Friday, 23. May 2025
|
07:30 – 08:00
|
Registration & Exhibition OpeningStart your day with inspiring conversations! The exhibition opens its doors – explore, connect, and enjoy what our sponsors have to offer. |
|
|
Break
|
||
|
08:00 – 09:30
Room 5B
|
AI – what is in the pipeline for practitioners in...? what’s the timeline?
Antonio Nocito, Baden; Ralph Peterli, Basel
|
|
|
Main Session
|
||
|
08:00–08:18
Decision making
Joël Lavanchy, Basel
|
||
|
08:18–08:36
Documentation
Alice Gilson, Geneva / Genève
|
||
|
08:36–08:54
Administration (Rehab etc.)
Olga Endrich, Bern
|
||
|
08:54–09:12
Paper writing
Marcel-André Schneider, Zurich
|
||
|
09:12–09:30
Legal issues
Iris Herzog-Zwitter, Weinfelden
|
||
|
08:00 – 09:30
Room 5C
|
Colorectal I
Matthias Turina, Zurich; Martin Hübner, Lausanne
|
|
|
Free Communication
|
||
|
08:00–08:07
Global Benchmarks for Minimal-Invasive Right Hemicolectomy in Adenocarcinoma
Fariba Abbassi, Zurich
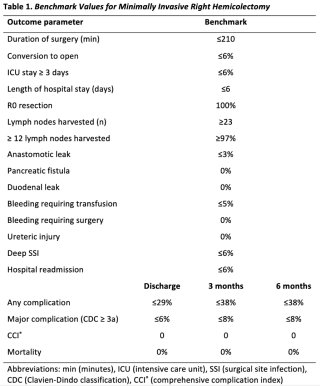
AbstractBackgroundOncologic right hemicolectomy (rHC) remains the only curative treatment for right-sided colon cancer. Despite its increasing complexity, this procedure is not centralized in many countries, underscoring the need for rigorous assessment and continuous improvement in surgical quality. Benchmarking is a validated quality improvement tool. By defining best achievable outcomes as reference (i.e. benchmarks), it enables centers to evaluate their performance and identify weaknesses or areas for improvement. AimsThis analysis aimed to establish benchmarks for outcome parameters in minimal-invasive rHC. MethodsWe analyzed data from consecutive patients with adenocarcinoma of the colon who underwent minimal-invasive rHC between July 2017 and June 2022 at 19 expert centers across five continents. Ideal cases were defined as elective surgeries for cT1-T3 tumors without distant metastases, major comorbidities, or significant prior abdominal surgeries. Benchmarks were derived for 19 clinically relevant surgical outcomes, including perioperative and oncological parameters, procedure-specific complications, overall morbidity, and mortality. Benchmarks were set at the 75th percentile for negative outcomes and the 25th percentile for positive outcomes across all centers’ medians. ResultsAmong 3154 patients, 686 (22%) qualified as ideal. The proportion of ideal cases varied widely across centers (range: 2 – 51%) (Figure 1). Key benchmarks at 3 months were overall morbidity ≤38%, major (Clavien-Dindo ≥3a) complications ≤8%, and 0% mortality. Procedure-specific benchmarks were anastomotic leak ≤3%, and deep surgical site infections ≤6%. Finally, oncologic benchmarks included R0 resection rates 100% and ≥12 lymph nodes harvested ≥96.9% (Table 1). Ideal compared to non-ideal patients and centers performing ≥500 cases compared to <500 cases annually demonstrated superior outcomes. ConclusionThis study demonstrates that, despite its complexity, minimally invasive rHC can be performed with low morbidity and high oncological accuracy. The established benchmarks provide a reference for centers striving to achieve excellence in this procedure. 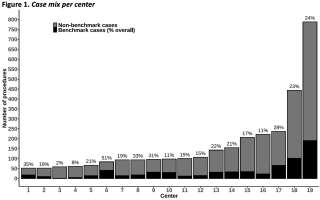
|
||
|
08:10–08:17
Development and Validation of Predictive Models for Anastomotic Leakage in TaTME Rectal Surgery
Alexis Litchinko, Fribourg
AbstractBackgroundAnastomotic insufficiency remains a devastating complication in colorectal surgery. AimsThis study sought to develop a statistical model to predict the occurence of anastomotic insufficiency and support preoperative planning, helping to mitigate risks. MethodsData from the international prospective TaTME registry were analyzed. Random Forest and logistic regression models were developed to estimate the probability of anastomotic insufficiency, taking into account demographics and clinical variables. ResultsA total of 2,262 patients from the registry were analysed and split in a training and test datased. Significant predictors identified by the models included BMI, age, tumor height, and hospital. The Random Forest model emphasized weight as a significant variable, while the logistic regression model highlighted gender as an important predictor. In both models, tumor height and hospital were independent predictors of anastomotic insufficiency. Logistic regression emerged as the superior model, exhibiting a higher predictive accuracy of 65% when compared to Random Forest. ConclusionThis study successfully identified several critical preoperative risk factors for anastomotic insufficiency in colorectal surgery, including BMI, age, tumor height, and hospital-specific variability. The logistic regression model demonstrated better predictive power, making it a valuable tool for assisting surgeons in preoperative risk assessment. |
||
|
08:20–08:27
Clinical, Sociodemographic, and Treatment Characteristics of Early-Onset Versus Late-Onset Colorectal Cancer: Final Results of a Multicenter Observational Study
Hélène Gros, Basel / San Diego
AbstractBackgroundEarly-onset colorectal cancer (EOCC), defined as colorectal cancer (CRC) ≤ 50 years, has seen an alarming rising incidence in Western countries. AimsThis study aims to analyze clinical, socio-economic, and oncological treatment differences between EOCC patients and those with later-onset colorectal cancer (LOCC). MethodsThis multicenter observational cohort study included CRC patients treated from 01/01/2023 to 30/06/2024 across 11 centers in Northwestern Switzerland. Data was collected through questionnaires and patient charts ResultsWe included 764 patients, thereof 58.9% male. Mean age was 42.1 for EOCC (n=80) and 70.8 years for LOCC (n=684). EOCC were more frequently non-Swiss (67.5% vs. 32.2%, p<0.001), reported greater financial hardship (p<0.001), had higher glucose consumption (>5 units/week) (48.8% vs. 35.2%, p=0.02), and more often had second-degree relatives with CRC (p=0.05). Childhood radiation exposure was higher in LOCC versus EOCC (94.6% vs. 88.8%, p=0.05). Most common EOCC symptoms were abdominal pain (54.6%) and rectal bleeding (50.6%) versus rectal bleeding (35.4%) and changes in bowel habits (25.3%) in LOCC. EOCC experienced longer time to diagnosis (7.2 vs. 4.2 months, p=0.03). At the 75th percentile, EOCC reached a higher UICC stage (IIIC) compared to LOCC (IIIA). Adjuvant therapy was more common in EOCC with colon cancer (52.4% vs. 35.2%, p=0.04) and rectal cancer (58.3% vs. 33.3%, p=0.02) than in LOCC. Defunctioning ostomies were more frequent in EOCC than LOCC colon cancer patients (13.2% vs. 3.2%, p=0.01), with no difference in rectal cancer patients (p>0.99). Overall, EOCC had shorter hospital stays (8.66 vs. 11.43 days, p=0.05), while ICU stays, retrieved lymph nodes, and operation time were comparable. ConclusionEOCC patients experienced diagnostic delays, more advanced disease at presentation, and notable socioeconomic and lifestyle disparities. These findings highlight the need for risk-adjusted screening programs and personalized diagnostic strategies to enable earlier detection and improved outcomes for individuals under 50. |
||
|
08:30–08:37
ChatGPT for therapy conception of colorectal cancer: Can artificial intelligence complement a traditional tumor board?
Dimitrios Chatziisaak, St.Gallen / St. Gallen, Lausanne / Lausanne, St. Gallen
AbstractBackgroundAlthough multidisciplinary tumor boards (MDT) represent the gold standard for decision-making in cancer treatment, they require significant resources and may be susceptible to human bias. Artificial intelligence (AI), particularly large language models such as ChatGPT, has the potential to enhance or optimize the decision-making processes. The present study examines the potential for integrating AI into clinical practice by comparing MDT decisions with those generated by ChatGPT. AimsThe aim of this study is to evaluate the concordance between the therapeutic recommendations proposed by a MDT and those generated by a large language model (ChatGPT) for colorectal cancer. MethodsA retrospective, monocentric comparative study was conducted involving consecutive patients with newly diagnosed colorectal cancer discussed at our MDT. The pre-therapeutic and post-therapeutic MDT recommendations were compared with those of ChatGPT-4 in respect of concordance. ResultsIn the pre-therapeutic discussions, complete concordance was observed in 72.5% cases, with partial concordance in 10.2% and discordance in 17.3%. For post-therapeutic discussions, the concordance increased to 82.8%. 11.8% of decisions displayed partial concordance, and 5.4% demonstrated discordance. It is noteworthy that discordance was more frequent in patients > 77 years and with ASA ≥ III. ConclusionThere is a substantial concordance between the recommendations generated by ChatGPT and those provided by traditional MDT, indicating the potential utility of AI in supporting clinical decision-making for colorectal cancer management. |
||
|
08:40–08:47
Does Papillon contact x-ray radiotherapy allows organ preservation in rectal cancer: results from a Swiss cohort
Frédéric Ris, Geneva
AbstractBackgroundMultimodal treatment of rectal cancer involves a combination of radiotherapy (RT), chemotherapy, and surgery. There has beena an increasing interest in organ preservation strategies. Response strongly correlates with RT dose, but dose escalation with external beam remains limited. Papillon is an endocavitary Radiotherapy device,which delivers low energy X-rays, allowing for safe dose escalation and better complete response rate directly at the tumour location. AimsThis study reports on the use of Papillon in a swiss cohort MethodsRetrospective study on a prospective database of all patient treated between January 2015 and end of 2024. Inclusion criteria: small tumors (< than 3 cm), for larger tumors after a standard CRT and a median interval of 3 weeks Application of the boost according to the OPERA trial protocol Assessment at 6 weeks after the end of the Papillon , at 3 months and every 3-month interval for the first 2 years and every 6 months thereafter. Kaplan Meier for local relapse and TME-free survival. Local relapse was defined as any visible tumor on rectoscopy and or MRI and confirmed by histology after achieving complete response. TME-free survival was defined as the organ preservation at 12 month ResultsBetween January 2015 and end 2024, 24 rectal cancer patients were treated with the addition of a boost delivered by Papillon to standard RT, with or without chemotherapy, in an upfront organ preservation strategy. After a median follow-up (FU) of ConclusionOur results demonstrate that the addition of Papillon contact RT provides a high rate of local remission with sustained long-term organ preservation, offering a promising alternative to traditional surgical approaches in patients with rectal cancer |
||
|
08:50–08:57
Prevalence of genetic alterations in patients with early-onset colorectal cancer
Benjamin Wiesler, Basel
AbstractBackgroundThe number of patients diagnosed with colorectal cancer under the age of 50 is increasing. The aetiology of early-onset CRC remains incompletely elucidated, with uncertainty surrounding potential contributory factors such as the prevalence of genetic alterations. AimsThe objective of this study was to compare the prevalence of genetic alterations that are associated with CRC in early-onset colorectal cancer (EOCC) with late-onset colorectal cancer (LOCC). MethodsThe molecular profiles of patients diagnosed with locally advanced or metastatatic CRC between 2015 and 2023 in two large pathology departments were analyzed using targeted next-generation sequencing. ResultsA total of 769 patients were included in this retrospective study (70 patients in the EOCC group and 699 in the LOCC group). The male:female ratio of patients was 59.7:40.3, with 27.4% (n=144) of patients diagnosed with UICC Stage III and 51.33% (n=270) with Stage IV disease. In the EOCC group, 67.7% (n=46) of patients had a KRAS mutation compared to 68.1% (n=469) in the LOCC group (p=1.0). The percentage of patients with a BRAF mutation in the EOCC group was 84.1% (n=58) compared to 86.5% (n=602) in the LOCC group (p=0.58). NRAS mutations were detected in 97.1% (n=66) of EOCC patients and 96.7% (n=666) of LOCC patients (p=1.0). TP53 mutations were found in 53.1% (n=26) of EOCC patients and 55.5% (n=257) of LOCC patients (p=0.76), while SMAD4 mutations were found in 6.12% (n=3) of EOCC patients and 10.6% (n=49) of LOCC patients (p=0.46). There was no difference in the presence of microsatellite instability between the two groups. ConclusionNo significant differences were observed for the commonly known mutations in this medium-sized cohort of advanced CRC. Future molecular studies of EOCC might rather focus on epigenetic factors than particular mutational patterns. |
||
|
09:00–09:07
Lymph Node Ratio Added to N-Stage Improves Risk Stratification in Colorectal Cancer
Francesca Cordera, Liestal
AbstractBackgroundLymph node metastases (LNM) have an important prognostic value in colorectal cancer (CRC) and staging intends to determine adjuvant treatment. Lymph node ratio, defined as the proportion of positive lymph nodes compared to the total amount of resected lymph nodes, seems to have an important prognostic impact while taking the quality of lymphadenectomy and number of resected lymph nodes into account compared to the conventional N-stage. Previous studies could demonstrate better prognostic predication of LNR compared to conventional N-stage. AimsWe aimed to evaluate the prognostic impact of LNR on the outcome of patients with CRC. MethodsThis is a unicentre retrospective cohort study. We included all patients undergoing surgical resection for colorectal cancer between 2014 and 2022 in a specialised centre in Switzerland. We used predefined LNRs from previous publications in CRC. Survival rates according to N-stage and LNRs were analysed using uni- and multivariate Cox regression. Results493 patients were included. The median number of resected lymph nodes was 28. 5-year overall survival (OS) was 94% in N0-stage (n=301/493). Patients with LNMs (n=192/493) had decreasing 5-year overall survival (72% with pN1 and 52% in pN2). LNR showed decreasing 5-year OS with increasing LNR (50% in LNR2, 36% in LNR3 and 30% in LNR4, p < 0.001). Additionally, disease free survival (DFS) showed the same dynamic with 50% 5-year DFS in LNR2-3 and 33% in LNR 4 (p = 0.002). While most of the N1-stage patients showed LNR1, 4/122 (3%) had LNR2-3 and therefore a poorer prognosis. ConclusionThe predefined LNRs should be standardly used for risk stratification in CRC as they add to the prognostic value of the conventional N-stage. LNR allows to predict 5 year OS and DFS more precisely than conventional N-stage. |
||
|
09:10–09:17
Preoperative Vascular Mapping for Complete Mesocolic Excision During Right Colectomy; a Single Center Feasibility Study
Evangelos Kalogiannis, Nyon / Fribourg
AbstractBackgroundColorectal cancer (CRC) affects 4.5% of the general population, with 15% involving the right colon. Surgery, when feasible, varies from conventional right colectomy to Complete Mesocolic Excision (CME). Although better oncological outcomes were reported in the literature after CME, there is an acknowledged higher risk of operative vascular lesions. Various approaches have been proposed to facilitate CME, such as the “open book” model and 3D modelling of the mesenteric vessels, however CME remains technically challenging. AimsOur study aims to analyze whether preoperative CT imaging with vascular mapping (PVM) of the superior mesenteric vessels could offer guidance on the vascular anatomy during CME. MethodsThis prospective, monocentric study aims to include 30 patients undergoing CME for right CRC. Preoperatively, a biphasic CT scan with 3-D vascular reconstruction of the superior mesenteric vessels is performed. Vascular distances are calculated based on CT, then compared to intraoperative documentation of the mesenteric vessels (Figure 1). Primary outcomes are the surgeons’ evaluation of the benefit of vascular mapping and the statistical correlation of the vascular distances between CT guidance and operative finding. ResultsTo this day, 22 patients have been included. Surgeons found the preoperative vascular mapping very useful (3.58/5 on a Likert scale). Mean operation time was 263 minutes, with a mean of 36 lymph nodes harvested and no vascular lesions. Postoperative ileus occurred in 27% (6/22), Clavien-Dindo complications III-V in 13,6% (3/22) with one anastomotic leak (4,5%) and one death after discharge at home of unknown cause. Statistical analysis of the vascular distances will be performed upon completion of the study. ConclusionOur preliminary data suggest that PVM may be a valuable tool for reducing the risks associated with CME and aiding vascular ligation in this complex surgical technique. Further studies are required to asses PVM utility in CME and confirm these outcomes. 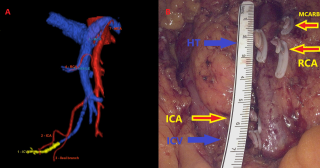
|
||
|
09:20–09:27
Fluorescence Indocyanine Green (ICG) for Sentinel-Lymph-Node Mapping in Colorectal Cancer: a Systematic Review
Alexis Litchinko, Fribourg
AbstractBackgroundModern surgical guidance in oncologic colerectal resections can be enhanced by visualizing lymphatic flow during surgery, informing the extent of lymphadenectomy and the precise extent of digestive resection. Indeed, lymphadenectomy is mandatory in a curative procedure. AimsThe objective of the present work is to review the practice and impact of indocyanine green fluorescence imaging for real-time identification of lymphatic flow and especially sentinel nodes in patients undergoing elective surgery for colorectal cancer. MethodsA systematic review was conducted to identify relevant studies on sentinel node mapping using indocyanine green (ICG) in colorectal cancer surgery. A comprehensive search was performed in electronic databases including PubMed, Embase, and Cochrane Library from inception to December 2024. The search strategy incorporated relevant keywords and MeSH terms, combining variations of "colorectal neoplasms," "sentinel lymph node," "indocyanine green," and related terms. The search was limited to articles published in English language. ResultsA total of 337 relevant studies were identified and screened. Among them, 45 studies were considered for eligibility, and 12 were ultimately included in the systematic review. ICG-FI has not yet demonstrated superiority over the standard blue dye technique. Moreover, a notable heterogeneity existed among the reported studies concerning ICG dosage, injection methods, and the definition of positive LN status, making direct comparisons challenging. ConclusionDespite the potential demonstrated in other oncological resections, ICG-FI requires further investigation and standardization, both in protocols and indications to fully harness its capabilities for SLN detection in CRC. This is particularly important for the reliable detection of metastatic lymphnodes. Larger patient populations should be considered in future research to comprehensively assess the efficacy of ICG-FI. This systematic review serves as a valuable resource for researchers and clinicians interested in utilizing ICG-FI for SLN detection in colorectal cancer, yet it also highlights the need for further standardization in this area of study. |
||
|
08:00 – 09:30
Room 1B
|
Global Surgery
Peter Nussbaumer, Niederurnen; Martin Walliser, Glarus
|
|
|
Main Session
|
||
|
08:00–08:18
We look at the same moon but live in different worlds - pediatric burn care in Afghanistan
Clemens Maria Schiestl, Zurich
|
||
|
08:22–08:40
Gallbladders, Condoms and Sheep Stew – Swiss Medical Teams in Tajikistan
Nicole van Veelen, Lucerne
|
||
|
08:44–09:02
Global Surgery fellowship: the what, the why and for whom
Kee B. Park, Boston US
|
||
|
09:06–09:24
Humanitarian Medical Missions: A Young Surgeons View on Expectations and Reality
Aatharshan Kannathasan, Zug
|
||
|
08:00 – 09:30
Room 4BC
|
Hernia
Andrea Donadini, Lugano; Lukas Widmer, Fribourg
|
|
|
Free Communication
|
||
|
08:00–08:07
Robotic versus conventional minimally invasive inguinal hernia repair: the blinded randomized controlled ROGER trial
Julian Süsstrunk, Basel
AbstractBackgroundIt remains uncertain whether robotic inguinal hernia repair offers advantages over conventional minimally invasive techniques. AimsTo evaluate postoperative pain following robotic transabdominal preperitoneal repair (rTAPP) compared to conventional totally extraperitoneal repair (TEP). MethodsProspective, blinded, 2-group, randomized single-center trial conducted at a tertiary healthcare institution in Switzerland including 182 patients with uni- or bilateral inguinal hernias. Patients were 1:1 randomized to undergo rTAPP or TEP with postoperative pain on a numeric rating scale (NRS 0 - 10) while coughing 24 hours postoperative as the primary outcome. Secondary endpoints included the assessment of multiple pain and quality of life questionnaires, intra- and postoperative complications, procedure time and the surgeon’s workload, measured using the NASA task-load-index. Results91 patients (94.4% male, mean age 55.1 +/- 14.5 years, mean BMI 24.6 +/- 2.9 kg/m2, 21.1% bilateral hernias; p = n/s) were randomized to undergo rTAPP and 91 patients (93.4% male, mean age 56.8 +/- 15.2 years, mean BMI 24.8 +/- 3 kg/m2, 22% bilateral hernias) to TEP respectively. Postoperative pain 24 hours after surgery while coughing was 4.52 +/- 2.6 after rTAPP and 4.73 +/- 2.55 after TEP (p = 0.56). 30-days postoperative comprehensive complication index was 1.37 in rTAPP and 1.63 in TEP (p = 0.99). Procedure time for unilateral repair was 79 +/- 15.2 minutes in rTAPP and 64 +/- 15.2 minutes in TEP (p < 0.001). Overall surgeon’s workload was lower in rTAPP compared to TEP (Pillai's Trace = 0.45, F(6, 174) = 12.34, p < .001) ConclusionrTAPP and TEP result in comparable postoperative pain, length of stay and complication rates. Surgeons' workload was lower in rTAPP at the cost of a longer operative time. Recurrence rates and cost analysis will be reported 1 year after. |
||
|
08:08–08:15
Ventral Incisional Hernia Repair With Synthetic Versus Biosynthetic Mesh; Retrospective Comparative Analysis From a Tertiary Reference Center.
