodal data into prediction models. AimsThis systematic review (SR) provides an overview on the use of ML for predicting long-term survival, focusing on multimodality of data. MethodsA systematic literature search was conducted on MEDLINE, Embase, IEEE Xplore and Web of Science according to a prespecified search strategy. Studies using ML to predict overall survival in surgical oncology patients were included. If ML models were not predicting long-term overall survival (≥ 1year) or if performance metrics were not comparable, studies were excluded. Quality assessment was done in accordance with the PROBAST guideline. This SR was registered on PROSPERO (CRD42024529178). ResultsFrom initially 4159 results, 394 were selected for full text review and 134 studies were eventually included. This SR shows that ML for outcome prediction is becoming increasingly popular (Figure 1). Within our SR the organ systems are represented as follows: 38.5% abdominal (n=55), 18.2% CNS (n=26), 13.3% urogenital (n=19), 9.1% cardiothoracic and musculoskeletal (both n=13), 7% breast (n=7), 4.2% ENT (n=6) and 0.7% skin (n=1). Among the included studies, 73.9% used one (n=99) and 26.1% used two modalities (n=35). The modalities are displayed in Figure 2. ConclusionThis SR showed that ML is increasingly used to predict survival in surgical oncology. Prediction models progressively rely on multimodal input and achieve improved performance. Future research must analyze the impact of improved prediction models on management and long-term survival of surgical oncology patients. 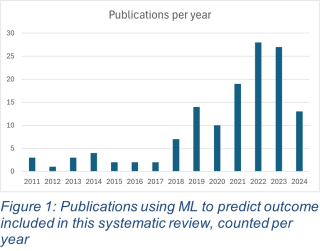
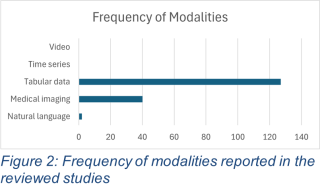
|
||
|
PSGVC132
Robotic-Assisted Full-Thickness Gastric Wall Resection for GIST Using Adjuvant Imaging Technologies - a Robotic Center Experience
Sofia Teixeira Da Cunha, Olten
AbstractBackgroundRobotic-assisted surgery has expanded the scope of minimally invasive techniques in general surgery. This study evaluates the feasibility and safety of robotic-assisted gastric GIST resections, integrating intraoperative diagnostic adjuncts such as endoscopy, laparoscopic ultrasound, and near-infrared fluorescence imaging (NIFI). AimsTo assess the feasibility and safety of robotic-assisted gastric GIST resections performed in our robotic center with advanced imaging technologies. MethodsBetween November 2018 and January 2023, ten patients underwent robotic-assisted surgery for gastric GISTs using the da Vinci Xi system. Procedures incorporated real-time imaging technologies: intraoperative endoscopy, laparoscopic ultrasound, and NIFI via the Firefly system. Patient demographics, perioperative parameters, and clinical outcomes were descriptive analysed. ResultsThe median patient age was 64 years (range: 36–84). Eight patients underwent full-thickness resections, and two had wedge resections. Intraoperative adjuncts were utilised in all cases to localize tumours and ensure vascularised anastomoses. The median operative time was 132.5 minutes, and the median hospital stay was 6 days. Complications included three cases of postoperative bleeding (Clavier-Dindo I-II), with no anastomotic leaks or intra-abdominal infections. Final pathology confirmed R0 resection in 70%, and no recurrences were observed during a median follow-up of 27.5 months. ConclusionRobotic-assisted gastric GIST resection with intraoperative imaging technologies is safe and effective, offering precise tumor localisation, enhanced visualisation. These findings support the integration of robotic platforms with advanced diagnostics for complex minimally invasive surgeries. |
||
|
PSGVC133
RATS Sleeve Left Lower Lobe Lobectomy and Mediastinal Lymphadenectomy in a Carcinoid Tumor Case
Minou Mohajeri, Zürich
AbstractBackgroundRobot-assisted thoracic surgery (RATS) has gained popularity and advanced techniques are more often used including complex procedures such as the present case of a left lower lobe (LLL) sleeve lobectomy. AimsThe aim was to show how RATS can be considered as an alternative approach when facing lung tumors in challenging locations such as the present case of a left lower lobe sleeve lobectomy. MethodsWe present the case of a 57-year-old male smoker (30 pack-years) diagnosed with a carcinoid tumor in the left lower lobe (UICC-Stage IA2) via bronchoscopy. A FDG-PET/CT scan confirmed a proximal endobronchial lesion at the level of the carina between the upper and lower lobe measuring 11mm, with no other metabolically active lesions. Pulmonary function tests showed FEV1 of 3.21L (87) and DLCO of 8.0 mmol/kPa/min (81%). Based on these findings and the challenging location of the tumor, a robot-assisted sleeve resection of the lower left lobe and mediastinal lymph node dissection was performed. ResultsThe postoperative course was uncomplicated. The patient received intravenous antibiotics (Co-Amoxicillin) for 72 hours. A bronchoscopy performed 3 days post-surgery showed excellent anastomotic healings and the patient could be discharged on the 4th postoperative day. Histopathological examination revealed a complete and R0 resection of the tumor with tumor-free lymph nodes. ConclusionRobot-assisted thoracic surgery offers promising outcomes, with a smooth postoperative course and early recovery. This case highlights the feasibility and effectiveness of RATS in managing lung carcinoid tumors located at anatomically challenging sites, such as the carina between the upper and the lower lobe bronchi. The robotic approach allowed for precise resection and reconstruction, effectively avoiding the need for open surgery. |