Noémie Simonetta, Nyon / Lausanne
AbstractBackgroundAlthough biosynthetic mesh is being increasingly used to treat ventral incisional hernias (vIH), there is a paucity of data derived from non-industry-sponsored studies. AimsAim of the present study was to compare i) postoperative Surgical Site Occurrences (SSO) and ii) viH recurrence in patients operated with non-absorbable synthetic versus slowly absorbable biosynthetic mesh. MethodsAdult patients who had vIH repair surgery in our tertiary referral hospital between 01.01.2017 and 31.12.2023 were retrospectively assessed. Demographics and surgical outcomes were compared between patients with synthetic (S) versus biosynthetic (BS) vIH mesh repair. SSO were defined as surgical site seroma, infection or hematoma. Standard univariable and multivariable logistic analysis were performed, with significance threshold at p<0.05. ResultsOverall, 95 patients were included in the present study (57.9% males, mean age 63±14years); 56 (58.9%) patients were in the S and n=39 (41.1%) in the BS group. No differences in baseline characteristics or comorbidities were observed. SSO were documented in 48.2% S versus 43.6% BS patients (p=0.657), but seroma rates were increased in S patients (25% versus 5.1% BS, p=0.011). Mesh type was not associated with SSO in multivariable analysis (aOR 0.67, 95%CI 0.23-1.94). Overall 90-day morbidity was comparable, although BS patients had higher readmission rates (17.9% vs 3.6% S, p=0.019). vIH recurrence was observed in 5.4% S vs 7.7% BS patients (p=0.687), with similar mean recurrence intervals (456d S versus 625d BS, p=0.100). ConclusionIn the present study, vIH repair with a slowly absorbable biosynthetic mesh was associated with similar overall SSO and hernia recurrence rates as a non-absorbable synthetic mesh. |
||
|
08:16–08:23
Prophylactic mesh reinforcement after open aortic aneurysm repair: a retrospective study
Melissa Lagger, Fribourg / Villars-sur-Glane
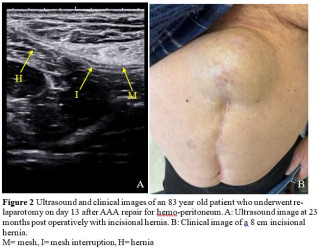
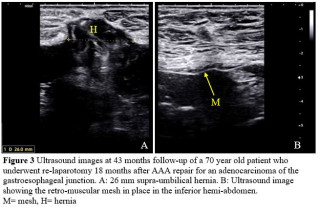
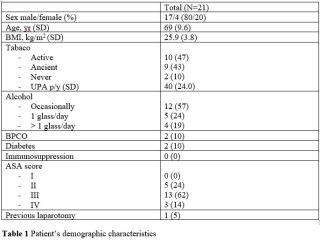
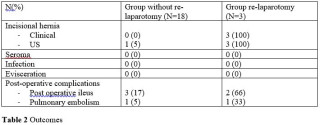
AbstractBackgroundPatients who undergo open abdominal aortic aneurysm (AAA) repair via a midline laparotomy face a 3-fold increased risk of developing an incisional hernia (IH) postoperatively. Recent guidelines in vascular surgery strongly recommend prophylactic mesh reinforcement (PMR) during abdominal wall closure for AAA to reduce the incidence of incisional hernias (IH). AimsThis study aims to evaluate the effectiveness of retromuscular PMR in reducing the incidence of IH after AAA repair, as well as to assess secondary postoperative complications. MethodsThis retrospective study includes patients who underwent elective AAA repair with PMR in our institution between 2019 and 2024. Patients' demographics, operative details and postoperative complications were collected from patient’s records. Follow-up consisted in clinical examinations at least one year post-surgery, abdominal ultrasounds (Figure 1, 2 and 3) and EQ-5D-5L questionnaires. The primary outcome was the incidence of IH, secondary outcomes included the incidence of fascial dehiscence, seromas and surgical site infections. Descriptive statistics were used to evaluate both the primary and secondary endpoints. ResultsTwenty-one patients were included. The median follow-up period was 32 months. The overall incidence of IH was 19% (4 cases): three hernias occurred in patients who had been re-operated with incision and closure of the mesh; the fourth was identified through ultrasound examination without any clinical correlation. Re-laparotomy seemed to be a relevant risk factor for hernia development, but the sample size and study configuration limited our ability to confirm a significant association. None of patients developed fascial dehiscence, seromas or surgical site infections (Table 1 and 2). Quality of life was reported to be largely preserved, with most experiencing little to no functional impairment and an average general health score of 80%. ConclusionThis study provides clinical evidence supporting the application of recent guidelines in vascular surgery regarding the use of retromuscular PMR. Registration number: Observational study NCT06762561 (https://www.clinicaltrials.gov) 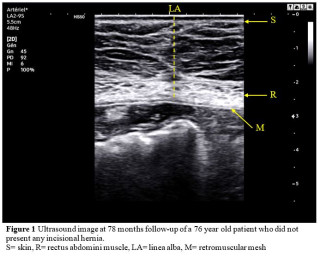
|
||
|
PSGVC88
08:24–08:31
The Lumbar Hernia
Karolin Dallago, chur
AbstractBackgroundThe Lumbar Hernia is a rare entity, there are about 300 cases described in the literature. It seems to be a once in a lifetime opportunity for a surgeon to treat a lumbar hernia. The defect lays in the lumbar muscles below the 12th rib and above the iliac crest There are two types described, the superior lumbar hernia (Grynfeltt-Lesshafthernia) which is more common and the inferior lumbar hernia (Petit hernia) Case presentationA 71 year old lady presented with a pain and swelling in the right lumbal aerea for several months. The MRI which was ordered by her family doctor showed the clear immage of a superior lumbar hernia. We indicated an endocopic reapair for this hernia, which can be done laparoscopically (intraperitoneal IPOM or extreperitoneal TAPP, TEP) or retroperitoneally TEP repair (rTEP). We chose the rTEP, which is very well described in the articel by B.Li et al. "Retroperitoneal totally endoscopic prosthetic repair of a primary lumbar hernia" from 2020. (Videopresentation) No postoperative complications occurred. ConclusionVarious surgical repair strategies have been recorded for the treatment of the umbar hernia, but there seems to be no currently unified standard. In our patient RTEP could be performed safe and effective. A simple non coated polypropylene mesh can be used. |
||
|
08:32–08:39
Outcomes of Outpatient Hernia Surgery at a Tertiary Referral Center: Results of a Standardized Pathway
Enrique Lázaro-Fontanet, Lausanne
AbstractBackgroundOutpatient hernia surgery is increasingly practiced, in a global effort to optimize patient comfort and outcomes, as well as healthcare costs. Standardized patient selection criteria and postoperative pathway are key to limit the risk of unplanned hospital admissions after surgery. AimsThe aim of the current study was to assess the outcomes of our institutional standardized outpatient hernia surgery program and identify factors potentially contributing to outpatient management failure (OMF). MethodsAll adult patients undergoing outpatient hernia repair in our tertiary referral center between 06.2013, and 12.2019 were retrospectively assessed. Primary endpoint was the rate of OMF, defined as unplanned hospital admissions and/or consultations for poor pain management. Demographic and surgical characteristics were compared to identify factors associated with OMF. The χ² test or Fisher’s exact test were used for categorical and Student’s t-test for continuous variables, with a significance threshold sat p < 0.05. ResultsOverall, 405 patients were included in the present study. Mean age was 50 years (SD 15), and 85% (n=345) were male. Outpatient management failure (OMF) was observed in 3% (n=12) of all patients. Among demographic parameters, only ASA class was significantly higher in OMF patients (ASA 2-3 in 75% OMF versus 40% non-OMF patients, p=0.039). Bilateral inguinal hernia repair was performed in 41.7%OMS versus 10.4% non-OMF patients, p=0.009), whereas mean operative duration was longer in OMF patients (43.1 min versus 65.8min, p=0.019). Postoperative complications were observed in 5.7% in the whole cohort (50% in OMF versus 4.3% non-OMF patients, p<0.001). Persistent postoperative pain was also more frequent in OMF patients, in 1 week (p=0.033), 1 month (p=0.003) and 3 months (0=0.009) after surgery. ConclusionThe implementation of a standardized pathway has achieved favorable outcomes in outpatient hernia surgery, with a low overall OMF rate of 3%. Patient- and procedure- related characteristics need careful assessment to optimize patient selection. |
||
|
08:40–08:47
Multisite hernia treatment: The robotic approach makes it feasible
Eva Diaz Casanova, Bellinzona
AbstractBackgroundThe use of robotic surgery for combined abdominal wall hernias, including multiquadrant hernias, is underexplored in the literature. While the prevalence of simultaneous hernias is not well documented, they represent a frequent clinical challenge. AimsThis study aimed to evaluate the feasibility of a robotic approach for treating simultaneous umbilical, incisional, and inguinal hernias. MethodsWe retrospectively reviewed a prospectively maintained dataset of abdominal wall hernias to identify patients treated for combined hernias. Patients were divided into two groups based on the robotic docking technique, and the data were analyzed. ResultsFrom January 2020 to December 2024, 30 patients underwent robotic combined hernia repair. 90% were male, with a mean age of 63.2 (49.8–76.6) years. Single docking was feasible for 30% patients with W1 median hernias with mean diameter of 2.8cm (1.4–4.2) combined with an unilateral inguinal hernia. Double docking was necessary for 70% of patients with wider (W1-3) median hernia defect, mean diameter of 4.0cm (1.2-6.8) or bilateral inguinal hernias. No intraoperative complications were reported. The mean operative time was 148.0 minutes (111.0–185.1) for the single docking and 230.7 minutes (152.1–309.3) for the double docking and the mean hospital stay was 2.1 days (1.5–2.7) for the single docking and 3.4 days (0.5–6.2) for the double docking. The morbidity rate was 11.1% for the single docking and 23.8% for the double docking, only with one reintervention was needed in the double docking. Most of the complications in both groups were surgical site occurrences, managed conservatively. At a mean follow-up of 19.2 months (4.2–34.2), no recurrences were observed. ConclusionRobotic multisite hernia repair is a safe and effective minimally invasive option. Single docking offers advantages but is limited to patients with median defects and unilateral inguinal hernias. For median defects combined with bilateral inguinal hernias, double docking is generally required. |
||
|
08:48–08:55
Evaluating the Learning Curve of Dexter-Assisted rTAPP: Feasibility, Safety, and Early Outcomes at a High-Volume Hernia Center
Marc Salm, Baden
AbstractBackgroundRobotic-assisted surgery has been associated with enhanced precision and the potential to reduce postoperative complications in preperitoneal inguinal hernia repair. The novel Swiss robotic platform Dexter, designed as an open and adaptable system, integrates into conventional laparoscopic setups. It was introduced at our high-volume hernia center, where total extraperitoneal hernia repair (TEP) previously served as the standard of care. AimsThis study aims to evaluate the clinical outcomes and feasibility of robotic transabdominal preperitoneal hernia repair (rTAPP) using the Dexter platform during the initial learning curve at a Cantonal Hospital in Switzerland. MethodsFrom February to December 2024, consecutive patients undergoing Dexter-assisted rTAPP were prospectively enrolled in a database. Postoperative outcomes, including prolonged pain, were assessed during follow-up visits 6–8 weeks after surgery. Importantly, none of the participating surgeons had prior routine experience with robotic surgical platforms before Dexter's implementation. ResultsA total of 66 patients (82% male, median age 61 years, IQR 54–71) underwent rTAPP, with 91% presenting bilateral hernias and 6 cases involving recurrences. The median operative times for bilateral and unilateral hernias were 108 minutes (IQR 93–140) and 90 minutes (IQR 79–109), respectively. Major postoperative complications (Clavien-Dindo grade ≥3) occurred in two patients (3%), both requiring relaparoscopy—one for pain out of proportion on postoperative day 1 and one for foreign body retrieval. Follow-up data were available for 39 patients (70%). Among these, 83% reported no pain, 14% reported mild pain, and 3% reported moderate pain. There were no hernia recurrences observed during the follow-up period. ConclusionDexter-assisted rTAPP can be safely implemented during the learning curve, demonstrating acceptable safety and feasibility. However, the learning curve is associated with prolonged operative times. Further studies with expanded robotic experience and longer follow-up are required to assess potential benefits, particularly in reducing chronic pain. |
||
|
08:56–09:03
Comparative Analysis of Robotic versus Laparoscopic Surgery
Claudio Canal, Frauenfeld
AbstractBackgroundMinimally invasive surgery reduces recovery times and complications compared to open procedures. While laparoscopic surgery (LS) is widely used, robotic-assisted techniques (RS) like the DaVinci system are gaining recognition for enhanced precision and potential improvements in patient outcomes. AimsThe aim of this project was to evaluate and compare the differences between RS and conventional LS across various surgical procedures. MethodsPatients undergoing RS for transabdominal preperitoneal hernia repair (TAPP), right hemicolectomy, rectal resection, rectopexy and hiatus hernia repair between January 2019 and December 2022 were included. In addition, patients undergoing LS for the same procedures during this time frame were also included. Patient demographics, operative time, length of hospital stay, complications, costs, and remuneration were analysed retrospectively. ResultsOverall, 88 patients were included. The 46 RS patients were younger than the 42 LS patients (62 vs. 69 years) but both groups had a similar distribution with regards to sex, weight, and Charlson Comorbidity Index. RS had a significantly longer operative time (162 ± 84 minutes) compared to the LS group (127 ± 67 minutes, p=0.036). However, the RS patients had a shorter length of hospital stay (5.5 ± 4.5 days vs. 8.1 ± 7.1 days, p=0.038). There was no difference regarding complication rates (22% vs 19%, p=0.098). Costs were not different between RS and LS (24367 vs. 23963 CHF, p=0.916). However, LS had a higher earning-cost balance (RS -2034 vs. LS 6319 CHF, p=0.002). ConclusionRS compared to LS is associated with a longer operative time, but a shorter hospital stay and comparable complication rates. Overall, however, LS seems to be more rewarding than RS. |
||
|
09:04–09:11
Laparoscopic Enhanced View Totally Extraperitoneal Rives-Stoppa Repair (eTEP-RS) for Ventral Hernia: No Robot, No Problem!
Lukas Gantner, Zurich / Zürich
AbstractBackgroundThe eTEP-RS technique has become a versatile approach for ventral hernia repair, offering a minimally invasive option while avoiding the risks of intraperitoneal mesh placement. Despite the growing popularity of robotic platforms for this procedure, many Swiss hospitals face limited access to such systems. AimsThis video aims to demonstrate a laparoscopic eTEP-RS repair, emphasizing technical aspects and key anatomical landmarks. The objective is to provide a practical guide for surgeons with limited access to robotic systems who wish to expand their repertoire with a minimally invasive sublay technique. MethodsThe video includes high-quality intraoperative footage of a laparoscopic eTEP-RS repair. Step-by-step instructions are provided, focusing on trocar placement, dissection techniques, and achieving optimal visualization of the retromuscular space. The procedure demonstrates the feasibility of using standard laparoscopic instruments to accomplish a tension-free mesh placement. ResultsThe video illustrates the key steps of a laparoscopic eTEP-RS technique:
ConclusionThe laparoscopic eTEP-RS technique provides an excellent alternative to open and robotic sublay repairs, enabling the placement of a large mesh in line with current guidelines. This video highlights the feasibility of performing eTEP-RS laparoscopically, making the technique accessible to surgeons in hospitals with limited robotic resources. |
||
|
09:12–09:19
Steps in eTEPs: What can possibly go wrong?
Isabelle Obrecht, Basel
AbstractBackgroundEnhanced-view total extraperitoneal plasty (eTEP) is a promising minimally-invasive technique for ventral hernia repair, allowing extensive retromuscular dissection and large mesh placement with low rates of wound complications and fast recovery. The learning curve, however, is flat and technical expertise is crucial for good outcomes. AimsThe aim of this study is to analyze the difficulty and occurence of adverse events of 10 crucial steps in the eTEP procedure for ventral hernia repair. This may provide guidance for a safe introduction of eTEP for surgeons new to this technique. MethodsAll patients undergoing eTEP for primary or incisional ventral hernias between October 2023 and December 2024 at three centres were included in this prospective study. 10 crucial surgical steps were defined and each step was rated for its difficulty (0 – 5 points on a numeric rating scale) and analyzed for incidence of adverse events. Surgeon workload was measured using the NASA-Task-Load-Index. ResultsA total of 118 patients underwent eTEP. Suture of the hernia defect was rated the most difficult step (2.49/5), followed by dissection of the hernia defect (2.45/5) and closure of posterior defects (2.19/5). Common adverse events were pneumoperitoneum during dissection of the hernial sac (50.9%) and minor bleeding during dissection of the retromuscular plane (46.6%). A less common but more severe adverse event was injury to the linea alba in 5 cases during cross-over. Mean operation time was 97 minutes, median length of stay was 2 days. Operative revisions were necessary in 3.4%. Mean mental and physical workload according to NASA-Task-Load-Index was 44 / 100 and 45 / 100 respectively. ConclusioneTEP is a technically challenging procedure with a relatively high surgeon workload, mainly due to suturing and hernia dissection. Detailed knowledge about possible adverse events and their frequency during the procedure is a helpful guide for mastering this technique. |
||
|
09:20–09:27
Abdominal Wall Reconstruction: The Role of the Plastic Surgeon
Radu Olariu, Bern
DetailsBackgroundAbdominal wall reconstruction (AWR) is a complex challenge requiring expertise in plastic surgery to restore both structural integrity and function. While general / visceral surgeons primarily address hernia repair, plastic surgeons play a critical role in soft-tissue management, functional restoration, and complex defect reconstruction using advanced flap techniques. Innovations in locoregional and free tissue transfer have expanded reconstructive options, improving outcomes in cases of extensive tissue loss, infection, or prior surgical failure. AimsThis study highlights the plastic surgeon’s role in AWR, reviewing key reconstructive techniques, including pedicled and free flaps, perforator-based approaches, functional muscle transfers and abdominal wall allotransplantation. Material & MethodsAn overview of plastic surgical techniques for AWR is presented and a retrospective analysis of AWR cases in our unit was conducted, focusing on surgical techniques, indications, and outcomes of flap-based reconstructions. ResultsPlastic surgical techniques are essential for complex AWR. Pedicled and free flaps provide robust soft-tissue coverage, enhance vascularized support, and reduce recurrence rates. The rectus abdominis, external oblique, tensor fasciae latae, and anterolateral thigh flaps remain workhorses in reconstruction. Free tissue transfer, including the latissimus dorsi and gracilis flaps, offers solutions for extensive defects or prior failed repairs. Functional muscle transfer, particularly the rectus femoris or chimeric anterolateral thigh flaps, is crucial for restoring dynamic abdominal wall support. Flap-based approaches yield high success rates, particularly in contaminated fields where mesh use is limited. ConclusionsPlastic surgeons provide expertise in flap-based reconstruction for functional and aesthetic restoration in AWR. Advancements in perforator-based and functional muscle flaps continue to refine outcomes, highlighting the need for a multidisciplinary approach. Further research is needed to optimize flap selection and integration with evolving AWR strategies. |
||
|
08:00 – 09:30
Auditorium B
|
Residents training - an international comparison with the Swiss system
Seraina Faes, Zurich; Guido Beldi, Bern
|
|
|
Main Session
|
||
|
08:00–08:07
Training in the operation room in Switzerland. Results form the national survey 2024
Dieter Hahnloser, Lausanne
|
||
|
08:10–08:25
The Swiss system
Joëlle Zingg, Winterthur
|
||
|
08:26–08:41
The US system
Beat Möckli, Geneva
|
||
|
08:42–08:57
The French system
David Fuks, Lausanne
|
||
|
08:58–09:13
The German system
Karoline Horisberger, Mainz DE
|
||
|
09:14–09:29
The Danish system
Christoph Tschuor, Copenhagen DK
|
||
|
08:00 – 09:30
Room 1A
|
SGG - Free Communication 2
Simone Hofer, Chur; Sébastien Déglise, Lausanne
|
|
|
Free Communication
|
||
|
08:00–08:07
Outcome of Infrarenal Sealing With a Conformable Stentgraft System in Abdominal Aortic Aneurysms With Hostile Neck Anatomies
Simone Hofer, Chur
AbstractBackgroundInfrarenal aortic aneurysms with hostile neck anatomies are often treated by fenestrated/branched endovascular aortic repair or by open repair. Both strategies show a higher complication and mortality rate in literature than standard infrarenal endovascular aortic repair (EVAR). AimsWe analyzed the outcome of abdominal aortic aneurysms (AAA) with hostile neck anatomies (HN) treated by EVAR with a conformable stentgraft system (CSS) at our institution. MethodsFrom April 2019 until December 2024 all patients treated by CSS with HN in AAA were analyzed. We defined HN according to the Delphi Consensus (Marone et al, 2020) and asigned five risk factors (RF): neck length, width, angulation, thrombosis/calcification, conic/barrell shape. Technical success rate, short and long term outcome (30 day mortality, reintervention rate, sac behavior) were analyzed. Results100 patients with HN were treated by CSS. Three patients showed a HN with 5 RF, 14 with 4, 20 with 3, 30 with 2, and 33 with one RF, respectively. The technical success rate was 99%. 29 patients showed an endoelak type IA (ELIA) in the angiogram and/or early postoperative CT scan, of these 28 ELIA were resolved after 6 weeks. 30 day mortality was 1%. The median and mean follow-up time was 14 and 20 months. 5 patients had no follow-up CT scan. 4 patients needed a neck related reintervention, two underwent cuff-implantations because of an early (patient with one RF) and a late onset ELIA (4 RF) and two RedoEVAR due to stentgraft migration (4 and 5 RF). In 72% of all patients we achieved sac shrinkage and in 21% sac stabilization. ConclusionInfrarenal sealing in HN seems to be a safe option with a good outcome and acceptable reintervention rate. This treatment strategy should be be considered more often and thus, avoiding higher risk surgical procedures. |
||
|
08:11–08:18
Monocentric Experience on the Open Surgical Treatment of Aortic and Aorto-Iliac Aneurysms
Pietro Federico Ricciardi, Lausanne
AbstractBackgroundEndovascular aortic aneurysm repair has become the standard for treating standard abdominal aortic aneurysms (AAA). For complex AAAs, such as juxta-/suprarenal, open surgical repair—entailing suprarenal clamping and, when necessary, reconstruction of the visceral/renal arteries—has historically been considered the gold standard. Nevertheless, newer fenestrated and branched endovascular techniques, provide a valid alternative. Recent ESVS guidelines recommend choosing between open and endovascular repair based on patient fitness, anatomy and preferences. AimsThis study evaluates the results of open surgery for AAA of various complexities, focusing on complications and mortality. MethodsThis single-center retrospective study analyzed 185 consecutive patients who underwent open surgery for AAA and aorto-iliac aneurysms between 2017 and 2023. Primary outcomes were 30-days, and overall mortality, while secondary outcomes focused on postoperative complications, especially acute kidney injury (AKI). ResultsAmong the 185 patients, 85.95% were male, with a mean age of 70 years. The majority (70.27%) had infrarenal aneurysms, while 27.57% were juxtarenal and 2.16% suprarenal. The mean aneurysm diameter was 59.35 mm, and 73.51% were fusiform. Of the procedures, 83.78% were elective, with 96.22% performed via median laparotomy. Clamping was infrarenal in 67.57%, inter-renal in 12.43%, and suprarenal in 20%, with a mean renal ischemia time of 33.5 minutes. The 30-day mortality was 0.54%, while overall mortality, on a mean follow-up of 38 months, was 8.11%. Postoperative complications included pulmonary insufficiency (16.22%), minor cardiac events (6.49%), acute limb (2.7%), colitis (2.16%), and spinal cord (1.08%) ischemia. AKI rate was 14.05%. 3.78% persist at 30-days, without long-term dialysis. Late complications included symptomatic incisional hernias (9.73%) and prosthesis infection (1.62%). Peri-operative reintervention rate (aortic and non-aortic related) was 8.11%. ConclusionOpen surgery remains an effective and viable option for treating AAA, especially in complex cases unsuitable for endovascular repair. Managing cardio-pulmonary and renal function preoperatively is crucial for improving outcomes. |
||
|
PSGG25
08:22–08:29
Exploring the Need for Standardization and Practice Recommendations in Physician-Modified Endografts for the Treatment of Abdominal Aortic Aneurysms: a Cross-Sectional Survey
Giorgio Prouse, Lugano
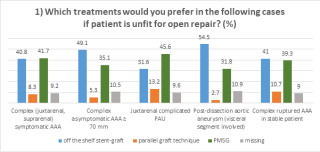
AbstractBackgroundPhysician-modified endografts (PMEGs) are increasingly used to treat complex abdominal aortic aneurysms (cAAA), especially when custom-made grafts are unfeasible. Despite their growing use, PMEGs lack standardization and are influenced by practitioner experience and institutional resources. AimsTo evaluate PMEG practices and identify areas for standardization to guide future expert-driven recommendations. MethodsA global cross-sectional survey was conducted using the EDDDIE platform, with 31 questions across six sections covering practitioner demographics, indications, device selection, planning, technical preparation, and free-text comments. Invitations were sent to 4,286 vascular specialists, supplemented by targeted outreach through professional platforms and social media. Responses were collected anonymously and analyzed using descriptive statistics and subgroup analyses. ResultsOf the 1,542 respondendents who accessed the survey link, 227 from 30 countries completed it. Among participants, 40% reported limited PMEG experience, while 25% had performed over 30 procedures. PMEGs were most commonly selected for symptomatic cAAAs, ruptured juxtarenal AAAs, and perforating aortic ulcers (Fig.1). Confidence in addressing challenging anatomies (Fig.2), such as small target vessel diameters or severe stenosis, was significantly higher among practitioners with greater experience. Thoracic grafts were the most frequently used devices (52%), followed by bifurcated abdominal endografts (30%). Approximately 67% of respondents did not use 3D-printed templates, though 22% employed them routinely, often with in-house printing capabilities. Planning preferences for minimal proximal sealing zones varied widely, with 33% opting for at least 20 mm. Amognst technical modifications, preloading vessel fenestrations and using reducing ties showed significant variability based on practitioner experience. ConclusionThe study underscores the differences in PMEG practices and the need for standardization to enhance patient safety and outcomes. Findings provide a foundation for further efforts to develope practice recommendations based on the areas of strong variability detected. 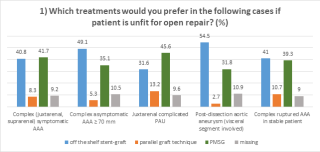
|
||
|
08:33–08:40
Outcomes of Staged Endovascular Repair with FET, TEVAR, and f/bEVAR for Complex Aortic Pathologies: A Single-Centre Experience
Camilla Schürmann, Bern
AbstractBackgroundA staged treatment approach combining open arch repair with Frozen Elephant Trunk (FET) technique, Thoracic Endovascular Aortic Repair (TEVAR), and either Fenestrated or Branched Endovascular Aortic Repair (f/bEVAR) has emerged as a less invasive treatment of thoraco-abdominal aortic aneurysms extent I to III. Nevertheless, this approach imposes significant physiological stress, with the risk of postoperative complications after open repair and rupture in the interval between interventions. AimsThis study analyses the early and late major adverse events (MAEs), including spinal cord ischemia (SCI) and stroke, target vessel instability, reinterventions and mortality rates after this combined treatment. MethodsThis is a single-centre retrospective study conducted in a high-volume tertiary aortic centre between January 2017 and December 2024. Patients treated with a combination of FET, TEVAR and f/bEVAR were included. All included patients had at least six months of follow-up. Outcomes were early and late major adverse events (MAEs), including spinal cord ischemia (SCI) and stroke, target vessel instability, reinterventions and mortality rates. ResultsDuring this period, 500 patients received FET. 100 had afterwards TEVAR for distal FET extension. Twelve patients (seven males) with a mean age of 68.5 ± 6 years received an additional f/bEVAR. Spinal cord ischemia, stroke and 30-day mortality rates were 17% (2/12), 8% (1/12) and 8% (1/12), respectively. Liquor drainage was performed in 17% (2/12) patients. Two patients died during follow-up, one of which was aortic related. Two patients required reintervention during follow-up: one due to type Ib endoleak and another due to bridging stent occlusion of the truncus coeliacus and superior mesenteric arteries. ConclusionThe staged approach combining FET, TEVAR, and FEVAR or BEVAR provides a feasible and durable solution for complex aortic diseases, with low mortality, acceptable complication rates, and low rate of target vessel instability. Further studies are needed to confirm long-term durability and safety. |
||
|
08:44–08:51
Patterns of Rupture After Endovascular Aortic Repair
Aita Sommerau, Chur
AbstractBackgroundRupture of abdominal aortic aneurysm (AAA) after endovascular aortic repair (EVAR) is rare but represents a critical treatment failure. It poses a significant risk to patient outcome. AimsThe objective of this study was to investigate incidence, causes, treatment options and clinical outcome in patients with ruptured AAA after EVAR (raE) in a single center cohort. MethodsOut of all patients after EVAR between June 2008 and December 2024, we identified those sustaining raE. Data collection included endoleak (EL) type, treatment modality, technical success rate and 30-day mortality. Results494 patients after EVAR were included in our surveillance program. Six cases of raE (1.2%) occurred. The majority of patients underwent regular follow-up imaging after primary EVAR, with the last surveillance on average one year before rupture (range 0.1-3.3 years). The follow-up was uneventful with aneurysm shrinkage in five patients (83%) (mean shrinkage 10mm, range 0-27mm). No graft migration could be discerned. The mean time interval between initial repair and raE was 3.9 years. In two patients the cause of raE was an EL type I A, in two an EL type I B and in two an EL type III. One patient underwent open repair, five were treated endovascularly. Technical success rate was 100%, 30-day mortality 0%. ConclusionFollow-up after EVAR is an important pillar of successful endovascular aneurysm treatment. But even with regular monitoring after EVAR and imaging showing sac shrinkage, there is a residual risk of aneurysm rupture, with EL type I and III leading to raE. The patients can be treated mainly endovascularly with a good outcome. |
||
|
08:55–09:02
Branched endovascular aortic repair after failed fenestrated endovascular aortic repair: Technical Note
Vaiva Dabravolskaite, Bern
AbstractBackgroundDurability after fenestrated/branched endovascular aneurysm repair B/FEVAR remains a concern, as both techniques have unique challenges due to their complex nature. Late type I or III endoleak (EL) is a rare complication after FEVAR. We describe the use of BEVAR with inner branches after failed FEVAR. Case_presentationThree male patients (#1 82, #2 80 and #3 68 years old) presented with an expansion of the aortic sac after FEVAR with type Ia, type III and Ib, respectively. One custom-made inner branch (#1) and two (#2 and #3) off-the-shelf E-inside branched grafts (Artivion, NW, Kennesaw, GA 30144, USA) were used. Patient #1 presented with type Ia EL after previous 3x FEVAR due to juxtarenal AAA. Patient #2 had thoracic EVAR and 4- FEVAR for thoracoabdominal aortic aneurysm type III. Patient #3 was treated with a thoracic EVAR and with one fenestration physician-modified FEVAR for truncus coeliacus (TC) due to subacute Stanford B aortic dissection. Three months later patient presented to the emergency department with back pain and aneurysm progression. The TC branch and the bridging stent to TC could not be catheterized due to limited intraortal space, however, perfusion was provided via collaterals. Begraft Plus covered stents (Bentley, Hechinger, Germany) were used as bridging stents for all target vessels. Operating and fluoroscopy times were 325, 291, 322, and, 175, 133, and 127 minutes, respectively. Patient 1# died six months after the procedure due to non-aortic related causes; patient #2&3 completed one-year and 6-months follow-ups without endoleak or target vessel instability. ConclusionFailed fenestrated repair can be successfully treated with custom-made or off-the-shelf branched devices with inner branches. The above-described approach is technically demanding but allows a novel-treating alternative. 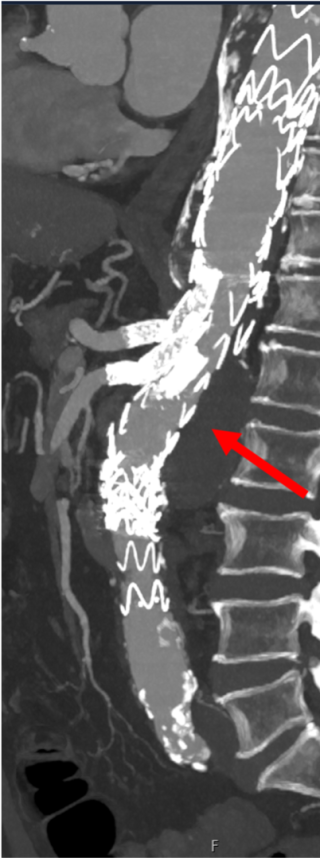
|
||
|
09:06–09:13
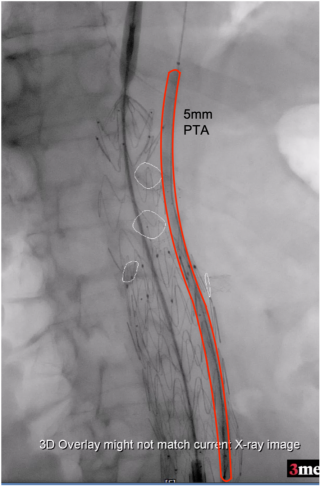
Intentional Creation Of Gutter Leak To Reduce RenovVisceral Ischemia During Urgent Paravisceral Aortic Aneurysm Treatment With In Situ Laser Fenestration: Technical Note
Vaiva Dabravolskaite, Bern
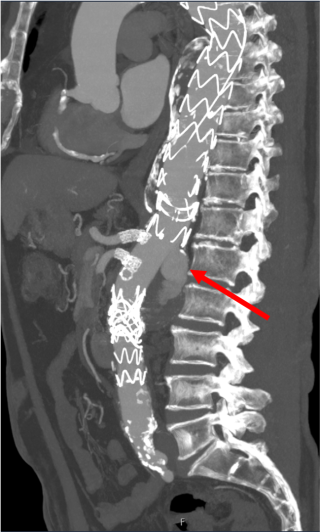
AbstractBackgroundEmergent repair of paravisceral aortic aneurysms (pAA) with in situ laser fenestration (ISLF) technique is associated with renovisceral ischemia due to the need to cover the target arteries prior to ISLF creation. We describe two alternative strategies of temporary gutter leak creation to ensure renovisceral perfusion during ISLF repair of symptomatic pAA. Case presentationA 79-year-old and an 83-year-old patient, deemed unfit for open repair, presented with a symptomatic pAA. A Cook Zenith Alpha tubular endograft (Cook Medical LLC, Bloomington, IN, USA) was used in both cases. All visceral vessels were pre-stented to serve as a guide marker during ISLF. Prior to the deployment of the endograft, a Cook Flexor 8F sheath (Cook Medical LLC, Bloomington, IN, USA) was placed in the superior mesenteric artery (SMA) (patient #1) (Figure 1), and a 6 x 200 mm angioplasty balloon (Figure 2) was placed between the endograft and the aortic wall (patient #2). Angiograms after visceral coverage confirmed perfusion of the renovisceral arteries through gutter endoleaks. Thereafter, ISLF and bridging stenting for SMA and the renal arteries were performed before the removal of the sheath or PTA balloon to stop the gutter leak. Both patients did not experience any intra- and postoperative complications. No clinical or laboratory signs of renovisceral malperfusion were detected.
ConclusionThe above-described techniques for gutter leak creation during emergent pAA repair with ISLF can potentially reduce reno visceral ischemia and increase the ISLF technique's safety. 
|
||
|
09:17–09:24
GORE® EXCLUDER® Iliac Branch Endoprosthesis: Relevance of Current Instructions for Use
Sophia Ruddakies, Chur
AbstractBackgroundThe GORE® EXCLUDER® Iliac Branch Endoprosthesis (GoIBE) provides endovascular treatment of common iliac artery or aortoiliac aneurysms. It includes an iliac branch component and an internal iliac component (IIC) extending into the internal iliac artery (IIA). The latest instructions for use (IFU) were published in February 2022. AimsThis study evaluates the utility of the current IFU by comparing outcomes between GoIBD implanted within and outside IFU criteria. MethodsA retrospective review of patients undergoing GoIBE surgery between 2015 and 2023 at our institution was conducted, focusing on intraoperative success, postoperative outcomes, and reinterventions. The IFU criteria were analyzed, including femoral/iliac access, presence of aortoiliac or common iliac artery aneurysm, adequate sealing zones of the internal and external iliac artery, proximal landing zone diameter of the common iliac artery and use of an aortoiliac endoprosthesis. ResultsAmong 75 patients with 94 GoIBE implanted, 20 met all IFU criteria, while 74 were implanted outside IFU. In total 22 reinterventions were performed. 18 in the outside-IFU group and 4 in the within-IFU group (p=0.685). Postoperative complications were observed in 5 cases, each belonging to the outside-IFU group (p=0.581). Additionally 5 intraoperative complications occurred, all in the outside-IFU group (p=0.581). Two intraoperative IIA occlusions were recorded, one additional occlusion occurred during follow-up. ConclusionThere were no significant differences in intraoperative or postoperative complication rates between devices implanted within or outside IFU criteria, suggesting that deviations from the IFU do not inherently compromise procedural outcomes. Follow-up surgery rates were also comparable. Implanting the GoIBE outside IFU appears to be a safe and effective option, allowing for the preservation of the internal iliac artery in most cases. |
||
|
08:00 – 09:30
Room 1C
|
Treatment of burned children (MHS) in Zurich and in Lausanne: similarities and differences
Kathrin Neuhaus, Zurich; Anthony de Buys Roessingh, Lausanne
|
|
|
Main Session
|
||
|
08:00–08:05
Benefits of sphincteroplasty on speech in children with velopharyngeal insufficiency and cleft lip and palate
Marion Poget, Lausanne
AbstractBackgroundVelopharyngeal insufficiency (VPI), a potential sequela of cleft lip and palate (CLP) repair, is the passage of air from the oral cavity into the nasal cavity during phonation. An altered nasal resonance, sometimes translated as a high-pitched voice, is a compensatory mechanism for VPI and may worsen intelligibility. The treatment of VPI is based on speech therapy; surgical intervention may be considered if symptoms persist. The most commonly used techniques are superior/inferior pharyngeal flap or sphincteroplasty. These two techniques have not shown any difference in terms of hypernasality, i.e., the passage of air through the nasal cavity during speech. However, the alteration of nasal resonance, with the clinical manifestation of a high-pitched voice, has not yet been studied in the literature. AimsThe aim of this study is to investigate the change in nasal resonance following sphincteroplasty. MethodsThis study includes children born with a CLP who underwent sphincteroplasty for VPI between April 2023 and July 2024 at our university hospital. Pre- and postoperative phonation assessments were carried out using the Borel-Maisonny classification and vocal frequency measurements obtained with a validated phonetic analysis software. ResultsFive out of six children, aged 12 to 19 years, showed postoperative phonation improvement. A decrease in vocal frequency was observed in the four children who had a high-pitched voice preoperatively. ConclusionThe results demonstrate a reduction in VPI and a decrease in vocal frequency following sphincteroplasty, resulting in a more harmonious voice quality and better intelligibility. These findings suggest that sphincteroplasty may offer additional benefits over pharyngeal flap. A prospective study with a larger cohort of patients undergoing sphincteroplasty, and with a longer recruitment period, is being conducted. This study will precede a comparative analysis between these two pharyngoplasty techniques. 
|
||
|
08:07–08:12
ICP elevation in scaphocephaly - a retrospective study
Johanna Eber, Lucerne
AbstractBackgroundSynostosis of the sagittal suture resulting in scaphocephaly is known to be the most common form of craniosynostosis. Although the severity of presentation may vary, there is a large consensus on the indication for surgical treatment due to an increased risk of intracranial pressure (ICP) and the abnormal skull shape. However, the prevalence and significance of elevated ICP remains unclear. AimsTo evaluate a patient cohort with delayed diagnosis of scaphocephaly with regard to ICP elevation. MethodsA retrospective study of a cohort of five patients with delayed diagnosis of scaphocephaly. As a control group, we included three infants who underwent osteoclastic craniectomy within the same time. The data collection involved meticulous reviews of medical records, diagnostic imaging, and clinical assessments, with a focus on demographics, clinical presentations, imaging results, Cranial Index (CI) measurements, presence of papilledema, and intraoperative documentation, including ICP measurements. ResultsThere was no significant difference in the preoperative CI between the two groups (p = 0.14). All patients diagnosed with scaphocephaly were assessed for papillary edema by our ophthalmologists. Two cases in the late-treatment scaphocephaly group presented with papillary edema at diagnosis. There were no cases of papillary edema in the control group. All five late treatment-group scaphocephaly patients underwent modified Pi-plasty procedures with systematic ICP-monitoring. The mean opening pressure was 24mmHg which significantly dropped to a mean closing pressure of 7.5mmHg. In comparison, the control group had a significantly lower mean opening pressure of 5mmHg (p < 0.01). ConclusionOur study demonstrates that all patients in the late-treatment scaphocephaly group showed elevated intracranial pressure at the time of surgery. Despite variability in presentation, the elevated ICP in these patients highlights the importance of timely diagnosis and intervention to mitigate the risk of intracranial hypertension. |
||
|
08:14–08:19
Single-Center Experience With Pediatric Endoscopic Pilonidal Sinus Treatment (PePSiT): A Safe and Low-Recurrence Minimally Invasive Technique in the Paediatric Population
Marco Garatti, Bellinzona
AbstractBackgroundPilonidal sinus disease (PSD) is a common condition affecting the natal cleft, often complicated by infection or abscess formation. Traditional surgical approaches include excision with open wound healing or primary closure. Minimally invasive techniques, such as pediatric endoscopic pilonidal sinus treatment (PePSiT), have shown significant improvements in outcomes. This study reports our single-center experience with PePSiT in paediatric patients. AimsTo evaluate the safety, efficacy, and long-term outcomes of PePSiT as a minimally invasive treatment for PSD in paediatric patients. MethodsA retrospective analysis was conducted on 72 paediatric patients treated between 2015 and 2024. All patients followed a standardized protocol, including preoperative laser hair removal therapy. A minimum follow-up of 2 years was ensured, except for recent cases still under observation. Outcomes assessed included healing rates, morbidity, PSD characteristics, recurrence rates, and quality of life (QoL). Patients older than 18 years were excluded. ResultsThe mean age was 15.4 ± 1.6 years (range 11.6–18), with a male-to-female ratio of 1.3:1. Large cavities (>3 cm) were present in 27.8% of cases, and abscess formation was the most common presentation (49%). The mean procedure duration was 35 ± 8.8 minutes. All patients were discharged the same day, resumed activities within 10 days, and achieved complete wound healing within 4 weeks in 96% of cases. The overall recurrence rate was 6.9%, decreasing to 3.8% in the last 5 years. ConclusionPePSiT is a safe, effective, and minimally invasive treatment for PSD in paediatric patients. Its low recurrence rate, absence of hospitalization, and inclusion of laser hair removal therapy improve outcomes and reduce costs. PePSiT is recommended as a first-line treatment for this age group, with future studies needed to confirm these findings |
||
|
08:30–09:30
Joined talk: Treatment of burned children (MHS) in Zurich and in Lausanne: similarities and differences
Kathrin Neuhaus, Zurich; Anthony de Buys Roessingh, Lausanne
|
||
|
08:00 – 09:30
Room 5A
|
Video: How I do it?
Antoine Meyer, Fribourg; François Pugin, Fribourg
|
|
|
Main Session
|
||
|
08:00–08:10
Concomitant laparoscopic cholecystectomy and transcystic balloon sphincteroplasty for the treatment of choledocholithiasis
Gian Andrea Prevost, Chur
|
||
|
08:13–08:23
Intracorporeal anastomosis – how I do it
Amaniel Kefleyesus, Lausanne
|
||
|
08:26–08:36
Complex pulmonary segmentectomy by RATS
Etienne Abdelnour-Berchtold, Lausanne
|
||
|
08:39–08:49
Proximal femoral nailing: How we do it?
Matthias Christen, Fribourg
|
||
|
08:52–09:02
LumenEye Rigid Rectoscopy: technique and indications
Daniel Clerc, Sion
|
||
|
09:05–09:15
Perioperative Indocyanine green lymphangiography is a useful adjunct for the management of lymphatic complications after vascular surgery – How I Do it
Emmanouil Psathas, Fribourg
|
||
|
09:18–09:28
Robotic major hepatectomy
Emmanuel Melloul, Lausanne
|
||
|
09:30 – 10:00
|
Coffee Break |
|
|
Break
|
||
|
09:30 – 09:55
Room 1B
|
General Assembly International College of Surgeons |
|
|
Assembly
|
||
|
10:00 – 11:30
Room 5B
|
Bariatrics
Minoa Karin Jung, Geneva; Christian A. Nebiker, Aarau
|
|
|
Free Communication
|
||
|
10:09–10:16
Reversal of Roux-en-Y Gastric Bypass:A Multi-centric Analysis of Indications, Techniques and Surgical Outcomes
Liane Plath, Zuerich / Maennedorf
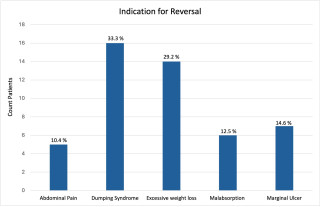
AbstractBackgroundRoux-en-Y gastric bypass may present long-term complications that require revisional surgery or even reversal to normal anatomy (Figure1). Data on the indications, surgical technique and outcomes of RYGB-reversal remain scarce.
AimsTo analyze indications, techniques and surgical outcomes after reversal of Roux-en-Y gastric bypass. MethodsWe identified 48 cases of RYGB-reversals with complete 90-day follow-up within a multi-centric international retrospective database of elective secondary bariatric surgery. The operations were performed between 2010–2024 in high volume referral centers in Europe and USA. Data were collected on body weight, associated diseases and on surgical outcomes up to 1-year postoperatively. ResultsPatients were mainly female (81.3%) with a median age of 50 years (IQR 39-56). RYGB-reversal was performed 7 years (median) after primary RYGB in patients with a BMI 23.9 kg/m2 (IQR 20-27). Half of the patients underwent at least 1 bariatric revision before the reversal. Main indications for reversal were dumping syndrome (33.3%), excessive weight loss (29.2%), marginal ulcer (14.6%), malabsorption (12.5%) and abdominal pain (10.4%). Rate of conversion to open surgery was 8.3% and the postoperative complications during the first year reached 50%, including 31.3% Clavien-Dindo grade I-II, 16.7% grade III-IV complications and one death. At 1-year, the mean BMI of the cohort increased by 18% to 28.25kg/m2; only 1 patient reached pre-RYGB BMI. ConclusionAlthough RYGB is a theoretically reversible procedure, normal anatomy is re-established only in selected cases which are refractory to medical therapy and often also to revisional bariatric surgery. RYGB-reversals entail high morbidity, while the extent of recurrent weight gain at 1-year post-reversal seems to allow patients to remain below the threshold of severe obesity. 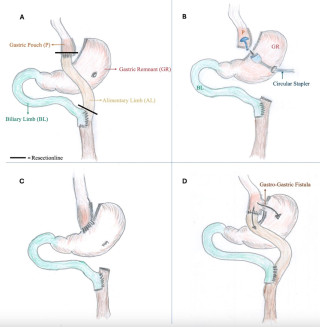
|
||
|
10:18–10:25
Preoperative Eating Patterns and their Effect on Post-operative Outcomes in Bariatric Surgery: A Cohort Study of 1550 Patients
Adisa Poljo, Basel
AbstractBackgroundAlthough surgical procedures like Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are highly effective, postoperative outcomes can differ significantly between individuals. These differences are shaped by a range of factors, including preoperative behaviors and psychological traits. Eating disorders (EDs), particularly binge eating, have been linked to less favorable weight loss outcomes following surgery. Certain guidelines even consider severe EDs as contraindications for bariatric surgery. AimsThe aim of this study was to investigate the influence of different EDs on the postoperative outcome of patients undergoing bariatric surgery. MethodsIn a retrospective analysis of prospectively collected data, patients who underwent RYGB or SG between January 2010 and December 2018 were examined. Patients were categorized by preoperative eating patterns, including binge eating, snacking, and high consumption of sweets or fatty foods. Demographics, early morbidity, and five-year follow-up data on weight loss, comorbidities, and complications were collected. Outcomes were assessed using the SF-Bari Score, a composite endpoint integrating weight loss, comorbidity improvement, and surgical complications. ResultsAmong 1,550 patients, eating patterns varied widely, with most exhibiting multiple EDs. ED patients were younger with higher baseline BMI. Total body weight loss (TBWL%) was initially higher in ED patients but differences diminished over time. SF-Bari Scores were also higher in ED patients at 5 years. RYGB consistently showed lower BMI, higher TBWL%, and higher SF-Bari Scores than SG. RYGB yielded better outcomes for Binge and Sweet ED patients, while significant differences for Nightly ED appeared after 2 years. Female patients achieved greater weight loss and SF-Bari Scores overall. ConclusionPre-operative EDs appear to have minimal or no significant impact on postoperative outcomes after bariatric surgery. These findings suggest the need to reconsider current guidelines, particularly the classification of severe EDs as contraindications for bariatric surgery. |
||
|
10:27–10:34
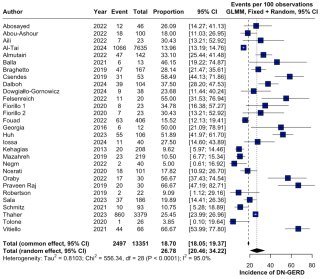
The De Novo GERD Puzzle After Sleeve Gastrectomy: A Meta-Analysis and Meta-Regression of Possible Predisposing Factors
Filippo Bistagnino, Luxembourg LU / Milano LU
AbstractBackgroundSleeve gastrectomy (SG) is one of the most performed bariatric procedures, yet its association with gastroesophageal reflux disease (GERD) remains debated. A substantial proportion of patients develop de novo GERD (DN-GERD) following SG, likely due to anatomical and physiological changes, highlighting the need to identify potential preoperative predictors that could inform risk stratification and guide surgical technique. AimsThis meta-analysis aims to identify preoperative predictors of DN-GERD after SG. MethodsRelevant studies were retrieved from PubMed, Embase, and the Cochrane Library that reported DN-GERD incidence among SG patients without symptomatic preoperative GERD. Only studies that explicitly excluded patients with preoperative GERD and employed a standardized follow-up protocol (using a uniform DN-GERD diagnostic method) were included. A meta-analysis of proportions was performed using a random-effects model with logit transformation to account for heterogeneity.
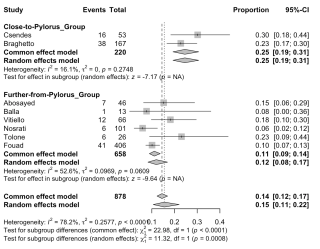
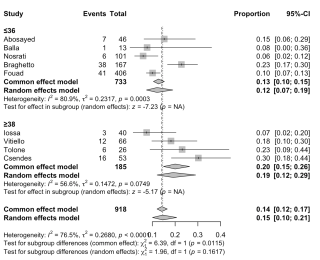
ResultsOut of 2’977 studies, 29 satisfied inclusion (13’351 patients). The overall incidence of DN-GERD was 26.8% (95%CI 20.5%–34.2%) as shown in Figure 1. Further analyses were conducted grouping studies by diagnostic approach: 24 used symptom-based (S) assessment, yielding a 23.2% incidence (95%CI 17.3–30.3%); 11 employed endoscopy (E), reporting 17.9% (95%CI 11.7–26.3%); and 6 utilized 24-hour pH-monitoring (P), with 48% (95%CI 32.6-63.8%). Substantial heterogeneity prompted meta-regression and subgroup analyses. Male sex was linked to higher GERD rates in S group (p=0.0171). In E group, a <4cm dissection from the pylorus showed higher DN-GERD rates (p=0.0008), while no significant difference was observed based on Bougie size (≤36Fr vs. ≥38Fr; p=0.1617) as shown in Figure 2 and 3 respectively. ConclusionThis meta-analysis underscores the considerable variability in DN-GERD incidence when assessed by symptoms, endoscopy, or pH monitoring. Male sex might predispose to symptomatic GERD. A <4cm dissection might lead to a higher reflux. Additional standardized studies are urgently warranted to further optimize these SG outcomes.
|
||
|
10:36–10:43
Impact of preoperative GLP-1 agonist receptor treatment on metabolic and bariatric surgery outcome
Pauline Aeschbacher, Bern
AbstractBackgroundGlucagon-like peptide-1 (GLP-1) receptor agonists have transformed obesity treatment, offering a rapid and safe approach to significant weight loss. However, metabolic and bariatric surgery (MBS) remains an effective option, achieving total weight loss (TWL) of 25%–35% of presurgical body weight. The role of GLP-1 use prior to MBS in patients requiring surgery due to insufficient weight loss or weight regain after GLP-1 treatment remains largely unexplored. AimsThis study aims to assess the potential effects of preoperative GLP-1 receptor agonist treatment on postoperative outcomes following MBS. MethodsThis retrospective, single-center study analyzed patients who underwent MBS between January 2022 and December 2023. Postoperative outcomes and 12-month %TWL were compared between patients with prior GLP-1 receptor agonist treatment and those without. ResultsAmong the 236 patients included, 70% (n=165) were female. The median age was 39 years (IQR 31–51), and the median BMI was 42 kg/m² (IQR 39–45). The median follow-up duration was 14 months, with 75% of patients having at least 12 months of follow-up. MBS procedures included Sleeve Gastrectomy (n=176, 74%) and Roux-en-Y Gastric Bypass (n=60, 25%). Half of the patients (n=118) received preoperative GLP-1 receptor agonist treatment (liraglutide or semaglutide). 69% (n=82) had treatment failure (>5% %TWL or >10% weight regain). Patient characteristics (except for dyslipidemia), operation time, length of stay, overall and major postoperative morbidity, and readmission rates were similar between the groups. However, %TWL at 12 months was significantly higher in patients without prior GLP-1 receptor agonist treatment (30% vs. 26%, p=0.043) especially when compared to patient with GLP-1 treatment failure (p=0.007). ConclusionPreoperative GLP-1 treatment may be associated with lower %TWL after bariatric surgery, potentially due to intrinsic factors or the effects of GLP-1 exposure. Further research is needed to clarify these mechanisms. |
||
|
10:45–10:52
GLP-1 Agonists and Bariatric Surgery: Does Preoperative Treatment Make a Difference?
Adisa Poljo, Basel
AbstractBackgroundObesity is a chronic disease associated with systemic dysfunction and increased risk of serious health conditions, requiring multifaceted treatment approaches. Although bariatric surgery remains the most effective option, pharmacotherapy—particularly glucagon-like peptide-1 receptor agonists (GLP-1 RAs)—has recently gained recognition as a promising alternative or complement to surgical intervention. AimsThis study compares the outcomes of bariatric surgery in patients treated with and without preoperative GLP-1 receptor agonists, exploring their impact on weight loss, comorbidity resolution, and reasons for transitioning to surgery. MethodsWe conducted a retrospective analysis of patients undergoing laparoscopic Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (SG) between 2015-2020, excluding those with revisional surgeries, postoperative GLP-1 therapy, or pregnancies during follow-up. Patient outcomes, including weight loss, comorbidity resolution, and surgical complications, were assessed. ResultsAmong 192 eligible patients, 43 received GLP-1 therapy before bariatric surgery, while 149 did not. Baseline characteristics, including age, BMI, and surgery timing, were similar, though diabetes prevalence was higher in the GLP-1 group. No significant differences in weight loss, resolution of arterial hypertension, dyslipidemia and OSAS, or complication rates were observed during the three-year follow-up. Diabetes remission rates were significantly higher at three months in patients without prior GLP-1 treatment, but no differences were observed beyond this point. Both groups achieved "Fair response" SF-Bari Scores at all time points, with similar complication rates and severity. Patients in the GLP-1 group transitioned to surgery for definitive treatment, due to side effects or unavailability of medication. ConclusionPreoperative GLP-1 therapy does not appear to affect long-term weight loss outcomes, resolution of comorbidities or complications rates following bariatric surgery. |
||
|
10:54–11:01
Surgical Versus Endoscopic Outlet Reduction for Weight Regain and Dumping Syndrome After Roux-en-Y Gastric Bypass: A Single-Center Retrospective Mid-Term Follow-Up Study
Maren Djajadisastra, Luzern
AbstractBackgroundOver the last decades, obesity and its co-morbidities have reached pandemic dimensions. Nearly 60 percent of European adults are overweight. This disease leads to decreased quality of life, high mortality and immense socio-medical and socio-economic burden. Bariatric surgery, i.e. Roux-en-Y gastric bypass (RYGB), is still the most effective therapy with excellent long-term results. Nonetheless, weight regain and dumping syndrome occur in a relevant number of patients, often due to a dilatation of the gastrojejunal anastomosis. Transoral outlet reduction (TORe) as well as implantation of a MiniMIZER Ring (IMR) are less invasive treatment options than bypass revision which has been the standard treatment in the past. AimsThe aim of the study was to compare the effectiveness of IMR with TORe in patients concerning weight regain or insufficient weight loss and dumping syndrome after RYGB. MethodsA single-center retrospective data analysis of 105 patients who underwent IMR, TORe or both from January 2018 to March 2024 was performed. 56 patients underwent TORe only, ten IMR only and 39 both interventions (Table 1). Primary endpoint was weight stabilization or weight loss for subjects with weight regain and remission of symptoms for those with dumping syndrome. Secondary endpoints were length of hospital stay, perioperative complications and revisional procedures. ResultsPatients after IMR more often accomplished weight loss or maintenance than those treated endoscopically (Figure 1: Follow-up at 48 months: 75 % after IMR versus 22 % after TORe). After IMR, more patients had a rapid and persisting dumping improvement compared to after TORe (Figure 2). Due to dysphagia after IMR ten patients needed surgical revision. ConclusionIMR is a safe and effective therapy for weight regain and dumping syndrome after RYGB. IMR showed better mid-term results compared to TORe, but some patients suffered from dysphagia. A prospective randomized controlled trial for long-term results is recommended. 
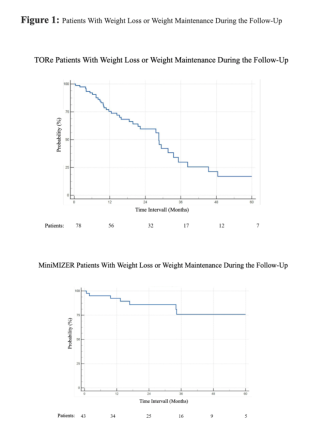

|
||
|
11:03–11:10
Conversion of Sleeve Gastrectomy to Roux-en-Y Gastric Bypass and One-Anastomosis Gastric Bypass: A Retrospective Study
Andreas Yves Lair Ferrari, Luzern / Lucerne
AbstractBackgroundBariatric surgery is a well-established treatment for morbid obesity. However, primary bariatric surgery may not always succeed in weight loss and can cause relevant side effects. Current literature lacks clarity on which bypass method is superior in redo operations for weight loss and gastroesophageal reflux. AimsThis study aims to compare the effectiveness of converting SG to either RYGB or OAGB in terms of weight loss and reflux control. MethodsA multicenter retrospective study was conducted on 72 adult patients who underwent conversion from SG to RYGB or OAGB between February 2014 and June 2023. The primary endpoint was the reasons for reoperation following SG — specifically, reflux or weight gain —and to evaluate which reoperation technique, either RYGB or OAG, results in the best outcomes for reflux relief and weight loss. Secondary endpoints included changes in weight, BMI, surgery duration, overall complication rate, and postoperative endoscopic findings. ResultsPatients’ characteristics showed no difference. RYGB was performed on 34.7% of patients for reflux and 47.2% for excess weight, while 18.1% underwent OAGB for excess weight. There were no intraoperative complications, and six postoperative complications occurred. Reflux symptoms significantly remitted in 95.8% of cases. The Kaplan-Meier analysis revealed no significant difference in weight loss between RYGB and OAGB procedures (RYGB HR 0.747, 95% CI 0.207-2.693, p=0.656). A Cox regression analysis showed no correlation with excess weight loss either (HR 1.863, 95% CI 0.479-7.253, p=0.369), even after adjusting for confounding variables. ConclusionOur study showed that conversion of SG to RYGB was effective for gastroesophageal reflux symptoms remission. For weight loss, both RYGB and OAGB seem to be equally effective during the follow-up. |
||
|
11:12–11:19
Ten-Year Outcomes of Roux-en-Y Gastric Bypass Following Failed Sleeve Gastrectomy: A Propensity-Matched Analysis with Primary Bypass Patients
Jonas Fischer, Bern
AbstractBackgroundAlthough sleeve gastrectomy (SG) is a commonly performed bariatric procedure, conversion to revisional Roux-en-Y gastric bypass (rRYGB) is a widely used method to treat patients who experience inadequate weight loss or recurrent weight gain. However, the long-term outcomes of rRYGB remain poorly studied. AimsThis study aimed to evaluate the 10-year weight efficacy and outcomes of patients who underwent revisional RYGB after SG (Cohort 1; C1) and compare these results with those of patients who underwent primary RYGB (Cohort 2; C2). MethodsThis retrospective cohort study analyzed a 10-year follow-up of bariatric patients. Patients who experienced insufficient weight loss (<20% total weight loss [TWL]) or recurrent weight gain) underwent revisional RYGB (rRYGB) after SG (n=28). These patients were propensity score-matched (1:1 nearest neighbor matching, caliper = 0.2) with primary RYGB patients (n=105) based on age, BMI, and sex. The primary endpoint was TWL%. ResultsAfter matching, 27 patients were included in each cohort. The median follow-up time was 10.9 years for Cohort 1 (C1) and 10 years for Cohort 2 (C2). The mean TWL% was 27.8 ± 10.7 for C1 and 31.7 ± 17.7 for C2, while the median TWL% values were similar at 28.8 for C1 and 29.4 for C2. Statistical analysis revealed no significant difference between the cohorts (Wilcoxon rank sum test, p = 0.6672; Cliff’s Delta = -0.073, 95% CI: -0.370 to 0.237), indicating a negligible effect size. ConclusionThis 10-year follow-up demonstrated that rRYGB after failed SG achieves comparable long-term weight loss outcomes to primary RYGB. |
||
|
11:21–11:28
Body Contouring Surgery in the Postbariatric Patient: Challenges and Opportunities
Mihai Constantinescu, Bern
DetailsBackgroundThe increasing prevalence of bariatric surgery has led to a growing number of patients seeking body contouring surgery (BCS) to address post-weight loss deformities. While BCS significantly improves health-related quality of life, there remains controversy regarding its functional versus aesthetic indications, affecting insurance coverage decisions. AimsThis study examines the indications, outcomes, and insurance coverage of common BCS procedures in post-bariatric patients. MethodsWe conducted a retrospective review of post-bariatric patients undergoing BCS in our unit, analyzing surgical techniques, patient outcomes, and insurance coverage rates. ResultsAbdominoplasty and circumferential body lifts are the most frequently performed procedures, followed by thigh lifts, brachioplasty, and breast surgery. Patient satisfaction is high, with favorable results and mainly minor complications requiring minimal surgical intervention. Combining BCS procedures is safe if excessive operative time and blood loss are avoided. Greater weight loss correlates with better outcomes, while higher preoperative BMI increases the risk of surgical site infections. Insurance coverage for post-bariatric BCS remains low (~40%), with abdominal procedures more likely to be covered than other surgeries. The absence of standardized criteria creates uncertainty for both patients and insurers. ConclusionsBCS effectively and safely corrects contour deformities after massive weight loss, with high patient satisfaction and low complication rates. However, inconsistent and subjective insurance coverage highlights the need for standardized guidelines to improve access and reduce frustration in this expanding patient population. |
||
|
10:00 – 11:30
Room 4A
|
EPAs - Train the Trainers
Steffen Geuss, Lucerne; Stefan Eisoldt, Männedorf; Henning Fischer, Lucerne
|
|
|
Course
|
We propose a workshop tailored for surgeons committed to enhance their teaching skills, with a focus on Entrustable Professional Activities (EPAs). As post-graduate medical training transitions towards a competency-based model, the SCS has introduced a Core Surgical Curriculum that is structured around a range of essential surgical competencies defined as EPAs. Implementing this new concept in daily work challenges surgical educators to advance their teaching methods and assessment strategies. In this 3-part workshop participants will explore the principles of competency-based education, focusing on EPAs, and gain practical tools for assessing competence, teaching procedural skills, and delivering effective feedback. Two 60-minute video sessions and one 90-minute face to face session |
|
|
10:00 – 11:30
Room 5A
|
FJC Session: The next guardians - journey to success
Joëlle Zingg, Winterthur; Michael Winiker, Lausanne
|
|
|
Main Session
|
||
|
10:00–10:15
Navigating through residency
Manuela Oberlechner, St. Gallen
|
||
|
10:15–10:30
Your surgical pathway: allrounder – specialist – academic
Rebecca Kraus, Chur
|
||
|
10:30–10:37
Subspecialties - Reaching the final destinationColorectal
Benjamin Weixler, Winterthur
|
||
|
10:40–10:47
Subspecialties - Reaching the final destinationHPB
Philip Müller, Basel
|
||
|
10:50–10:57
Subspecialties - Reaching the final destinationUpper-GI / Bariatrics
Seraina Oettli, St. Gallen
|
||
|
11:00–11:07
Subspecialties - Reaching the final destinationEndocrine
Robert Mechera, Männedorf
|
||
|
11:10–11:17
Subspecialties - Reaching the final destinationParietology
Henry Hoffmann, Basel
|
||
|
10:00 – 11:30
Room 1A
|
Guardian of the Scalpel: Securing excellence in miscellaneous vascular pathologies
Stephan Engelberger, Baden; Thomas Lattmann, Winterthur
|
|
|
Guardians of the Scalpel
|
||
|
10:00–10:07
Debate: The future of treatment in asymptomatic carotid stenosisOnly the best medical treatment
Florian Dick, St.Gallen
|
||
|
10:07–10:14
Debate: The future of treatment in asymptomatic carotid stenosisSurgery will remain the first choice
Justine Longchamp, Lausanne
|
||
|
10:14–10:21
Debate: The future of treatment in asymptomatic carotid stenosisEndo will be the solution (TCAR or CAS)
Claude Haller, Sion
|
||
|
10:21–10:30
Debate: The future of treatment in asymptomatic carotid stenosisDiscussion |
||
|
10:30–10:40
Debate: Internal iliac artery must be preserved in aorto-iliac treatmentFor the motion
Simone Hofer, Chur
|
||
|
10:40–10:50
Debate: Internal iliac artery must be preserved in aorto-iliac treatmentAgainst the motion
Sébastien Déglise, Lausanne
|
||
|
10:50–11:00
Debate: Internal iliac artery must be preserved in aorto-iliac treatmentDiscussion |
||
|
11:00–11:10
Debate: Acute mesenteric ischemiaOpen surgery first
Nicolas Attigah, Luzern
|
||
|
11:10–11:20
Debate: Acute mesenteric ischemiaEndovascular first
Edin Mujagic, Basel
|
||
|
11:20–11:30
Debate: Acute mesenteric ischemiaDiscussion |
||
|
10:00 – 11:30
Room 1C
|
Guardians of Pediatric Surgery
Anthony de Buys Roessingh, Lausanne; Luisa Heuer, Zürich
|
|
|
Guardians of the Scalpel
|
||
|
10:00–10:20
What we have achieved
Claude Le Coultre, Geneva
|
||
|
10:20–10:35
What do we cherish
Marc Schumacher, Zurich
|
||
|
10:35–10:50
Where will we go
Michael Gradwell, Basel
|
||
|
10:50–11:30
Panel Discussion |
||
|
10:00 – 11:30
Auditorium B
|
SCS - Outpatient reimbursement: Quo Vadis? All you need to know
Arno Stellmes, Lucerne; Beat Möckli, Geneva
|
|
|
Main Session
|
||
|
10:00–10:15
Reimbursement in outpatient surgery today
Guido Beldi, Bern
|
||
|
10:15–10:30
Update on political process
Marc-Olivier Sauvain, Neuchâtel
|
||
|
10:30–10:45
Reimbursement in outpatient surgery 01.01.2026
Torsten Franz, Uster
|
||
|
10:45–11:00
What can FMCH do?
Michele Genoni, Zurich
|
||
|
11:00–11:30
Roundtable, Discussion |
||
|
10:00 – 11:30
Room 1B
|
SGH - Free Communication
Silvia Schibli, Nottwil; Saskia Kamphuis, Basel
|
|
|
Free Communication
|
||
|
10:00–10:40
The dark side of the moon – from perilunate injuries to lunate replacement
Mathias Häfeli, Chur
|
||
|
10:40–10:47
Force Loss and Distribution of Load in Hands with Carpal Tunnel Syndrome
Kristina Rohmfeld, Bern
AbstractBackgroundCarpal tunnel syndrome is the most common entrapment syndrome of a peripheral nerve and is causing pain, sensory deficits and atrophy of the thenar. AimsThe functional deficit due to paralysis of the median nerve is not yet fully understood. For a better knowledge of the impact due to carpal tunnel syndrome, the force and contact area of the fingers, thumb and palm in addition with the load distribution of patients with carpal tunnel syndrome were subjected to a differentiated analysis. MethodsFor this clinical study, 30 patients with carpal tunnel syndrome were analysed by Manugraphy (Figure 1). The manugrahy sytem consists of 3 cylinders covered with pressure sensor matrices. The cylinders had circumferences of 100, 150, and 200 mm, corresponding to 32, 48, and 64 mm diameters, respectively. The grip strength and the contact area of the affected hand were compared to the healthy opposite hand with regard to the median difference for three different cylinder sizes. In addition, the areal forces of seven anatomical areas of the hand (thumb, four fingers, thenar and hypothenar) were analysed. ResultsThe grip force of the affected hand was significantly reduced with 11-16% compared to the opposite hand for the 100 and 200 mm cylinder, and 4% for the 150 mm cylinder. The contact area between hand and cylinder was reduced by 5% (100 mm), 3% (150 mm) and 2% (200 mm) due to muscle atrophy (Figure 2). Analysis of the areal forces showed the most significant deficit in the middle and ring finger (Figure 3).
ConclusionAlthough the thumb and thenar are considered most severely affected by carpal tunnel syndrome, the force deficit was most severe in the middle and ring finger. This is probably caused by sensitive impairment and the fact, that the stabilisation of the thumb is affected by the carpal tunnel syndrome and therefore results in a reduced force transmission. 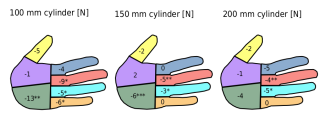
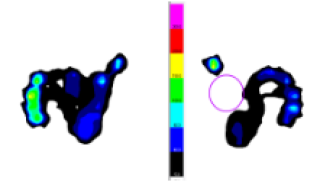

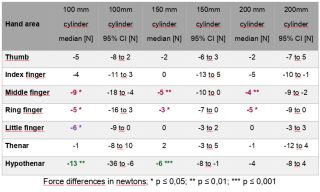
|
||
|
10:50–10:57
Association between Distal Radius Fractures and TFCC Injuries; The Frequency of such Injuries and their Role in Clinical Practice
Katarina Schär, Winterthur
AbstractBackgroundDistal radius fractures belong to the most common fracture type. Injuries to the triangular fibrocartilage complex (TFCC) can occur as an associated injury and are a predictor of a worse outcome. They are a cause of persistent (ulnocarpal) papin, decreased grip strength, and limited range of motion. In particular, the foveal insertion of the TFCC plays a crucial role in the stability of the distal radioulnar joint (DRUJ). AimsThere is still no unified guideline for the treatment of TFCC injuries. This presentation aims to draw attention to TFCC injuries, provide an overview, and offer possible treatment recommendations. MethodsThe PubMed database was searched using the keywords "distal radius fracture, TFCC." A total of 73 studies were identified in the past 10 years. Of these 73 studies, 19 were included in this review. ResultsThe majority of studies based solely on MRI diagnostics showed a prevalence of TFCC injuries ranging from 54% to 97%. Arthroscopy-based studies observed TFCC injuries in 17% to 90% of cases. Additionally, DRUJ instability was found in 26% of cases. Two studies described arthroscopy performed during follow-up. A reoperation was conducted due to ulnocarpal pain. Lesions of the TFCC were found in up to 80% of cases. ConclusionDiagnosis and treatment of distal radius fractures and TFCC injuries require careful consideration of the patient's individual needs and the selection of the most suitable treatment options to achieve optimal functional outcomes. Early diagnosis and tailored therapeutic approaches are essential for reducing the risk of chronic pain and functional limitations. Not every TFCC injury requires surgical intervention but an accurate diagnosis and the initiation of conservative treatment measures benefit the patient and improve postoperative care. Against this background, a protocol like the "WRIST" protocol (published by Goorens) could provide assistance in clinical practice. |
||
|
11:00–11:07
Carpal Tunnel Syndrome, Trigger Finger, and ATTR Amyloidosis: When Should a Biopsy be Performed?
Clara Marie Pecher, Zürich
AbstractBackgroundCarpal tunnel syndrome (CTS) and trigger finger (TF) may be early symptoms of transthyretin amyloidosis (ATTR), which can lead to cardiac involvement (CA) with heart failure, atrial fibrillation and bundle branch block within 5-10 years. Previous studies reported, 2.3 % to 34 % of ATTR positive biopsies in the context of carpal tunnel release. AimsThe data collected in our clinic in 2022 was low for ATTR positive samples compared to the literature. We are looking for the causes, re-analysing our patient population based on risk factors and aim to make recommendations on when to do a biopsy. MethodsOur previous data showed ATTR positivity in biopsies in 3 out of 34 patients (9 %) due to increased synovial tissue in carpal tunnel and A1 pulley release. In this paper re-analysis was performed for risk factors (RF) such as bilateral CTS or TF in men > 50 and women > 60 years. Results12 out of 34 patients fulfilled the RF of bilateral CTS/ TF and the defined age limits. 3 out of these 12 patients were ATTR positive (25 %). Other risk factors identified in the literature include spinal stenosis, distal biceps tendon rupture, hearing loss, atrial fibrillation, heart failure, cardiomyopathy (as sign of occult CA) and positive family history. In middle-aged and older patients, the ATTR wild-type (also known as senile systemic amyloidosis) is usually common, so that the incidence of the hereditary types was negligible. A specimen size of > 1 cm2 of synovia is recommended. ConclusionAnalysis by RF showed an ATTR positivity of 25 % like those in the literature. Amyloid deposition does not cause synovial proliferation, so biopsy should be performed in men > 50 and women > 60 years with bilateral CTS or TF. RF-based patient selection helps to diagnose ATTR amyloidosis early, specific and cost-effectively. |
||
|
PSGH31
11:10–11:17
3D-Planned Intraarticular Corrective Osteotomy of Malunited Bennett's Fracture Using Patient-Specific Guides: Clinical Outcomes and Postoperative Assessment of Reconstruction Accuracy
Arnaud Klopfenstein, Zurich
AbstractBackgroundMalunions of Bennett fractures can cause deformities and functional impairments. Intra-articular corrective osteotomy, though demanding due to the small fragment size, is the only reconstructive treatment. 3D planning and patient-specific guides can enhance accuracy and aid in such cases. AimsThis study evaluated the feasibility, post-op joint congruency, and functional outcomes of first metacarpal base corrective osteotomies using three-dimensional (3D) planning and 3D-printed patient-specific instruments (PSI). MethodsWe report outcomes of 14 patients who underwent corrective osteotomies at the base of the first metacarpal for malunited Bennett’s fractures. Computer-assisted 3D preoperative planning, using the contralateral hand as a template, facilitated the creation of 3D-printed patient-specific guides for intraoperative navigation. Articular step correction and reduction of first metacarpal subluxation were assessed on follow-up CT scans. In addition, clinical assessments, including range of motion (ROM), pain, and grip and pinch strength, were performed at 6 months or the final follow-up. Postoperative complications were also documented. Results14 patients (mean age 29.1 ± 11.9 years, range 14–56) underwent corrective osteotomy at the base of the first metacarpal, with a mean follow-up of 18.1 ± 16.8 months (range 2–60 months). Follow-up CT scans in 13 patients confirmed successful corrections, good joint congruency, and regular osseous consolidation. The mean articular step-off decreased significantly from 1.9 ± 0.4 mm preoperatively to 0.2 ± 0.1 mm postoperatively. One patient required revision surgery with a carpometacarpal (CMC) I arthrodesis due to screw cut-out. At 6 months or final the follow-up, ROM improved significantly, and strength returned to levels comparable to the contralateral side. ConclusionOur results suggest that precise reductions for corrective osteotomies of the first metacarpal base, following malunion of Bennett fractures, can be achieved using 3D planning and PSI. This technique also leads to significant clinical improvements and high patient satisfaction. |
||
|
11:20–11:27
Vascularized Composite Allotransplantation in Switzerland: from Bench to Bedside
Radu Olariu, Bern
DetailsBackgroundVascularized composite allotransplantation (VCA), such as hand and face transplants, offers reconstructive solutions for patients with severe tissue loss. However, the necessity for long-term systemic immunosuppression to prevent graft rejection poses significant risks, including opportunistic infections and metabolic disturbances, limiting the broader application of VCA. To address these challenges, our research group has investigated local immunosuppression strategies aimed at minimizing systemic drug exposure while effectively preventing graft rejection. AimsWe aim to present an overview of our research on localized drug delivery systems (DDS) that offer targeted immunosuppression within the graft site, thereby reducing systemic toxicity and enhancing graft survival, and provide an overview of clinical VCA experience worldwide. Material & MethodsOver the last 15 years we designed biomaterial-based DDS, including tacrolimus-loaded hydrogels and in situ forming implants, intended for local, on-demand immunosuppressive drug release. These systems were tested in preclinical models, such as rat hind-limb and porcine VCA models, to assess their efficacy in delivering high local concentrations of immunosuppressive agents while minimizing systemic exposure. We also provide an up-to-date overview of clinical VCA, focusing especially on hand transplantation. ResultsOur work demonstrated that local delivery of tacrolimus via DDS effectively prolonged graft survival in VCA models. Notably, the localized treatment reduced T-cell infiltration and neutrophil extracellular trap formation within the grafts while systemic drug levels remained low, suggesting a reduction in potential off-target toxicity. These findings support the feasibility of local immunosuppression to mitigate the adverse effects associated with systemic immunosuppression in VCA. ConclusionsThe Bern VCA research group's investigations into local immunosuppression strategies have shown promising results in preclinical models, indicating that targeted drug delivery systems can effectively prevent graft rejection while minimizing systemic toxicity. These advancements may pave the way for safer and more widespread clinical application of VCA and potentially first clinical cases in Switzerland. |
||
|
10:00 – 11:30
Room 5C
|
Swiss HPBA joins the SGVC: Advances in Hepatobiliary and Pancreatic surgery
Christian Toso, Geneva; Stefan Breitenstein, Winterthur
|
|
|
Main Session
|
||
|
10:00–10:05
Short presentation of the Swiss HPBA
Emmanuel Melloul, Lausanne
|
||
|
10:05–10:15
Minimal invasive pancreatic surgery: technical aspects
José Oberholzer, Zurich
|
||
|
10:15–10:25
Minimal inasive liver surgery: technical aspects
David Fuks, Lausanne
|
||
|
10:25–10:35
New trends in the surgical management of IPMN
Beat Müller, Basel
|
||
|
10:35–10:45
Management of the Liver cysts
Patryk Kambakamba, Winterthur
|
||
|
10:45–10:55
Echinococcosis: who needs surgery?
Severin Gloor, Bern
|
||
|
10:00 – 11:30
Room 4BC
|
The Surgeon: From Solo Performer to Team Leader, Risk Manager, and Self-Brand
Emilie Uldry, Lausanne; Valentine Luzuy-Guarnero, Geneva
|
|
|
Main Session
|
||
|
10:00–10:05
Introduction & Moderation
Emilie Uldry, Lausanne; Valentine Luzuy-Guarnero, Geneva
|
||
|
10:05–10:25
Teamwork: A-Team (of Surgery)
Nadine Bienefeld, Zurich; Nadine Diwersi, Obwalden
|
||
|
10:25–10:45
Failure in Surgery - Truth or Dare?
Valentin Neuhaus, Zurich; Jennifer Klasen, Basel
|
||
|
10:45–11:05
Self-Marketing: From Pokerface to Superhero!
Magdalena Biraima, Wetzikon; Christian Eugen Oberkofler, Zurich
|
||
|
11:05–11:30
Panel discussionAll speakers |
||
|
11:30 – 12:30
|
Lunch |
|
|
Break
|
||
|
11:35 – 12:15
Room 1C
|
Working Group: ForKids |
|
|
Main Session
|
||
|
11:35 – 12:15
Room 5C
|
Working Group: Pediatric Neurosurgery |
|
|
Main Session
|
||
|
11:35 – 12:15
Room 1B
|
Working Group: Pediatric UrologyVariaSuisse |
|
|
Main Session
|
||
|
12:30 – 14:00
Room 4BC
|
Bail-out procedures every acute care surgeon needs to know! – A case based session
Beat Schnüriger, Bern; Tobias Zingg, Lausanne
|
|
|
Main Session
|
||
|
12:30–12:52
The impossible gallbladder... what are my options?
Karolin Dallago, chur
|
||
|
12:52–13:14
Gastric perforation – What if I cannot suture the perforation?
François Pugin, Fribourg
|
||
|
13:14–13:36
Complex appendicitis – surgical approaches?
Dominique Lisa Birrer, Zurich
|
||
|
13:36–13:58
The abdominal wall cannot be closed – Now what?
Tobias Haltmeier, Bern
|
||
|
12:30 – 14:00
Auditorium B
|
BJS Session - Cultivating Excellence: A Fireside Chat with Rebecca Kraus and Ellen Petry Leanse
Martin Hübner, Lausanne; Rebecca Kraus, Chur
|
|
|
Main Session
|
||
|
12:30–12:35
First International Benchmark Values for Robotic Right Hepatectomy: A new standard of care?
Philip Müller, Basel
AbstractBackgroundRobotic liver surgery is rapidly emerging as the preferred surgical approach to the liver. Novel benchmark values in robotic surgery are urgently needed to enable conclusive comparisons with the standard open or laparoscopic approaches as well as with robotic surgery among different centers. AimsTherefore, this first multicenter study aimed to identify benchmark values for robotic right hepatectomies (RRH) based on a low-risk cohort treated at expert centers. MethodsThis multicenter study analyzed outcomes from consecutive patients undergoing RRH for malignant or benign lesions from 16 international expert centers from 2018 to 2024. Fifteen benchmark values were identified and compared to a published multi-national cohort series of laparoscopic and open right hepatectomy (RH). Benchmark patients were without significant comorbidities including portal hypertension, Child B cirrhosis, obesity (BMI >35kg/m2) cardiac disease, chronic pulmonary disease and renal failure. ResultsOf 352 patients, 192 (54.5%) qualified as benchmark cohort. The proportion of benchmark patients varied between 24%-100% per center. All benchmark values are disclosed in Figure 1. Benchmark values were defined for operative time (<480min), conversion rate (<0%), bile leak (<5.6%), CCI at 90-days (<20.9), hospital stay (<10 days) and readmission rate (<0%). Benchmark cut-offs showed a significant rate for 3-month overall complications (≤62.9%), but low rate of major complications (≤29.8%). RRH compared favorably to a multi-national cohort series of laparoscopic RH with lower conversion- (≤0% vs ≤13%) and R1 rates (≤0% vs ≤18%). Compared to the open approach, the benchmark cutoff for operation time was longer (≤480min vs ≤370min), however RRH showed lower values for major complications (≤45.5% vs ≤29.8%) and length of stay (≤9d vs ≤12d) (Figure 1). ConclusionThis first benchmark analysis sets novel reference values for RRH, indicating several favorable outcomes as compared to open RH. These references values may serve for quality control of surgery in centers embarking in RRH, and RRH may be expected to become the approach of choice in minimally invasive RH. 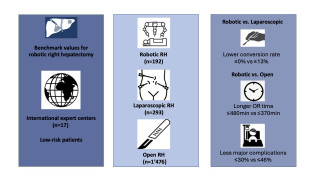
|
||
|
12:37–12:42
Lung volume reduction surgery reduces pulmonary hypertension in selected patients with emphysema
Bianca Battilana, Zurich
AbstractBackgroundLung volume reduction surgery (LVRS) provides benefit in survival, lung function, gas exchange and quality of life in patients with emphysema. Pulmonary hypertension (PH) is a late and serious complication in patients suffering from emphysema. Given the high-risk profile, LVRS remains controversial in this patient subgroup. AimsWe aim to present our institutional experience in performing LVRS in emphysema patients with PH. MethodsData was retrospectively collected from October 2002 until September 2024. We included patients with pre-and postoperative transthoracic echocardiogram (TTE) and/or right heart catheterization (RHC). We defined pulmonary hypertension (PH) as sPAP >35mmHg (TTE), mPAP ≥20mmHg (RHC) or other signs of pulmonary hypertension in TTE. We compared pre-and postoperative sPAP and forced expiratory volume in 1 second (FEV1) and analyzed the outcome. Results158 patients with COPD and PH underwent LVRS from October 2002–September 2024. Our cohort consists of 68 (43%) female patients with a median age of 67 [IQR 62-73]. 50 (32%) patients had homogeneous, 104 (66%) heterogeneous and 4 (2%) intermediately heterogeneous patterns of emphysema. 72 (46%) patients had an estimated sPAP >35mmHg in the preoperative TTE, 46 (29%) patients presented with mPAP ≥20mmHg during RHC, 40 (25%) patients showed signs of PH in the TTE. The sPAP (TTE) decreased significantly from 43.5mmHg [IQR 39-50] preoperatively to 39.5mmHg [IQR 35-44.25, p=0.0138] postoperatively, independent of emphysema type. These patients also had an improvement in FEV1 from 710ml [IQR 560-860ml] preoperatively to 845ml [IQR 687.5-1160ml, p<0.0001] postoperatively. The 30-day mortality was 2 (1%), and the median overall survival was 37.44 months [IQR 17.49-64.89]. ConclusionLVRS can lead to significant reduction of PH and improvement in lung function for patients with all emphysema types. Therefore, PH should not be an exclusion criterion per se and patients being equally assessed in a specialized institution. 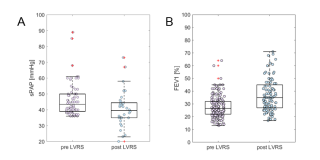
|
||
|
12:44–12:49
Pilot open randomized controlled trial comparing patients undergoing robotic gastric bypass with or without concomitant cholecystectomy
Marie Burgard, Geneva / Fribourg
AbstractBackgroundPatients experiencing rapid weight loss after bariatric surgery are at high risk of developing gallstones. However, the necessity of performing a concomitant cholecystectomy along with Roux-en-Y Gastric Bypass (RYGB) remains debated. Concerns over higher complication rates lead many surgeons to avoid performing concomitant cholecystectomy, particularly in patients without gallbladder pathology. AimsTo compare outcomes between patients without cholelithiasis undergoing RYGB with and without concomitant cholecystectomy. MethodsWe conducted a pilot prospective open randomized study from 2018 to 2023 involving patients without gallstones who underwent RYGB either without concomitant cholecystectomy (control group) or with concomitant cholecystectomy (study group). Follow-up occurred during hospitalization and at 1, 3, 6, 12, and 18 months. The primary composite outcome was intraoperative adverse events (iAEs) and postoperative complications (Clavien-Dindo classification). Secondary endpoints included detailed iAEs and postoperative complications, biliary outcomes, operation duration, length of hospital stay, and quality of life (QoL). ResultsA total of 95 patients were included in the study. Demographics were similar between groups. There was no statistically significant difference in the composite outcome of intra- and postoperative complications between the control and study group (24.4% vs. 42%, p = 0.083). Detailed iAEs, postoperative complications according to Clavien-Dindo, length of hospital stay, operation duration, and QoL at 1 and 12 months were similar, while the study group showed a higher early comprehensive complication index (mean CCI of 2.10 vs. 6.09, p = 0.047). The incidence of biliary complications during follow-up was 6.8% in the control group and 2.0% in the study group, with 4.5% of patients receiving biliary interventions in the control group. ConclusionWhile overall intra- and postoperative complications did not significantly differ, patients experiencing concomitant cholecystectomy showed a higher early complication index. The incidence of subsequent biliary interventions was low in this patient cohort without preexisting cholelithiasis. |
||
|
12:51–12:56
Return to Intended Oncologic Treatment (RIOT) After Surgical Resection of Oligometastatic Non-Small Cell Lung Cancer.
Raphael S. Werner, Zurich
AbstractBackgroundIn oligometastatic Non-Small Cell Lung Cancer (NSCLC) combining systemic and local ablative treatments, including lung resection or radiotherapy, has been shown to improve survival. Maintaining continuity in systemic therapy is crucial in metastatic disease, making the time to Return to Intended Oncologic Treatment (RIOT) after surgery a promising oncologic outcome parameter, which has not yet been investigated in oligometastatic NSCLC. AimsWe aimed to assess whether an early RIOT after anatomical lung resection is associated with improved survival. MethodsWe retrospectively analyzed patients with synchronous oligometastatic NSCLC (≤5 metastases in ≤3 organs) diagnosed between 2004 and 2024 who underwent anatomical resection of the primary tumor and were planned for adjuvant oncologic treatment. RIOT was defined as the interval between surgery and the first dose of adjuvant treatment. Predictors of overall survival (OS) and recurrence-free survival (RFS) were assessed by multivariate Cox regression. ResultsThirty-six patients were analyzed; 58% were female and the median age was 60.0 [53.0–67.0] years. Despite stage IV disease, 61% of lung resections were performed minimally invasive (42% VATS, 19% RATS). Median RIOT was 36.0 [27.0–56.3] days and ROC analysis identified 41.5 days as the cut-off to discriminate recurrence. Patients returning to oncologic treatment within 42 days had significantly improved RFS compared to those with delayed RIOT (44.0 [18.0–101.0] vs. 14.0 [5.0–31.0] months, p=0.012) (Figure 1). In the multivariate Cox regression model, RIOT was identified as an independent predictor of RFS (HR 2.55, 95% CI 1.04–6.27, p=0.042). ConclusionRIOT appears to be a valuable predictor for RFS in patients with synchronous oligometastatic NSCLC who undergo anatomical lung resection as part of the multimodality treatment approach. These findings emphasize the importance of minimally invasive surgery and the implementation of enhanced recovery after thoracic surgery (ERATS) protocols to facilitate a timely RIOT in this patient population. 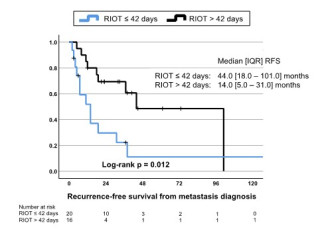
|
||
|
12:58–13:03
Trends and Perioperative Outcomes in Gastric Cancer Surgery in Switzerland: A National Inpatient Database Analysis (1998–2021)
Joël Gerber, Bern
AbstractBackgroundVolume–outcome relationships have driven the implementation of minimum case volume regulations for various surgical procedures under the framework of Highly Specialised Medicine (HSM) in Switzerland. However, the regulation of gastric oncological resections remains a subject of debate. AimsTo analyse volume–outcome relationships for oncological resections in gastric cancer patients in Switzerland. MethodsA nationwide analysis of an inpatient database (Medical Statistics of Hospitals) from the Swiss Federal Statistical Office was conducted. Diagnoses and related health problems were coded according to the International Classification of Diseases, 10th Revision (ICD-10), and diagnostic and surgical procedures using the Swiss Classification of Operations (CHOP). Patients with gastric cancer undergoing surgical or endoscopic resection from 1998 to 2021 were identified. Data were stratified by annual surgical caseload (quartiles), hospital typology, and annual inpatient volume. Outcomes included in-hospital mortality, postoperative complications, and failure-to-rescue (FTR) rates. ResultsA total of 8708 cases from over 30 million hospitalisations were included. Yearly caseload increased over time (2000: 255; 2010: 383; 2020: 432). Overall mortality was 3.8%. Higher surgical caseload was associated with lower mortality (2.2% for centres with >20 annual gastric cancer surgeries vs. 2.6–4.5% for lower quartiles, p = 0.001), as were annual inpatient volume (2.3% vs. 4.1–5.0% with a threshold of 30,000 annual inpatient cases, p < 0.001), and hospital typology (1.9% for university hospitals vs. 4.2–4.1% for centrum/other hospitals, p < 0.001). While hospitals with higher caseload reported relatively more complications, including anastomotic leaks and peritonitis, the associated FTR rates were lower (10.8% vs. 12.3–25.0% with 20 annual gastric resections as the cut-off, p < 0.001). ConclusionThe results indicate that patients who underwent gastric cancer surgery in hospitals with higher case volumes – both surgical and inpatient – experienced lower in-hospital mortality and reduced failure-to-rescue rates. |
||
|
13:05–13:10
Repeated Anatomical Pulmonary Resection for Second Primary Non-Small Cell Lung Cancer: Safety, Feasibility and Short-Term Outcomes
Céline Forster, Sion
AbstractBackgroundAdvances in non-small cell lung cancer (NSCLC) management have extended survival rates, contributing to a higher incidence of second primary NSCLC (2-20%). Repeated anatomical pulmonary resection in these cases poses significant technical challenges and functional limitations due to previous surgery. AimsThis study evaluates the feasibility and short-term outcomes of repeated anatomical pulmonary resections for second primary NSCLC. MethodsWe retrospectively reviewed all consecutive cases of repeated anatomical pulmonary resections for second primary NSCLC performed in our institution from January 2014 to December 2023. Clinical-pathological characteristics, postoperative complications, and oncological outcomes were analyzed. ResultsA total of 55 patients (median age 68 years [IQR: 61.5-72]) underwent repeated anatomical pulmonary resections for second primary NSCLC (figure 1). Adenocarcinoma predominated in both primary (78.2%) and secondary (76.4%) cases. Video-Assisted Thoracoscopy (VATS) approach was used in 94.5% and 96.4% after first and repeated resection, respectively (p=0.647). The extent of pulmonary resection differed between first and second resection, with a predominance of lobectomy during first resection (56.4%) and segmentectomy during second resection (85.5%, p<0.001). We did not observe any significant difference in postoperative overall morbidity after first and second resection (23.6% vs. 40%, p=0.065). However, there was a significant increased incidence of cardiac complications (16.4% vs. 0%, p=0.007) and prolonged air leak (>5 days) after second resection (14.5% vs. 0%, p=0.014). The median length of hospital stay was similar after first and repeated resection (5 vs. 5 days, p=0.089) and the duration of chest drainage was marginally increased after the second surgery (2 vs. 1 day, p=0.065). Three-year overall survival after primary resection was 89%. Recurrence was documented in one patient (1.8%) after first resection and two patients (3.6%) after second resection (p=0.558). ConclusionOur series demonstrated that second primary NSCLC can be safely managed by VATS segmentectomy, yielding favorable short-term survival and low recurrence rate. 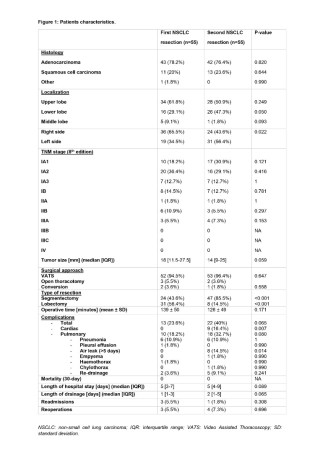
|
||
|
13:10–13:55
BJS Lecture
Ellen Petry Leanse, Santa Fe, New Mexico US
|
||
|
13:55–14:00
BJS Award Distribution |
||
|
12:30 – 14:00
Room 4A
|
Education
Emmanuel Melloul, Lausanne; Karoline Horisberger, Mainz DE
|
|
|
Free Communication
|
||
|
12:30–12:37
The Burden of Unwanted E-mails in Academic Surgery
Lorenzo Bernardi, Lugano / Lausanne
AbstractBackgroundUnwanted e-mails (UEM) constitute a futile burden for academic surgeons. However, data investigating the magnitude of this concern and its determinants are lacking. AimsTo assess the burden of UEM in academic surgery and to identify factors associated with a high burden of UEM. MethodsThis was a prospective cross-sectional study conducted in a division of visceral surgery of a tertiary center, between May 1-31, 2024. Participants included physicians of the division; UEM received in the institutional e-mail box by the participants during the study period were collected and examined. ResultsParticipants included 36 physicians: 13 residents, 14 fellows and 9 consultants. A total of 2934 UEM were examined; among them, 1707 (58.2%) solicited scientific contributions, including invitations to submit manuscripts (n=910, 31%). Number of UEM per participant was heterogenous, ranging from 0 to 601, with a median of 16 (0-106). The latter also showed differences between residents 0 (0-1), fellows 34 (5-70), and consultants 147 (101-402) (p<0.001). Finally, high burden of UEM was associated with surrogates of experience and research activity, such as age (OR, 1.21; 95% CI, 1.04-1.41; p=.011), board certification in visceral surgery (OR, 11.50; 95% CI, 2.01-65.91; p=.006), number of peer-review publications (OR, 1.12; 95% CI, 1.01-1.24; p=.027) or H-index (OR, 1.36; 95% CI, 1.07-1.73; p=.012). ConclusionUEM represent a major burden for academic surgeons. Exposure to UEM varies proportionally to professional experience and research activity. |
||
|
12:40–12:47
Future Demand for Visceral Surgeons in Switzerland: An Empirical Study
Hans Grossen, Frauenfeld
AbstractBackgroundSwitzerland’s aging population and evolving healthcare demands are expected to increase the need for specialized surgeons. Meanwhile, ongoing discussions about reduced working hours for residents and a growing trend toward minimally invasive and outpatient procedures may influence training opportunities and inpatient procedural volumes. AimsThe aim of this study was to evaluate workforce, training, and procedural volumes in surgery to predict the future demand for visceral surgeons in Switzerland. MethodsThis study analysed national datasets from 2009 to 2023 to assess trends in medical school enrolments, recognised medical diplomas, residency positions, and the availability of general and visceral surgeons. Additionally, surgical procedure volumes were evaluated, with a particular focus on pancreatic surgery as a proxy for complex cases. Linear regression models projected developments up to 2040, incorporating Swiss population growth forecasts. ResultsThe number of medical diplomas - both Swiss-issued and foreign-recognized - showed an increase from 2’725 in 2011 to 4’647 in 2023. Projections indicate a further rise, reaching over 6,000 by 2040. The overall pool of general surgeons increased from 1’127 in 2009 to 1’557 in 2023, with the proportion of women rising from 10.6% to 24.9% in the same interval. Visceral surgeons numbered 303 by 2023 (11% female), and forecasts suggest a 50% increase to approximately 462 by 2040. Pancreatic surgery cases grew by 14.5% between 2016 and 2023 and are projected to increase by an additional 25% by 2040. However, the number of surgeries per visceral surgeon is projected to decline steadily over the next years. ConclusionThe projected expansion of the surgical workforce seems to overcompensate for the growth in Switzerland’s population. In combination with a shift towards outpatient care and reduced working hours, procedural exposure could become critical in visceral surgery. Ensuring that training pathways and practice models adapt to these evolving demands will be vital to maintaining high standards of surgical care. |
||
|
12:50–12:57
Automatic Identification of Teamwork Behaviors in the Operating Room
Lilien Schewski, Bern
AbstractBackgroundAccurate identification of intraoperative behaviors is crucial for assessing surgical performance, improving patient outcomes, and supporting surgical training. Traditional methods for evaluating intraoperative behaviors rely on experts' on-site observations or assessments of video recordings. Although these methods have been shown to be reliable, they are time-consuming, prone to bias, and limited in scalability. Video recordings of the operating room (OR), combined with methodological advancements in computer vision and machine learning, offer promising opportunities for automated, objective, and scalable behavior analysis. AimsThis study explores the feasibility of automated approaches for assessing teamwork-related intra-operative behaviors in the OR. In a stepwise approach, we aim to automatically: 1) detect the positions and poses of the OR team members, 2) analyze movements and distribution patterns of the OR team, 3) determine their roles and functions, and 4) recognize structured team communication (e.g. team timeouts, briefings). MethodsA multi-view OR dataset with over 100 hours of video recordings was created at a Swiss university hospital, featuring annotations of team interactions during real surgical procedures. Using deep learning-based video techniques, a multidisciplinary team of work psychologists, computer scientists, and surgeons detects and analyzes key events of interest. ResultsA framework for automatic video analysis was developed and validated using the created dataset. The experimental results show that our framework provides a valuable and efficient alternative to existing state-of-the-art approaches for both surgical role classification and team communication detection tasks. ConclusionWe present a novel pipeline that automatically classifies the roles of the OR team members and detects behavioral team interactions. This work highlights the potential of automated approaches to revolutionize surgical practice and education by providing scalable, objective insights into non-technical skills. |
||
|
13:00–13:07
Development of DocNote: A Tool that Automatically Generates Structured Medical Reports to Reduce Administrative Workload and Enhance Doctor-Patient Interactions
Alice Gilson, Geneva / Genève
AbstractBackgroundEfficient reporting of medical consultations is a persistent challenge in healthcare, with traditional methods such as manual note-taking and dictation tools often leading to inconsistent report quality and interruptions in doctor-patient interaction. To address this, we developed DocNote, an application that generates structured medical reports from audio recordings using cutting-edge speech-to-text and natural language processing (NLP) technologies. DocNote aims to accelerate admin tasks, improve report quality, and enable physicians to focus more on patients during consultations. AimsThis work presents the design and development of DocNote, emphasizing its innovative features and potential contributions to medical practice. MethodsInterviews and surveys with physicians identified pain points in reports accuracy and user experience. The tool underwent iterative prototype testing in clinical settings, with feedback driving refinements. ResultsDocNote employs local audio recording, followed by speech-to-text conversion using advanced natural language processing (NLP) algorithms to transcribe conversations into structured text. Then, we use state of the art Generative Pre-trained Transformers models, trained on medical data, to generate the most accurate report, respecting specialized medical jargon. The application enables standardization through customizable templates, automatically formatting reports into predefined layouts to follow local requirements. Reports are stored locally and securely sent to physicians’ professional email, ensuring compliance with privacy regulations. Ethical considerations include patient consent for recordings, confidentiality through local storage and secure transmission, and hosting on Swiss servers. As DocNote is not classified as a medical device, physicians must review and validate reports before signing. Implementation challenges, such as ensuring transcription accuracy in noisy environments and addressing linguistic nuances, were overcome through collaboration among developers, physicians, and security experts. ConclusionDocNote offers a novel approach to medical reporting, reducing administrative burdens and enhancing report quality while improving doctor-patient interactions. This study highlights how collaborative, user-centered innovation can address longstanding challenges in healthcare. Future studies will assess the tool’s real-world impact on medical practice. 
|
||
|
13:10–13:17
The Avian Model as a Versatile and Cost-Effective Tool for Surgical Training Across Specialties
Alessia Allasia, Lausanne
AbstractBackgroundFive years after its 2019 validation, the avian tissue model for neonatal minimal access surgery (MAS) training was reassessed to evaluate its sustained effectiveness and realism. Unlike the original study, this evaluation included participants from paediatric and other surgical specialties.
AimsThe study aimed to reassess the model’s realism and effectiveness for neonatal MAS training and explore its potential for broader applications in surgical training. MethodsThe study occurred during two events: an international MAS Skills Lab in August 2024 and a national MAS Skills Lab in September 2024. Twenty-six participants (16 females, 10 males) took part, including 17 paediatric surgeons and 9 from other specialties. Using 3 mm MAS instruments on fresh chicken cadavers with balloon trocars, participants performed laparoscopic exercises such as adhesiolysis, cholecystectomy, and intestinal anastomosis. Feedback on the model was gathered via a 5-point Likert scale (MiSSES). ResultsParticipants had varied experience levels: 23% had performed over 100 MAS cases, 15.4% between 50–100 cases, and 61.5% fewer than 50 cases. The model’s perceived realism averaged 4.05 ± 0.10. Scores for specific features included 3.66 ± 0.09 for the abdominal wall, 3.85 ± 0.10 for the abdominal cavity, and 4.86 ± 0.09 for tissue dissection. Participants rated the model highly for improving laparoscopic knowledge (4.3 ± 0.90) and skills development (4.77 ± 0.07). Satisfaction scores highlighted its effectiveness in addressing challenges like trocar placement (3.64 ± 0.12), pneumoperitoneum (3.5 ± 0.10), and confined-space suturing (4.99 ± 0.08). Overall satisfaction with the model was rated at 4.9 ± 0.09. ConclusionThe avian tissue model remains an effective and realistic tool for neonatal MAS training, reaffirming the findings of the 2019 study. Positive outcomes across multiple disciplines demonstrate its versatility, highlighting its potential as a valuable training tool extending beyond paediatric surgery to other specialties. |
||
|
13:20–13:27
Gender disparities on editorial boards of digestive surgery and gastroenterology journals: a focus on H-index and journal impact factor
Elin Meyer, Genève
AbstractBackgroundDespite a steady increase in the number of women trained in medicine, their representation remains significantly low at the head of department level, particularly in surgery. This disparity extends to academic careers. AimsThis study aimed to determine if gender plays a role in the composition of editorial boards. MethodsSurgical (digestive and general surgery) and gastroenterology journals were selected for inclusion from the Clarivate database. Editorial board Data for these journals were extracted from searches on open-source websites. The H-index of editors-in-chief was obtained via Google Scholar and Scopus. Journal Impact Factors were found on Clarivate InCites 2023. ResultsOf 2’542 editorial board members from 124 journals included for analysis, 18% of all editors (456/2542) and 10% (16/155) of editors-in-chief were women. No difference was found in editorial board composition across journals by specialty. The proportion of female editorial board members increased significantly with the journal impact factor (p<0.05). The average H-index of male editors-in-chief was 56.69, whereas it was 38.13 for female editors-in-chief (p<0.05). ConclusionWomen are significantly underrepresented on surgical journal editorial boards, particularly in leadership positions such as editor-in-chief. While this disparity improves in high-impact journals, journal speciality has no apparent influence on composition. Differences in H-Indexes do not explain this disparity at editor-in-chief level. |
||
|
13:30–13:37
Impact of Ergonomic Microbreaks for Surgeons: A Systematic Review
Gabriel Heierli, Lausanne
AbstractBackgroundSurgeons face a risk of work-related musculoskeletal disorders (WMSDs). Repetitive movements and poor ergonomic conditions cause pain, particularly in the back, neck, arms, and shoulders. WMSDs not only impact surgeons' quality of life but also affect surgical performance, absenteeism, and healthcare costs. Intraoperative microbreaks (MBs) with active stretching exercises have been proposed to reduce WMSDs, fatigue, and to improve performance. AimsThe aim of this review is to study the effects of ergonomic intraoperative microbreaks and to define the most efficacious intervention (length of MBs, interval duration, specific stretching exercises). MethodsA systematic review of clinical trials evaluating physical or psychological impacts of microbreaks on surgeons, with a control group, was conducted in MEDLINE, Embase and Google Scholar from September to October 2024. Outcomes of interest included pain, discomfort, fatigue, dexterity, mental focus, and stress. ResultsTen clinical trials were retained for final analysis (8 crossover trials and 2 randomized controlled trials), for a total of 284 participants. Methodology and assessed outcomes varied considerably between studies. 6 out of the 10 trials showed at least one improved outcome with the implementation of microbreaks. The most frequently assessed outcomes were pain and discomfort (improved in 5/8 studies), mental focus (improved in 3/3 studies), and accuracy (improved in 1/3 studies). Five studies evaluated operative duration, all showing that microbreaks did not prolong the overall time. No specific duration, interval, or set of exercises was identified as the most effective approach for microbreak implementation. ConclusionMost of the studies included show that microbreaks appear to have a positive impact on surgeons’ well-being and performance. There is a need for standardization of interventions and outcome measures. The long-term effects of microbreaks remain yet to be studied, and more data is also required to identify the most efficacious intervention. |
||
|
13:40–13:47
From Observer to Contributor: How Do our Trainees Perceive their Tumor Board Participation?
Alecsandra Tudor, Lausanne / Bern
AbstractBackgroundTumor boards are an integral part of modern medical practice, fostering multidisciplinary collaboration, however little is known about how trainees perceive their participation, how it benefits their training, or how they evolve into active contributors by the end of their training. Understanding these questions is essential for optimizing the educational value of tumor boards for future specialists. AimsThis study aims to explore the experiences of trainees with thoracic tumor boards, to better understand their needs and thus help in improving the learning curve. MethodsUsing a constructivist paradigm and qualitative descriptive methodology, we interviewed trainees from thoracic surgery and pulmonology using an interview guide with open-ended questions. Data sufficiency was attained after six interviews. We used thematic analysis on the verbatim transcriptions to extract relevant themes capturing their experiences. ResultsWe identified six main themes: (1) "The formal and standardized structure", which gives the trainees reassurance, as they can hold on to something familiar and relatable; (2) "Watching a play", portraying the feeling of being a passive observer; (3) "Being in a tornado", suggesting the gap in understanding, and rapid flow of information; (4) "The experts who already have the answer", highlighting the daunting nature of becoming an active participant; (5) "Struggling with the pace and information quantity", reflecting being overwhelmed with the complexity of tumor boards; and (6) “Losing the thread and feeling it’s a waste of time”, which implies that quantity without quality is noticeable and undesirable. ConclusionTrainees frequently struggle to understand and engage in tumor boards, often feeling like passive spectators in a complex, unfamiliar environment. These challenges impact their motivation and hinder the learning process. To improve trainee involvement, enhance their learning experience, and better prepare them for active participation in multidisciplinary care, educational interventions should be tailored based on real world information and the local context. |
||
|
13:50–13:57
Effectivity of Peer-assisted learning in training of basic surgical skills for medical students: A monocentral study with 81 medical students in Switzerland.
Emilie Houdebert, Lausanne
AbstractBackgroundAcquiring basic surgical skills is a critical component of a physician's training, yet many medical students graduate with insufficient to none surgical competencies in suturing. AimsThis study investigated the effectiveness of peer-assisted learning on suturing skill progression and its influence on students’ engagement with surgery. MethodsData were collected as part of an ongoing prospective study (2023–2024) conducted in Lausanne, Switzerland. second to fifth year medical students attended three 2-hour suturing courses (e-learning and hands-on). They were required to record videos of their suturing performance and complete self-assessments at the beginning and end of the program. Videos were evaluated by surgeons using the OSATS scale with a minimal score of 1 point and a maximal score of 5 points. Multivariable linear regression was performed to identify independent predictors of progression. ResultsA total of 81 medical students (mean age: 24.5 ± 2.4 years; 59 % women) completed the study. Participants demonstrated significant skill improvement across all evaluated domains after the 3 suturing courses. With an average progression of 0.850 points out of five (p-value < 0.0001), the greatest improvement was observed in instrument handling (average progression 1.020 points, t-test 11.4, p-value < 0.0001), while the smallest improvement was noted in tissue handling (average progression 0.519, t-test 6.9, p-value < 0.0001). On multivariable analysis, progression was positively associated with age (coefficient 0.11; 95% CI: [0.009; 0.214], p-value: 0.033) and perceived competence in suturing (coefficient 0.29, 95% CI: [0.049; 0.538], p-value: 0.020). However, prior attendance at a suturing course and self-reported perception of improvement (coefficient -0.465, 95% CI: [-0.923; -0.007], p-value 0.047, and coefficient -0.369, 95% CI: [-0.701; -0.037], p-value 0.030, respectively). were negatively associated with progression. ConclusionPeer-assisted learning is an effective approach for teaching basic suturing skills to medical students, Demonstrating measurable improvements in technical performance after participating in a 6-hours suturing course. |
||
|
12:30 – 14:00
Room 1A
|
Guardians of the Scalpel: Securing excellence in peripheral artery disease treatment
Elisabeth Côté, Lausanne; Edin Mujagic, Basel
|
|
|
Guardians of the Scalpel
|
||
|
12:30–12:40
Debate: Treatment of common femoral arteryOpen surgery first
Thomas Lattmann, Winterthur
|
||
|
12:40–12:50
Debate: Treatment of common femoral arteryEndovascular first
Giorgio Prouse, Lugano
|
||
|
12:50–13:00
Debate: Treatment of common femoral arteryDiscussion |
||
|
13:00–13:10
The role of IVUS in BTK treatment
Céline Deslarzes-Dubuis, Lausanne
|
||
|
13:15–13:25
When to do a distal bypass in 2025?
Stephan Engelberger, Baden
|
||
|
13:30–13:40
Debate: complex occlusive aorto-iliac lesionsAortobifemoral bypass first
Daniel Danzer, Sion
|
||
|
13:40–13:50
Debate: complex occlusive aorto-iliac lesionsComplex endovascualr reconstructions first
Michel Bosiers, Bern
|
||
|
13:50–14:00
Debate: complex occlusive aorto-iliac lesionsDiscussion |
||
|
12:30 – 14:00
Room 1C
|
Guardians of the Scalpel: Securing excellence through collaboration in pediatric urology
Olivier Sanchez, Lausanne; Enrico Broennimann, Lausanne
|
|
|
Guardians of the Scalpel
|
||
|
12:30–12:50
Presentation Varia Suisse
Uchenna Kennedy, Zurich; Norma Ruppen-Greeff, Zurich; Maike Nelissen, Basel
|
||
|
12:50–13:10
Sharing is Caring: Multi-Institutional Collaboration for primary surgery and subsequent care of patients with bladder extrophy epispadias complex
Jacques Birraux, Geneva; Martina Frech-Dörfler, Basel; Maya Horst Lüthy, Zurich; Olivier Sanchez, Lausanne
|
||
|
13:10–13:25
Communication Up in the Sky: Key to Success
Cédric Gaillard, Lausanne
|
||
|
13:25–13:50
Panel discussion
Laura Zaccaria, Biel; Loredana D'amato Sizonenko, Geneva; Anthony de Buys Roessingh, Lausanne
|
||
|
13:50–13:55
Urological outcomes of 5-year old patients after open prenatal spina bifida aperta repair
Antonin Prouza, Zurich
AbstractBackgroundNeurogenic lower urinary tract dysfunction (NLUTD) is a severe and frequent burden in patients with spina bifida aperta (SBA). Less than 10% of patients with postnatal SBA repair achieve normal bladder function (NBF) by the typical toilet training age. AimsThis study aimed to assess if open prenatal spina bifida aperta repair (OPSBAR) improves urological outcome at age five, when most healthy children have bladder control. MethodsPatients undergoing OPSBAR at our institution are followed prospectively in a standardized way, with data collected in a REDCap registry. We reviewed urological outcome data at age five, including bladder diary, urodynamic and ultrasound findings, need for clean intermittent catheterization (CIC) and anticholinergics. NBF was defined as age-appropriate voiding patterns in a bladder diary, age-appropriate bladder capacity, absence of detrusor overactivity, leakage or pressure increase during filling, normal detrusor contractility, absence of detrusor-sphincter-dyssynergia, and voiding without significant residual urine. Results22% (20/91) of patients showed a NBF, all exhibited spontaneous micturition. 60% (12/20) were fully continent, 30% (6/20) required night-time diapers, and 10% (2/20) were not yet fully toilet trained and used diapers during the day. 78% (71/91) had NLUTD, with 19% (17/91) developing NLUTD related to inclusion cysts. CIC was performed by 70% of patients (64/91), and 45% (41/91) required anticholinergic therapy, all of whom also performed CIC. A subgroup analysis showed a higher percentage of NBF in patients operated on after 2017 (35% vs. 12%, p<0.05), correlating with a significant decreased incidence of inclusion cysts. ConclusionAfter OPSBAR, 22% of patients exhibit NBF by age five, increasing to 35% for those operated on after 2017. Compared to postnatal SBA repair, this represents a significant improvement in urological outcome. |
||
|
13:57–14:02
Pediatric Robot-Assisted Partial Nephrectomy With Intraoperative Indocyanine Green: A Report of Two Cases
Roberto Carulli, Bellinzona
AbstractBackgroundIn recent years, innovative technologies have been introduced to improve the outcomes of robot-assisted partial nephrectomy (RAPN). Among these, indocyanine green (ICG) has been proposed to assess intraoperative kidney perfusion in the pediatric population AimsTo report our experience with ICG-guided RAPN and evaluate its role in performing partial nephrectomy in pediatric patients. MethodsWe retrospectively analyzed data from two pediatric patients who underwent RAPN at our center in 2024 for non-functioning upper poles in duplex renal systems. Both patients underwent preoperative MAG3 scintigraphy to evaluate residual renal function. During surgery, ICG was administered intravenously at a dosage of 0.2–0.3 mg/mL/kg. The da Vinci Xi robotic platform, equipped with the Firefly fluorescence imaging system, enabled real-time switching to near-infrared fluorescence (NIRF) imaging for visualization of the target organs. ResultsThe study included one male and one female patient, with a median age of 2 years. Both procedures were completed without conversion to laparoscopy or open surgery. No adverse reactions to ICG, including allergies or anaphylaxis, were observed. The use of NIRF imaging allowed clear delineation of functional and non-functional renal segments, facilitating precise resection. Follow-up confirmed preservation of residual renal function in both patients. ConclusionOur experience suggests that intraoperative ICG administration is a valuable tool for guiding surgeons in assessing functional renal moieties in pediatric duplex kidneys. Additionally, this technique may help shorten the learning curve for young surgeons adopting pediatric robotic surgery. Further studies with larger patient cohorts are required to validate these findings |
||
|
14:04–14:09
Posterior Urethral Valves – an Underestimated Cause for Lower Urinary Tract Symptoms in Older Boys?
Vivienne Sommer, Basel
AbstractBackgroundPosterior urethral valves (PUV) are the main cause for lower urinary tract obstruction in boys and still 17% of cases end up in end-stage renal disease once in their life. Most cases are detected prenatally or in early childhood, but up to one third of the patients are diagnosed later. We present a series of older boys with lower urinary tract symptoms caused by PUV. AimsThe aim of this analysis is to show a correlation between persistent lower urinary tract symptoms and PUV in older boys. MethodsRestrospective analysis of all boys older than 8 years, who underwent diagnostic cystoscopy for persistent lower urinary tract symptoms (i.e incontinence of different severity, voiding disorders or urinary tract infections) from January 2023 until December 2024. Indication for cystoscopy was made after unsuccesful conservative treatment. PUV were defined as narrowing of the urethra at typical localization of at least 30%. ResultsA total of 23 boys older than 8 years underwent diagnostic cystoscopy during January 2023 and December 2024 due to unsuccesful conservative treatment of lower urinary tract symptoms. In 22 of these boys, PUV were detected and treated. In 13 patients, symptoms resolved completely within the first 6 months. There was no improvement of symptoms in 3 patients. In the rest (6 patients), a partial resolution of symptoms could be seen. ConclusionPUV are an underestimated cause of LUTS in older boys. Therefore, cystoscopy should be considered in patients with unsuccesful conservative treatment.
|
||
|
12:30 – 14:00
Room 5C
|
How I do it?
Vanessa Banz, Bern; Alessandra Cristaudi, Lugano
|
|
|
Free Communication
|
||
|
12:30–12:37
Robotic-assisted Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (CRS and HIPEC) – Case Report and Video Demonstration of Surgical Technique
Lara Studerus, Basel
AbstractBackgroundCytoreductive Surgery (CRS) with or without hyperthermic intraperitoneal Chemotherapy (HIPEC) is the preferred treatment of peritoneal carcinomatosis of various cancer types such as ovarian, gastric or colorectal cancers. Usually, these often complex procedures are performed using an open approach. In patients with limited peritoneal cancer index or in the prophylactic setting according to recent studies, minimally invasive techniques are possible. Robotic-assisted CRS and HIPEC - first described in 2019 - has not yet found its way into daily practice. Case presentationA 63-year-old male patient presented with anemia and abdominal pain. Further investigation revealed a cT4 adenocarcinoma of the cecum without distant metastasis. Multidisciplinary tumorboard recommended prophylactic CRS including right hemicolectomy, right parietal peritonectomy, omentectomy and HIPEC according to results of the recent HIPECT4-trial. We performed robotic-assisted CRS and HIPEC as follows (video sequences): (1) right parietal peritonectomy from right inguinal region to hepatic flexure, (2) inferior approach of right hemicolectomy, mobilization of right hemicolon and small bowel until Ligament of Treitz and Pancreas including Gerota’s fascia, (3) complete omentectomy until small gastric vessels, omentum is left at hepatic flexure, superior mobilization of transverse colon entering lesser sac, (4) central ligation of ileocolic vessels, (5) dissection of transverse colon and distal ileum, en-bloc removal of the specimen via Pfannenstiel laparotomy (6) intracorporal side-to-side anastomosis, closure of mesentery, (7) placing of HIPEC tubes, (8) hyperthermic (41-43°C) chemotherapy (Mitomycin C) for 90 minutes, (9) rinsing of the abdomen (saline) and closing of incisions. Postoperatively, the patient was monitored for one night at the Intermediate Care Unit. Discharge was at day 7 after surgery. Adjuvant chemotherapy was given for 6 months. Until today, no recurrent disease has been diagnosed. ConclusionRobotic-assisted surgery is gaining importance in the surgical treatment of cancer. Using the advantages of a robotic approach such as improved dexterity, better 3D visualization and increased precision could also improve outcomes in cytoreductive surgery and HIPEC. |
||
|
12:40–12:47
Ileostomies – a patient education video
Carol Ann Trachsel, Zürich
AbstractBackgroundIleostomies are created primarily to reduce complications of anastomotic leakage, for example after low anterior rectum resections. Although named diverting or “protective” ileostomies, they themselves are associated with significant complications and a high readmission rate. It is therefore essential to provide patients with comprehensive information about stoma care. It is well known that patients do not fully absorb the information from lengthy surgical consenting’s and often have difficulties implementing instructions. According to the cognitive theory, multimedia education is therefore more suitable. In particular, educational videos are an effective method of communicating complex content. AimsFor these reasons, we have created a patient education video on the subject of ileostomy. MethodsOn the basis of a detailed literature search and years of clinical experience, as well as in interdisciplinary discussions with ostomy nurses, the most important points of patient education were identified and a storyboard written. Illustrations were done in collaboration with the experts of the multimedia team. ResultsThe patient education video on ileostomies covers the topics of nutrition with an ileostomy and early warning signs of impending complications, especially dehydration due to high-output ileostomy. It also refers to effective initial measures and provides general tips for maintaining a balanced fluid intake. ConclusionVideos offer the opportunity to access information in a visually comprehensible way and to retrieve it independently and repeatedly. Our video is now being distributed to patients and the impact on postoperative complications, patient safety and the promotion of independence in dealing with the ileostomy is being analyzed. The aim is for patients to be able to recognize stoma-related problems at an early stage and, ideally, to solve them without medical assistance, thereby obviating the need for readmission. 
|
||
|
12:50–12:57
Minimally Invasive Simgoid Resection with the Dexter system™
Nico Seeger, Winterthur
AbstractBackgroundThe evolution of robotic-assisted surgery offers new opportunities for precise and effective treatment of sigmoid colon cancer. The Dexter Robotic System™ is a versatile and compact robotic platform featuring a three-arm setup with a sterile console, enabling full integration into standard laparoscopic workflows while offering benefits like robotic precision, wristed instrument articulation and ergonomics. AimsTo demonstrate the feasibility, surgical technique, and clinical outcomes of robotic-assisted sigmoid resection using the Dexter Robotic System™ for the treatment of sigmoid adenocarcinoma. MethodsA 53-year-old woman (BMI 21 kg/m²) with no prior abdominal surgery presented with a stenosing sigmoid mass confirmed as adenocarcinoma (cT3-4 cN+ cM0) following an episode of diverticulitis. The procedure commenced with laparoscopic mobilization of the sigmoid colon due to adhesions to the lateral abdominal wall. The Dexter robotic platform was then docked, utilizing previously used laparoscopic trocars. Robotic-assisted steps included precise medial-to-lateral dissection, central vascular dissection of the inferior mesenteric artery and vein, and mobilization and division of the mesocolon. Laparoscopic instruments, including an advanced energy sealer and stapler, were employed for division of the rectum and creation of the colorectal anastomosis. Dexter was subsequently used to secure the anastomosis with additional sutures. The video illustrates the surgical technique. ResultsThe surgery was completed successfully without complications or the need for a blood transfusion. Estimated blood loss was 100 mL, and the total operative time was 271 minutes. The patient had an uneventful recovery, with a hospital discharge on postoperative day 3. Histopathological staging revealed pT3a pN1a (1/15) L1 V1 Pn0 R0. ConclusionThis case demonstrates that robotic-assisted sigmoid resection with the Dexter Robotic System™ is a safe and effective technique for sigmoid adenocarcinoma. It offers precise tissue dissection, reliable suturing capabilities, and favourable short-term outcomes, underscoring its potential in minimally invasive oncological surgery. |
||
|
13:00–13:07
Robotic Rectopexy with Dexter
Dieter Hahnloser, Lausanne
AbstractBackgroundThe key benefits of robotics are improved precision and control, thanks to fully articulated robotic instruments and enhanced, stable endoscope control. Case presentationThe herein video demonstrates a fully robotic anterior mesh rectopexy in a 53-year-old patient with obstructed defecation syndrome (ODS). Standard laparoscopic 3-D camera, insufflator, trocars and energy devices, available in all hospitals performing laparoscopic surgery, were used in combination with the Dexter System from Distalmotion SA. Dexter is a compact, multiport platform which includes two robotic instrument arms, one robotic endoscope arm and an open, sterile surgeon console. Four trocars and three single-use instruments (scissors, Maryland dissector and needle holder) were used for this robotic procedure. After dissection of the recto-vaginal septum a DynaMesh®-PRR (FEG Textiltechnik mbH, Aachen, Germany) was sutured to the anterior rectal wall and fixed to the promontory. The peritoneum was closed entirely covering the mesh. The procedure lasted 107 minutes with no intraoperative adverse event. No conversion to standard laparoscopy was necessary in this procedure. The patient was discharged at postoperative day two and had an uneventful recovery. At 3 months, no post-operative adverse event was noted and the ODS symptoms improved with an ODS score before the operation of 22 to 12 post-operatively. ConclusionDexter is a valid open platform robotic solution combining the best of two worlds: robotics where precision and enhanced dexterity are required and standard laparoscopy (with all the equipment already present at every hospital) where it is at its best. The surgeon remains scrubbed-in at all times, allowing a switch between robotics and laparoscopy within seconds. |
||
|
13:10–13:17
Robotic Right-posterior Sectionectomy for Hepatocellular Carcinoma
Christoph Kümmerli, Basel
AbstractBackgroundHepatocellular carcinoma presents significant surgical challenges due to its anatomical complexity and proximity to vital structures. Traditional open approaches have been associated with considerable morbidity and laparoscopy has its limitations due to the limited range of motion. The advent of robotic surgery offers enhanced precision and dexterity, potentially improving outcomes in complex hepatobiliary procedures. Case presentationWe present a case of a 70-year-old male diagnosed with hepatocellular carcinoma located in the right posterior section of the liver measuring 6cm. Preoperative imaging, including MRI and CT scans, confirmed the tumour's resectability. The patient underwent a robotic right posterior sectionectomy using the da Vinci Xi Surgical System. The procedure was performed with the patient in a supine position tilted to the left. Four robotic ports and two assistant ports were utilised. Key steps included complete mobilisation of the right liver, identification and precise division of critical vascular and biliary structures, and precise parenchymal transection using vessel sealer and the “scissor hand” technique. Intraoperative ultrasound was employed to delineate tumour margins and critical vessels. The operation was completed successfully with a total operative time of 240 minutes and an estimated blood loss of 200 ml. The patient had an uneventful postoperative course and was discharged on postoperative day 7. Histopathological examination confirmed clear resection margins (R0). ConclusionThis case demonstrates the feasibility and safety of robotic right-posterior sectionectomy for hepatocellular carcinoma. The robotic approach provides superior visualisation and precision, facilitating complex liver resections with minimal morbidity. According to the IDEAL stages of surgical innovation, more randomised trials are now warranted to compare long-term outcomes of robotic versus conventional techniques in hepatobiliary surgery. |
||
|
13:20–13:27
Robotic technique for resection of liver tumors close to major intrahepatic vessels: How I do it without the CUSA
Eleonora Garosi, Lugano
AbstractBackgroundPrecise vascular dissection during liver surgery is mandatory. Specific instruments for parenchymal transection, however, are lacking in robotic hepatectomy (RH) compared to laparoscopy or open. In particular, the lack of CUSA has been an issue of debate. Thereby surgeons adopted alternative hybrid solutions (CUSA used by the table-assistant) or fully robotic ones with bipolar and robotic sealers versus double bipolar. In the present video, we show some technical examples of precise portal and hepatic veins dissection, and dealing with the hepatocaval confluence, performed with robotic sealer and bipolar forceps, for tumors in close relationship with main biliary/vascular pedicles within the liver. Case presentationCase 1 (Left hepatectomy extended to segment 1 and middle hepatic vein, HCC with left portal thrombosis) Confluence of the left (LHV) and middle hepatic vein (MHV) exposition. US confirmed tumor invasion of the MHV and left portal thrombus. Hilar approach with left portal vein isolation, thrombus management. Case 2 (Right hemihepatectomy for iCAA after right portal embolization) Hilar approach of the plate which is dissected from the porta, hilar plate section to expose right portal branch for section. Case 3-4 (Right-posterior sectionectomies, HCC close to RHV and iCCA) Full right liver mobilization with exposure of inferior vena cava (IVC) and right hepatic vein (RHV). Intraparenchymal isolation and dissection of pedicles for posterior section. Tumor detachment from the RHV. Case 5-6 (Wedge resections in segment 8 at the hepatocaval confluence, CRLM) Confluence of RHV and MHV exposed from above. Dissection of the tumor from major vessels upon US-guidance up to vena cava. Case 7 (HCC recurrence after open left-lateral sectionectomy, at the confluence of LHV-MHV and vena cava) Tumor dissection from hepatocaval confluence in cirrhotic liver. R1vascular for necessity. Case 8 (S2 segmentectomy, CRLM) Full LHV exposition during parenchymotomy. ConclusionRobotic sealer and bipolar forceps is safe for precise anatomical vascular dissection. |
||
|
13:30–13:37
Robotic Right Hemihepatectomy: ready for prime time?
Philip Müller, Basel
AbstractBackgroundRobotic right hemihepatectomy has emerged as a highly effective, minimally invasive alternative to traditional open surgery for the resection of liver lesions. This approach combines the precision and dexterity of robotic systems with the benefits of laparoscopic surgery, offering improved visualization, reduced blood loss, and faster recovery times. Case presentationWe presents the case of a 33-year-old patient with a 6 cm inflammatory adenoma, who underwent robotic-assisted right hemihepatectomy. The procedure was performed using the robotic platform. The adenoma was situated on the portal vein bifurcation of the right anterior and posterior branches. Key surgical steps included:
ConclusionThis case highlights the potential of robotic right hemihepatectomy as a safe and effective option for the resection of liver lesions. The technique offers significant advantages over traditional open surgery, with favorable outcomes in terms of blood loss, recovery time, and patient satisfaction. This video abstract will provide a detailed demonstration of the robotic procedure, showcasing key steps and technical considerations. |
||
|
13:40–13:47
Laparoscopic Liver Resection of Hepatic Cystic Echinococcosis in Segment VIII: A Technical Video
Antonio Fiore, Bern
AbstractBackgroundCystic Echinococcosis (CE) is a very rare zoonotic infection in Western Europe caused by Echinococcus granulosus, predominantly affecting the liver (approximately 80%). Symptoms often merge only after cyst rupture. Treatment options include antiparastitic medications and invasive interventions such as PAIR (puncture, aspiration, injection, and reaspiration) and open or minimally invasive surgery depending on the extent and the location of the disease. AimsWe aim to present the video of a laparoscopic liver resection of a large hepatic CE in Segment VIII, highlighting procedural steps and potential pitfalls. MethodsThe patient was positioned in the French position, slightly raised to the right, and with the right arm abducted overhead. Trocar placement included 5 12mm trocars along the right subcostal line and a 5 mm trocar for the Pringle tourniquet in the left hemi-abdomen. The right liver was fully mobilized, and intraoperative ultrasound guided resection margins. Liver resection was performed using (CUSA®) and (HarmonicTM) devices. ResultsWe report a case of a 38-year-old female with hepatic CE, pre-treated with a stereotactic PAIR procedure. Our center has treated 61 CE patients with 36 undergoing hepatic resections. In this case, a laparoscopic atypical liver resection of segment VIII was completed without significant bleeding. Preoperative PAIR and resection of the cyst with surrounding liver tissue instead of only an enucleation minimized rupture risk. Intraoperative medical prophylaxis against anaphylaxis was performed, as well as peri-operative treatment with Albendazol. The patient recovered uneventfully and was discharged on postoperative day three. Figure 1A shows the resection site, Fig. 1B/C the resected specimen. ConclusionDespite its technical challenges, laparoscopic resection of a segment VIII liver lesion represents an effective surgical approach for managing liver tumors including CE. The potential benefits include reduced postoperative morbidity, shorter hospital stay and faster recovery. 
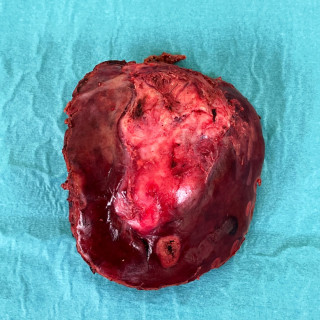

|
||
|
13:50–13:57
Innovation in Minimally Invasive Pancreatic Surgey: Dexter-Assisted Left Pancreatectomy
Giulia Piazza, Lausanne
AbstractBackgroundMinimally invasive surgery (MIS) has progressively become the standard for various procedures, with robotic surgery playing an increasingly important role in this evolution. Robotic platforms are having a growing impact on complex procedures, such as pancreatic surgery, by providing enhanced dexterity, precision and ergonomics. The Dexter robotic system allows smooth transitions between standard laparoscopy and robotic assistance, providing greater flexibility during surgery. This feature enables surgeons to maximize the advantages of both techniques and facilitate intraoperative teaching. AimsTo demonstrate the feasibility of a Dexter-assisted distal pancreatectomy and highlight its advantages. MethodsWe present a clinical case of a patient undergoing a Dexter-assisted distal pancreatectomy, highlighting the advantages of combining standard laparoscopy with the Dexter robotic platform. ResultsWe present the case of a 63-year-old patient with a history of coronary artery disease treated with stenting and previous open appendicectomy. The patient presented with a pulsatile abdominal pain, and an ultrasound showed a 20 mm hypervascular lesion in the body of the pancreas. Subsequent CT scan and MRI confirmed an 18 mm lesion. A PET/CT was also performed and showed an increased uptake of the pancreatic lesion measuring 33 mm, with no other fixations. Endocrinological evaluation revealed slightly elevated chromogranin and glucagon levels. Biopsy confirmed a well-differentiated grade 1 neuroendocrine tumor. ConclusionThe Dexter robotic system provides an innovative and effective approach for complex pancreatic surgery, combining the advantages of laparoscopic and robotic surgery. Its flexibility enhances surgical precision and facilitates intraoperative teaching. |
||
|
12:30 – 14:00
Room 1B
|
HPB
Guido Beldi, Bern; Maurice Matter, Lausanne
|
|
|
Free Communication
|
||
|
12:40–12:47
From Competency to Mastery: Learning Phases in Robotic Liver Surgery in 5 International Expert Centres
Gabriel Fridolin Hess, BASEL / Basel
AbstractBackgroundOpen liver surgery is increasingly being replaced by minimally invasive surgery, especially using robot-assisted liver resections (RLR). Along the learning phases of a surgical procedure intraoperative, postoperative, and oncologic outcomes improve at different stages. AimsThe aim of this study is to evaluate the learning phases of RLR in a large retrospective international multicentre setting to determine the number of procedures required to achieve competency, proficiency and mastery. MethodsConsecutive patients from 5 international expert centres who underwent elective RLR were included. Three thresholds were used to define the learning curve based on the first 150 RLRs in each centre: Operative time for competency, major complications (Clavien-Dindo ≥III) for proficiency, and textbook outcome for mastery. Clinical outcomes before and after the thresholds were compared. ResultsThe learning curve analysis was performed on 662 RLRs. From competency to proficiency 23 cases and from proficiency to mastery 63 cases were required. The rate of technically major/major resections increased significantly throughout the three phases (p<0.001), while the rate of major complications (8.4% to 7.1%) and length of hospitalisation (4 to 3 days) remained stable. RLRs were associated with an excellent rate of patients reaching textbook outcome from the beginning (87%). ConclusionCompetency, proficiency and mastery of RLR were achieved after 23 and 63 cases respectively. Robotic liver surgery was associated with excellent perioperative results while the indications towards major liver resections were expanded gradually. |
||
|
12:50–12:57
Specific items of perioperative care for liver surgery in cirrhotic patients: a systematic review
Constant Delabays, Lausanne
AbstractBackgroundEnhanced Recovery After Surgery (ERAS) pathways have been shown to be safe in cirrhotic patients undergoing hepatectomy. However, due to cirrhosis-induced complications, specific or additional items might need to be implemented. AimsThis study systematically reviewed the literature to assess specific items for the perioperative management of cirrhotic patients undergoing hepatectomy. MethodsA systematic review was performed until September 2024. Evaluated items were prevention and management of perioperative ascites, perioperative anticoagulation, perioperative nutrition, prophylactic abdominal drainage, encephalopathy prevention, postoperative analgesia, and vascular filling. Levels of evidence were given for each specific item based on the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system. ResultsA total of 2983 articles were screened, and 79 articles were included in the final analysis of the 7 evaluated items. Four items had a moderate or high level of evidence. Summary of the 4 items with moderate/high evidence level were I) preoperative ascites should be controlled before surgery, II) mechanical and pharmacological venous thrombo-embolism prophylaxis is recommended postoperatively if coagulation tests are within normal range, III) systematic drainage among patients with chronic liver disease or cirrhosis is not recommended, and IV) acetate-buffered solutions should be preferred over Hartmann solutions or 0.9% saline. ConclusionThis systematic review comprehensively evaluated specific perioperative items for cirrhotic patients undergoing liver surgery. Level of current evidence remains weak, and future research are still needed to develop specific recommendations for ERAS in cirrhotic patients undergoing liver surgery. |
||
|
13:00–13:07
Textbook outcome in elderly patients undergoing liver surgery
Emilie Zhu, Lausanne
AbstractBackgroundTextbook outcome (TO) is a novel composite outcome to measure quality and postoperative results. Data on TO in elderly patients undergoing liver surgery remain scant. AimsThis study aimed to assess the percentage of elderly patients achieving TO compared to young patients. MethodsA cross-sectional, single-center study was performed. All consecutive patients undergoing liver surgery (2013-2023) were included. All patients followed an ERAS pathway. Patients ≥70 years were defined as elderly. TO achievement was defined as absence of intraoperative grade 2/3 event, grade B/C biliary fistula, grade B/C liver failure, 90-day major complication (>3a Clavien), 90-day readmission and R1 resection margin. Predictive factors of TO achievement were calculated using multivariable binary logistic regression. ResultsA total of 618 patients were included (men 359/618=58%, median age 64, major hepatectomies 271/618=44%). One hundred-and-seventy-nine (29%) patients were ≥70 years. Overall complication rate was 281/618 (45%) and major complications occurred in 117/618 patients (19%). TO was achieved in 354 patients (57%). TO in elderly patients (101/179=56%) was similar as in younger patients (253/439=58%) (p=0.783). On multivariable analysis, operation time (OR 1, p=0.039), preoperative total bilirubin (OR 1, p=0.031), preoperative prothrombin time (OR 1, p=0.036), and compliance to Enhanced Recovery After Surgery (ERAS) items >60% (OR 1.9, p=0.006) were independent predictors of TO achievement, while age (OR 1, p=0.312) and minimally invasive surgery (OR 1.4, p=0.112) were not. ConclusionThis study found that TO achievement after liver surgery was similar in elderly and young patients. Age was not a TO predictor contrarily to operation time, bilirubin, prothrombin time, and compliance to ERAS. |
||
|
13:10–13:17
Comparison of Perioperative Outcomes in Robotic vs. Open Major Hepatectomy: A Single Center Propensity Score-Matched Pilot Study
Ruben Mercier, Genève
AbstractBackgroundRobot techniques have gained traction in the field of hepatobiliary surgery with previous studies demonstrating feasibility and safety of the robotic approach. However, a majority of major liver resections are still performed by laparotomy in Switzerland. AimsThis study aims to evaluate the robotic approach for complex liver resections in the Swiss setting. MethodsIn this case-control study, propensity score matching (PSM) analysis was performed to minimize selection bias. Patients undergoing either robotic or open major hepatectomy at a single academic medical center were included. Data on patient demographics, tumor characteristics, and perioperative outcomes were collected and analyzed. ResultsA total of 59 patients were included; 17 robotic and 42 open cases. After PSM, 51 patients (17 robotic and 34 open) were analyzed. Baseline characteristics were comparable between groups, including age (64 vs. 66 years; p > 0.9), BMI (23.7 vs. 25.0; p > 0.9), and ASA score distribution (p = 0.6). Robotic cases demonstrated significantly shorter length of stay (median, 9 vs. 13 days; p = 0.025) and lower comprehensive complication index (median, 0 vs. 26; p = 0.004). No significant differences were observed in postoperative complications (47% vs. 50%; p = 0.8) or length of ICU stay (p = 0.083). Conversion occurred for two patients in the robotic group (11.7%). Median operative time was longer in the robotic group (473 vs. 362 minutes; p = 0.053). Although bile leaks occurred more frequently in robotic cases (12% vs. 0%; p = 0.13), the difference was not statistically significant. ConclusionRobotic major hepatectomy was associated with reduced length of stay and lower complication severity compared with the open approach. Both techniques demonstrated similar rates of postoperative complications, confirming the safety and feasibility of robotic hepatectomy in experienced centers. Future research should focus on collaborative efforts between Swiss centers performing complex robotic liver surgery to further improve outcomes and expand the evidence base. 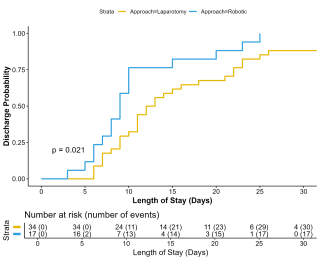
|
||
|
13:20–13:27
Safety and Feasibility of Robotic Repeat Hepatectomy Compared to Laparoscopic and Open Techniques: a Retrospective Cohort Study
Eleonora Garosi, Lugano
AbstractBackgroundRepeat hepatectomies can often be challenging operations due to altered anatomy and adhesions from prior surgeries. Thanks to the enhanced dexterity, better vision and stability, the robotic approach could expand the feasibility of minimally invasive liver surgery in the setting of repeat hepatectomies. AimsTo explore the surgical safety and oncologic efficacy of repeat robotic liver resection (RLR) compared to repeat laparoscopic (LLR) and open liver resection (OLR). MethodsAll repeat liver resection performed from January 2019 to December 2024 were retrospectively reviewed. Primary endpoints were complications (Comprehensive Comorbidity Index, CCI), conversions and rate of negative surgical margin (R0) or equivalent (R1 vascular). ResultsForty-two patients underwent repeat hepatectomy (OLR=15, LLR=13, RLR=14). The main indication to surgery was colorectal liver metastases (55%) followed by hepatocellular carcinoma (21.4%). Preoperative patients characteristics were similar: mean age of 68 years, ASA score of 3 and Charlson Comorbidity Index of 9. Only two patients in the LLR group required conversion to laparotomy vs none in the RLR group. Mean operative time was 466, 314 and 277 minutes (p=0.02) with mean blood loss of 320, 275 and 95 mL (p=0.01) in OLR, LLR and RLR, respectively. Post-operative overall complications occurred in 40% of OLR and 7.6% of LLR patients while none occurred in RLR (p=0.02) with mean CCI of 29.2, 8.7 and 0, in the respective order. There was no overall mortality in the 90 days after surgery. R0 was 73%, 100% and 77% (p=0.04) and R1 vascular was 13.3%, 0% and 23% (p=0.08) in the OLR, LLR and RLR groups. ConclusionRepeat RLR was not only safe but better in outcome, and ensured adequate oncologic results compared to LLR and OLR. |
||
|
13:30–13:37
Challenges in the implementation of enhanced recovery after surgery (ERAS) pathways for major hepatectomies: a retrospective cohort study
Lorenzo Bernardi, Lugano / Lausanne
AbstractBackgroundEnhanced recovery after surgery (ERAS) programs showed benefit by improving patient’s outcomes in liver surgery. However, obtaining high compliance with ERAS may be challenging for patients with major hepatectomy. AimsThe aim of the study was to investigate the challenges related to the implementation of ERAS in major hepatectomy by assessing the compliance in detail. MethodsAll consecutive major hepatectomies (≥3 Couinaud segments) within an ERAS program from 2013 to 2023 were reviewed. The primary endpoint was the proportion of patients achieving high compliance (≥70%) with ERAS protocol. Secondary endpoints included the institutional learning curve for improving compliance measured with the cumulative sum method (CUSUM), and the clinical outcomes of patients with high vs low compliance. Predictors of high ERAS compliance and of postoperative complications were assessed by a binary logistic regression model. ResultsTwo-hundred-eighty-six patients were included, median ERAS compliance was 59% (IQR 54-67) and 49 patients (17.1%) had a high compliance The CUSUM analysis identified an institutional learning curve of 143 cases encompassing the first 5 years of activity. High compliance patients increased 10-fold from during the learning curve to once the learning curve was completed (8.2% vs 91.8%; p<0.001) The improvement was mainly related to better compliance with intra- and postoperative ERAS items. High compliance was associated with less complications (53.1 vs 69.1%; p=0.045) and shorter hospital stay (8 vs 12 days; p=0.002). In multivariable analysis, the strongest independent predictor of high ERAS compliance was the use of MILS. High compliance was protective only against minor complications (Clavien-Dindo<IIIa). ConclusionThe implementation of an ERAS program with high compliance is challenging in major hepatectomy and needed more than 140 cases in our experience. A MILS policy, when feasible, should be pursued to increase compliance, which is associated to less complications and shorter hospital stay. 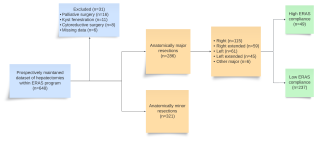
|
||
|
13:40–13:47
Complexity adjusted, learning curve assessment by multiple endpoints in laparoscopic and robotic liver resections: a retrospective study of 148 cases
Lorenzo Bernardi, Lugano / Lausanne
AbstractBackgroundThe methodology for learning curve assessment in laparoscopic (LLR) or robotic (RLR) liver resections is debated and heterogeneously reported. Several studies didn’t account for patient’s and procedure complexity, thus lacking generalizability. AimsThe aim of the study was the assessment of the learning curve in LLR and RLR considering both patient’s and procedure complexity. MethodsConsecutive LLR and RLR from 2019 to 2024 by a single surgeon trained sequentially in LLR then in RLR were reviewed. The learning curve was analyzed with the cumulative summation (CUSUM) method after adjusting for patient- and procedure-related confounders (age, sex, BMI, comorbidities, previous hepatectomy, portal hypertension, Iwate score, multiple resection areas, extension to neighbor organs, lymphadenectomy, associated local treatment). The primary endpoints were the learning phases for significant changes in operative time, blood loss, complications, and conversions. ResultsOne-hundred-forty-eight patients were included (LLR=94; RLR=54). In LLR vs RLR, mean age was 66.8±12.4 vs 66.4±10.4 (p=0.827), Charlson comorbidity index was 7 (IQR 5-9) in both groups. Median Iwate score was 6 (IQR 3-7) vs 5 (IQR 4-7) (p=0.694), conversions to laparotomy were 10 (10.6%) vs 1 (1.9%) (p=0.051) and complications were 16 (17%) and 14 (26%) (p=0.295) in LLR vs RLR respectively. CUSUM analyses showed that the adjusted operative time dropped after 45 LLRs vs 18 RLRs, blood loss dropped after 45 LLRs vs 25 RLRs. A composite endpoint of operative time and blood loss confirmed these results. No learning curve effect was seen for complications or conversions in either group. ConclusionThe robotic platform showed to have a significant impact on a faster learning curve in terms of operative time and blood losses. The sequential experience can play a role in faster learning. In liver surgery, patient’s and disease’s complexity can influence the outcomes alongside technical experience and must be considered for reliable learning curve assessments. |
||
|
13:50–13:57
Safety and efficacy of minor robotic liver resection in patients with cirrhosis and portal hypertension: a retrospective cohort study
Lorenzo Bernardi, Lugano / Lausanne
AbstractBackgroundThe role of robotic liver resection (RLR) is under-explored in patients with cirrhosis complicated by portal hypertension (PH).
AimsThe objective of the study was to explore the safety (complications and post-hepatectomy liver failure, PHLF) and oncologic efficacy (R0 and disease-free interval, DFI) of RLR in patients with cirrhosis and portal hypertension. MethodsConsecutive RLRs in patients with cirrhosis were retrospectively reviewed. Surgical and oncologic outcomes were compared between patients with and without PH. Recurrence-free survival was defined as the time between RLR and tumor recurrence or last follow-up. ResultsEighty patients underwent RLR for liver malignancies (males: 71.3%, median age: 70 years, Child-Pugh score A: 95%, history of HCV: 45%, single nodule: 90%). Median size of the tumor was 23 mm (IQR 18-30 mm). Twenty-three patients had PH (28.7%); preoperative characteristics were otherwise similar between patients with and without PH. All the 23 patients with PH underwent non-anatomic resection vs 48 (84.3%) in the group without PH (p=0.63), without any major hepatectomy. Surgical outcomes were also similar except for PHLF which occurred in 21.7% of patients with PH and none without PH (grade A: 8.7%, grade B: 13.0%, no grade C; p=0.0059). Complications occurred in 30.4% of patients with PH vs 15.8% without PH (p=0.24), conversion rate to open surgery was 8% in both groups, median blood loss was 150 vs 100 cc (p=0.07). Post-operative mortality was nihil in the series. R0 rate was obtained in 100% vs 88% (p=0.63) and RFS was equal in patients with and without PH (median of 19 months, p=0.86). In multivariable analysis PH was not associated with recurrence. ConclusionIn this small cohort of minor and mostly non-anatomic RLRs, the presence of PH was associated with a higher rate of PHLF (grade A and B, without grade C) but not with other surgical or oncologic outcomes. |
||
|
12:30 – 14:00
Room 5A
|
Radioprotection in Surgery
Reto Treier, Bern; Yvonne Käser, Uetikon am See
|
|
|
Course
|
Practical application today is so diverse that one should not generalise when giving instructions. Of course, there are clearly defined basic rules, especially for organisation. However, the practical working techniques of the various medical disciplines should always be taken into account. Radiation protection can and must be partly subject-, application- or even person-related.
|
|
|
12:30 – 14:00
Room 5B
|
Treatment of Pancreatitis - trends and current standards
Markus Weber, Zurich; Diego de Lorenzi, Grabs
|
|
|
Main Session
|
||
|
12:30–12:50
How to assess severeness of pancreatitis – classifications
Patryk Kambakamba, Winterthur
|
||
|
12:50–13:20
The stepup approach (DDD) – How many hot-axios to surgery?
Riad Sarraj, Bern
|
||
|
13:20–13:40
Surgical therapy including VARD - tips and tricks
Beat Müller, Basel
|
||
|
13:40–14:00
Outcome of pancreatitis – is the fight worth it?
Martin Bolli, Luzern
|
||
|
12:30 – 14:00
Foyer Garden
|
Visual Abstract Tour |
|
|
Free Communication
|
||
|
14:00 – 14:30
|
Coffee Break |
|
|
Break
|
||
|
14:30 – 16:00
Room 4A
|
Bariatric-Metabolic Surgery and the General Surgeon
Anna Dayer, Rennaz; Styliani Mantziari, Lausanne
|
|
|
Main Session
|
||
|
14:30–14:48
Medical treatment of obesity: what the surgeon needs to know
Lucie Favre, Lausanne
|
||
|
14:48–15:06
Endoscopic treatment of obesity: hype or hope?
Simon Bütikofer, Lucerne
|
||
|
15:06–15:24
Is there still a role for bariatric-metabolic surgery? Current knowledge and future perspectives
Daniel Gero, Zurich
|
||
|
15:24–15:42
Management of Gastroesophageal Reflux after Sleeve Gastrectomy
Francesco Abboretti, Lausanne
|
||
|
15:42–16:00
Prevention and management of internal hernias after Roux-en-Y gastric bypass
François Pugin, Fribourg
|
||
|
14:30 – 16:00
Room 5A
|
Coloproctology
Frédéric Ris, Geneva; Andrea Wirsching, Baden
|
|
|
Free Communication
|
||
|
14:30–14:38
Sacral Neuromodulation Improves Functional Outcome and Quality of Life in Patients With Pouch Dysfunction After Pan Proctocolectomy for Ulcerative Colitis
Matteo Di Giuseppe, Locarno
AbstractBackgroundPostoperative frequency of bowel movements and impaired fecal continence (FI) has a negative impact on quality of life following ileal pouch-anal anastomosis. Sacral neuromodulation (SNM) is a validated treatment of FI but its effectiveness in IPAA patients has been poorly reported. AimsThe aim of this study was to evaluate the effectiveness of sacral neuromodulation (SNM) in improving the functional outcomes and quality of life of patients with pouch dysfunction following ileal pouch-anal anastomosis (IPAA) for ulcerative colitis. In particular, the study sought to compare the outcomes of SNM treatment in patients with IPAA suffering from fecal incontinence (FI) with those of patients routinely treated with SNM for FI. MethodsA 3 weeks test-phase was performed before definitive implantation of the pulse generator. Patient’s data were prospectively gathered in a dedicated registry. IPAA patients were then compared to a matched-paired control group of patients routinely treated by SNM for FI. ResultsBetween 2007 and 2020, 14 IPAA patients were tested and 12 (85%) were implanted. This group was compared to a matched group of 20 patients implanted for FI. After a mean follow-up of 4.8 [0.5-16] years, there was a significant decrease of weekly leaks (29 vs 2 ;p=0.01), Wexner score (15 vs 10.8 ;p=0.01) and an improvement of quality of life (FIQOL 1.853 vs 2.42 ;p=0.01). IPAA patients evolved equally as compared to the control group in terms of Wexner score and quality of life at 6 months, 1 year and 2 years. ConclusionSNM provides a significant decrease of leaks and improves Wexner scores and quality of life in IPAA patients. The effectiveness seems comparable to these of patients routinely treated by SNM for FI. SNM indications could be extended to IPAA patients presenting bad functional outcome. 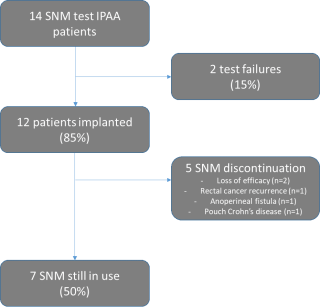
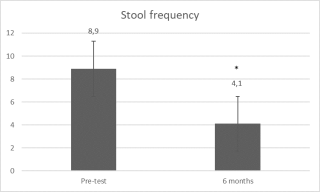
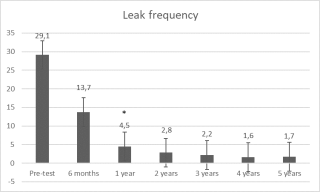
|
||
|
14:41–14:49
Allogeneic Expanded Adipose-Derived Mesenchymal Stem Cell Therapy for Perianal Fistulas in Crohn’s Disease: Conclusions from a six Year Single Center Experience
Daniela Cabalzar-Wondberg, Zurich
AbstractBackgroundThe treatment of perianal fistula, particularly in patients with Cohn's disease (CD), remains challenging. Analogous to the Admire trial published in 2016, a new therapy was established using mesenchymal stem cell injections (MSC). AimsEight years after approval, this treatment has now been withdrawn from the market due to no longer significantly demonstrable advantage in terms of closure rate compared to the treatment with placebo. We report our series of patients treated at one of two national centers to determine real world efficacy. MethodsIn total, we have treated 35 patients with CD and complex perianal fistula between February 2019 and July 2024 with a local injection of 120 million allogeneic MSC at a tertiary hospital. ResultsOf the 35 patients who were treated, 22 patients (63%) were male. The median age was 37 (18 to 82) years. On average, the patients suffered from fistulas for 5 years and from Crohn's disease for 12 years. The mean follow-up time was 46 months (5 to 70 months). Overall, fistula closure was found in 20 patients (57%). In 4 (27%) of the 15 patients in whom MSC treatment failed, closure was achieved by subsequent reoperation. A total of 8 (22%) patients developed perianal abscess which had to be treated surgically. Six of the patients treated are smokers. Of these, 5 patients did not experience any fistula healing. ConclusionAfter almost six years of complex fistula treatment with MSC, we were able to confirm the initial results of the Admire trial with a fistula closure rate of 57%. Despite the small number of 35 patients, this is one of the largest available series on MSC treatment for CD fistulas. The closure rate of 57% compares to classic surgical fistula treatments, thereby questioning the high cost of MSC treatment and supporting its cessation. |
||
|
14:52–15:00
Follow-up After Resection of High Grade Anal Intraepithelial Neoplasia (HSIL): How Long is Enough?
Susanne Bock, St. Gallen
AbstractBackgroundIncidence of Anal Carcinoma (AC) and its precursor lesion, HSIL, is rising. After incidental or planned resection of HSIL, surgeons are facing the question of whether a follow-up is necessary and how long. Given the fact that HSIL is induced by the Human Papilloma Virus (HPV), similarities to gynaecological dysplasia that can request life-long follow-up may exist. AimsTo find out when recurrence occurs after resection of HSIL. MethodsAll patients who received surgical excision for HSIL in our institution from 1.1.2013 to 31.12.2018 were retrospectively extracted from our prospective database. Only those with R0 resection margins were included. Time to recurrence was collected, as well as patient characteristics. Results24 patients (14 female, 7 male with HIV) received R0-resection of HSIL. 12 primary surgeries (50%) included skin transposition. 8 patients (33%) needed more than one surgery, either to achieve R0-resection (4 patients, 1-3 surgeries) or due to complications (4 patients, 2-5 surgeries) . 12 of the patients (50 %) had a recurrence (1 Carcinoma, 6 HSIL, 5 LSIL) which occurred after a median 63 months (3-131). The recurrence rate of HSIL/Carcinoma alone (without LSIL) was 29% and always occurred more than 60 months after initial resection (median 72, range 62-131). ConclusionAfter resection of HSIL, even when performed quite radically needing plastic surgery, recurrence is common and occurs usually more than five years after the initial resection. Therefore, longtime follow-up is mandatory, possibly life-long. We recommend following the patients in specialized clinics, if possible with high resolution anoscopy.
|
||
|
15:03–15:11
Guardians of the Scalpel in Proctology: exhaustive review.
E. Xavier Delgadillo - Pfenninger, La Chaux-de-Fonds
AbstractBackgroundWe might considered Ancient Egypt as the cradle of surgery, and Egyptian coloproctological surgery may have a crucial role of influence in the practice of surgery in neighbouring cultures, including Greeks and Romans. AimsEgyptian influence spread beyond Europe, thereby affecting Western civilization significantly. We keep ancient documents on western countries describing as the Smith's Papyrus and Eber’s Papyrus, demonstarting allegations regarding proctological surgery from the ancient Egypt have a main role until today. MethodsStudy Design consisted in an exhaustive review of original sources, modern literature papers regarding proctological surgery (7) and proctologists in the ancient Egypt. We had compiled documentation during 15 years (2009-2024), that we found in Saqqara, Cairo, Vienna and London. ResultsWe found in 34 literature sources, 24 archaeological / proctologic sources, 117 medical libraries and 8 personnel explorations on-site: We found “two main surgeons in proctology” called the treat anal entities. 94% of pictographs demonstrated that two great proctologists existed in ancient Egypt, however, this is open to interpretation because there were named “shepherds of the anus” and not surgeons (Figure No. 1). Therapeutic options were mentioned in the literary sources, while the specimens suggested demonstrating such treatments were credited to those physicians and not to sorcerers. The outstanding surgeons identified were : Ir En Athky and Khouy Hwi. Both distant one to each other about 150 years. We verified their knowledge and the conventional level of Egyptian colorectal surgery possibly performed under uncommon circumstances. ConclusionThe ancient Egyptians certainly treated proctological diseases of various kinds, and with varying degrees of success. Concerning surgical procedures and therapeutic drainages, there is no clear evidence for the existence of such procedures as demonstrated for example in Greece. It would, however, be surprising if malignant entities were not treated, even though they have not left traces in the surviving sources. 
|
||
|
15:14–15:22
Pruritus ani (Diagnosis to Treatment): Updated-Umbrella review.
E. Xavier Delgadillo - Pfenninger, La Chaux-de-Fonds
AbstractBackgroundPruritus ani a complex syndrome, generally idiopathic, often accompanied by a psychogenic component, very difficult for colo-proctologist to identify primary and secondary etiology's and very hard to diagnose. AimsTransmit to young surgeons, strength specialist's knowledge to identify primary+secondary causes of pruritus ani and guide choosing the best hygienic-dietary meassures and treatments. Clues and Algorythm for diagnosis. Figure No 1. MethodsUpdated-umbrella review towards diagnosis & treatment, non-meta-analytical, thus a comprehensive review of the international literature. Accessed through software research programs, dividing the study in 3 phases: 1st Analysis, 2nd Cataloging, 3rd Responses, spanning time 20 years (2003 to 2023). ResultsBy Google Scholar we yielded 8,160 results : pruritus ani (scratching, itching, diagnosis & treatment). Bing 41,500 results and Yahoo 364,000 results. We limited analysis of medical literature in English at PubMed 136 : Pruritus ani, 121 : itching, 275 : scratching, 70 : diagnosis-treatment. Odds Ratio (OR 0:1.1) Figure No.2 ConclusionPruritus ani frequently refractory to initial treatment, in case of a therapeutic failure, the patient should be send to the dermatologist (second opinion). Definitively frustrating for both, patient and surgeon, not being able to find an objective cause for anal pruritus is a reason to avoid any unnecessary surgical procedures. The presence of concomitant lesions conduct to proceed to excision-biopsy. 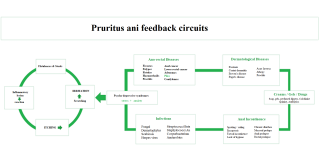
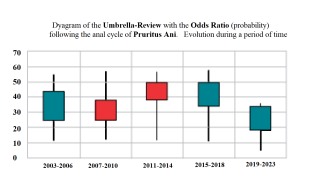
|
||
|
15:25–15:33
Preventing Wound Complications with Prophylactic Negative-Pressure Therapy After Abdomino-Perineal Resection: A Systematic Review
Alexis Litchinko, Fribourg
AbstractBackgroundPerineal wound complications following abdominoperineal resection (APR) for anal or low rectal cancer remain a significant clinical challenge, frequently leading to high rates of surgical site infections (SSIs), wound dehiscence, and prolonged healing. These complications not only increase patient morbidity but also contribute to extended hospital stays and greater healthcare costs. Negative pressure wound therapy (NPWT) has emerged as a potential intervention to improve wound outcomes in this setting, yet its clinical effectiveness remains uncertain. AimsThis systematic review aims to evaluate the effectiveness of NPWT in managing perineal wounds after APR. Specifically, it focuses on the impact of NPWT on reducing SSIs, decreasing wound dehiscence, and enhancing overall healing. MethodsA comprehensive literature search was performed in MEDLINE, Embase, and the Cochrane Library following PRISMA guidelines. Eligible studies included randomized controlled trials, cohort studies, and case series investigating NPWT for perineal wounds post-APR. Data on SSI rates, wound dehiscence, healing time, and related complications were extracted. Due to heterogeneity in study designs and reported outcomes, a narrative synthesis was undertaken. ResultsNine studies met the inclusion criteria, representing a range of study designs and sample sizes. NPWT use was generally associated with lower SSI rates, with some studies reporting up to a 30% reduction compared to conventional dressings. Evidence also suggested potential benefits in reducing wound dehiscence and improving healing times. However, variability in patient populations, study quality, and NPWT application protocols, as well as device-related complications (e.g., vacuum malfunctions), limit the overall strength and generalizability of the current evidence. ConclusionNPWT shows promise in improving the management of perineal wounds following APR, particularly among high-risk patient groups. Nonetheless, existing evidence is constrained by methodological heterogeneity, small sample sizes, and technical challenges. Larger, well-designed randomized controlled trials are needed to confirm the efficacy of NPWT and to establish standardized guidelines for its integration into clinical practice. |
||
|
15:36–15:44
IMPACT OF SPORT PRACTICE ON PELVI-PERINEAL SYMPTOMS IN ACTIVE WOMEN
Guillaume Meurette, Geneva
AbstractBackgroundLimiting the sport practice is routinely recommended for patients with perineal symptoms, but little is known on the prevalence of perineal complaints and the real negative impact of sport practice in the active population.
AimsTo assess the prevalence of pelvi-perineal symptoms (fecal incontinence, urinary incontinence, sexual dyscomfort and prolapse) in an active female population and to evaluate the impact of sports practice on these symptoms. MethodsA cross-sectional study was performed by administering a online-questionnaire addressing 25 questions on physical activity and pelvi-perineal symptoms in various gym centers and universities across Geneva during a 4 month period. ResultsTwo-hundred and eighty questionnaires were collected from 264 women and 16 men, leaving 264 questionnaires for analysis. Most of responders (70.8%) were younger than 50 years. The mean BMI was 23.1+/-3.9, 22.7% met the criteria for obesity. One hundred thirty-eight responders (52.3%) experienced pregnancy. In terms of physical activity, one hundred and sixty-nine responders practiced some kind of regular sports. Of note, 187 of them reported exercising at least twice weekly (77.3%). In terms of pelvi-perineal symptoms, 89 (34%) responders suffered from dyspareunia, 107 (40.5%) from anal incontinence (gas: 34.9%, feces: 5.7%), and 120 (45.5%) from urinary incontinence. Fifty-one responders (24.1%) reported suffering from pelvic prolapse. As expected, childbirth were predictive of perineal symptoms (both urinary and fecal incontinence). On the contrary, physical activity did not predict a worsening of anal incontinence (p=0.578), urinary incontinence (p=0.787) or prolapse (p=0.353). Frequency of sport practice did not modulate these results nor the type of sport. ConclusionBased on our findings, prevalence of perineal symptoms is high among an active population of female; the sport practice seems not to be of negative impact on the perineal comfort |
||
|
15:47–15:55
Robotic vs Laparoscopic Rectopexy: A Single-Center Observational Study
Nicerine Krause, genève
AbstractBackgroundMinimally invasive techniques, including laparoscopic and robotic-assisted rectopexy, have become the standard of care for rectal prolapse repair. However, there is ongoing debate regarding the comparative effectiveness of these approaches, particularly in terms of recurrence, and functional outcomes. AimsThe study aimed to compare the perioperative, short-term, and long-term outcomes of robotic-assisted versus conventional laparoscopic rectopexy in a single high-volume tertiary care center MethodsThis retrospective cohort study included 157 patients who underwent laparoscopic (n=130) or robotic (n=27) rectopexy for rectal prolapse between 2013 and 2023. Exclusion criteria included recurrent cases, open procedures, or multiple concomitant interventions. Baseline characteristics, perioperative outcomes, and long-term results were analyzed using descriptive statistics and bivariate tests. Recurrence rates were evaluated using Kaplan-Meier survival analysis. ResultsBaseline characteristics, including age, gender, and ASA scores, were similar between groups. Robotic rectopexy was more frequently associated with mesh implantation (96.3% vs. 72.3%, p=0.006). Operative time was significantly longer for robotic cases (150 ± 55 minutes vs. 120 ± 51 minutes, p=0.011). Intraoperative complications and conversion rates were comparable. Postoperative recovery profiles, including length of hospital stay and laboratory markers, did not differ significantly. Recurrence rates were lower in the robotic group (3.7% vs. 21%, p=0.049), and reoperations were exclusively reported in the laparoscopic group (13%, p=0.048). ConclusionRobotic-assisted rectopexy demonstrated comparable safety to laparoscopy, with advantages in recurrence and reoperation rates. While operative time remains longer, robotic surgery is a promising modality, particularly in complex cases. Prospective multicenter studies are warranted to further investigate long-term functional and patient-reported outcomes. |
||
|
14:30 – 16:00
Room 1B
|
Colorectal II
Martin Hübner, Lausanne; Seraina Faes, Zurich
|
|
|
Free Communication
|
||
|
14:30–14:38
Hirschsprung Associated Enterocolitis (HAEC) in patients after transanal pull through – A Retrospective Analysis of 24 years
Lea Fackler, Luzern 16 / Lucerne
AbstractBackgroundHirschsprung associated enterocolitis (HAEC) is one of the most severe known complications of Hirschsprung’s disease, both pre- and postoperatively. Current understanding of the pathogenetic mechanism is dysmotility with microbial dysbiosis, altered intestinal barrier function and impaired mucosal immune response. Typical clinical findings of the intestinal inflammation are fever, abdominal distention, diarrhea and sepsis. AimsTo explore the efficacy of consequent postoperative bougienage and consequent long-time follow-ups to reduce the frequency of HAEC. MethodsA retrospective analysis involving 53 patients who underwent transanal pull through (with and without laparoscopic mobilization) between 1999 and 2023 at our institution was conducted. Rigorous follow-up protocols were implemented, incorporating regular bougienage sessions during the initial three months postoperatively. Patient records, including clinical notes and diagnostic tests, were carefully reviewed to assess the incidence of HAEC. ResultsAmong our cohort, out of the 53 children, only one confirmed case of postoperative HAEC was documented. Another case was suspected but never confirmed. This remarkably low HAEC rate of 4% in postoperative cases highlights the potential benefits of our implemented bougienage strategy and consequent regular follow ups with early detection of stenosis and constipation as well as its treatment in preventing HAEC following transanal pull through. ConclusionConsequent postoperative bougienage, implemented in a meticulous follow up regimen, has proven to be a promising approach to reduce the risk of Hirschsprung Associated Enterocolitis following transanal pull through procedures. |
||
|
14:41–14:49
Spinal anesthesia decreases pain and total hospitalization costs but not ileus after colon surgery: A prospective study
Elena Krombholz, Baden
AbstractBackgroundSpinal anaesthesia (SA) as an adjunct to general anaesthesia has been shown to improve perioperative pain management after colorectal surgery. A subsequent reduction of opioid analgesics might further shorten postoperative ileus and costs in colorectal surgery. AimsWe aimed to assess the impact of spinal anaesthesia on pain control, postoperative ileus and costs after colorectal surgery. MethodsStarting in June 2021, all patients undergoing colorectal surgery at our center were offered SA in addition to general anesthesia in order to improve pain control. Patients with contraindications to SA or patients refusing SA were commonly managed with opioids in addition to basic analgesics. Data of consecutive patients undergoing elective, laparoscopic colorectal resections not receiving an ostomy between October 2021 and April 2024 were entered into a prospective database. ResultsOur analysis includes a total of 170 patients (112 with SA and 58 patients without SA). The majority of patients was female in both groups (54% vs. 60%, p=0.399). Laparoscopic sigmoid resection was most frequently performed in both groups (66% vs. 67%, p=0.938) followed by right hemicolectomy (21% vs. 19%, p=0.850). Spinal anaesthesia was associated with a decreased median numeric rating scale for pain at 3h (0 vs 5, p= 0.009), 6h (2 vs. 3, p=0.004) and 24h (2 vs. 5, p=0.012) following surgery. There was no difference in median time-to-flatus (27h vs. 27h, p=0.355), time-to-stool (67h vs. 71h, p=0.245) and time-to-normal diet (62h vs. 67h, p=0.155) after surgery. SA was associated with a decrease in hospital length of stay (6 days vs. 7 days, p=0.038) and total hospitalization costs (16 485 CHF vs. 18047 CHF, p=0.044). ConclusionSpinal anesthesia improves postoperative pain control and is associated with a decrease in hospitalization costs and length-of-stay. There was not impact of SA on return of bowel function. |
||
|
14:52–15:00
Improving compliance and satisfaction with quality coffee intake to enhance bowel recovery after colorectal surgery
Constant Delabays, Lausanne
AbstractBackgroundCoffee is a simple, safe, and inexpensive method to prevent post-operative ileus (POI) after digestive surgery. However, uptake of coffee in clinical routine is variable, standardization challenging and compliance unknown. AimsThis study aimed to determine whether serving freshly brewed, high-quality, and flavorful coffee could improve patient compliance and support the routine implementation of coffee as a post-surgical intervention. MethodsIn this prospective monocentric single arm study, we proposed to every patient undergoing elective colorectal surgery 3 daily doses of freshly made coffee with a capsule system over 3 days. Primary endpoints were compliance (x/total possible doses) and reasons for non-compliance. Secondary outcome was satisfaction of patients using a visual analogue scale (VAS: 0-10). Results50 patients were included for analysis. Median postoperative coffee consumption was 6 (IQR 5-8) during the first three post-operative days (POD), and was not modified after exclusion of patients with POI (n=5). Median compliance was 78% (IQR 56-100) and 35 patients (70%) drank more than 2/3 of possible doses. Compliance decreased post-operatively by POD 2 (Figure 1). The main reason for non-compliance was nausea (n= 28) (Table 1). Patients’ satisfaction with the coffee was high (mean VAS 8.2 ±1.6). ConclusionWe achieved high levels of compliance and satisfaction by offering a standardized yet personalized and freshly brewed coffee, paired with an enjoyable moment. Integrating therapeutic interventions with positive and enjoyable experiences demonstrates a promising strategy to enhance adherence to postoperative measures. 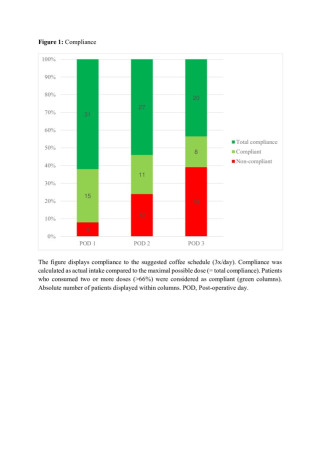

|
||
|
15:03–15:11
Side-to-End Colorectal Anastomosis Using the da Vinci Xi Linear Stapler
Christina Copei, Luzern
AbstractBackgroundThe side-to-end colorectal anastomosis technique is widely used in robotic colorectal resections. The colon is incised, the circular stapler anvil is inserted antimesenterically, and the colon is closed and transected distally with a linear stapler. The anastomosis is completed laparoscopically by transanal introduction of the circular stapler and docking it to the anvil. Standard laparoscopic linear staplers are commonly used for colon closure. AimsThis study evaluates the feasibility and safety of using the da Vinci Xi Sureform-60 linear stapler extracorporeally for side-to-end anastomoses and assesses its potential to reduce complications and costs by eliminating the need for an additional laparoscopic stapler. MethodsThe da Vinci Xi Sureform-60 linear stapler was routinely used for rectal transection and side-to-end colorectal anastomoses in robotic left colectomies/high anterior resections (for colon cancer or diverticulitis) and low anterior resections (for rectal cancer). A modified technique enabled the extracorporeal use of the stapler for colon closure and transection. This method was applied in 139 robotic colorectal resections performed between April 2018 and August 2024. ResultsThe cohort included 74 females (mean age 61.46 years) and 65 males (mean age 60.58 years). No intraoperative complications occurred. Postoperative complications included 2 cases of anastomotic bleeding (1.44%) and 7 anastomotic leaks (5.04%), all associated with the circular staple line. No complications were attributed to the linear staple line. ConclusionThe extracorporeal use of the da Vinci Xi Sureform-60 linear stapler for side-to-end anastomoses is feasible, safe, and cost-effective. Further studies with larger patient cohorts are needed to validate these findings. |
||
|
15:14–15:22
RIGHT HEMICOLECTOMY for LOW-GRADE APPENDICEAL MUCINOUS NEOPLASM (LAMN). IS IT NECESSARY?
Giacomo Bianco, Lugano
AbstractBackgroundLow-grade appendiceal mucinous neoplasms (LAMN) are rare appendiceal tumors characterized by a wide spectrum of clinical presentations and prognoses. Although the prognosis for LAMNs confined to the appendix is generally favourable, there remains a potential risk of progression to pseudomyxoma peritonei (PMP) and metastases. Historically, this risk has often led to extensive surgical resections for localized LAMNs, including ileocecectomy or right hemicolectomy. AimsThe aim of this study was to assess the necessity of performing a right hemicolectomy in the management of localized LAMNs. MethodsA comprehensive literature search was conducted across PubMed, Cochrane Library, Web of Science and Google Scholar databases to identify articles reporting cases of localized LAMNs treated with right hemicolectomy and with histopathological assessment of lymph node status. Studies involving cases without right hemicolectomy, with PMP or tumors other than LAMN, or lacking lymph node involvement data were excluded. ResultsA total of 21 articles published between 2009 and 2024 were included, reporting 99 cases of right hemicolectomy (44% open, 28% laparoscopic, 28% not reported). None of the cases had lymph node involvement upon histopathological examination. Only one patient underwent cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) after the right hemicolectomy. ConclusionThis is the largest systematic review of localized LAMNs treated with right hemicolectomy and with histopathological assessment of lymph node status. Based on our results, right hemicolectomy may not be necessary in the treatment of these tumors. |
||
|
15:25–15:33
A paradigm shift towards centralized colorectal cancer surgery – a nationwide audit using administrative data on 34’106 patients across ten years
Michaela Ramser, Zürich
AbstractBackgroundOncologic colorectal surgery has evolved significantly, leading to increasing surgical complexity necessitating subspecialty training. Concepts such as total mesocolic excision, D2/D3 lymphadenectomy or the widespread acceptance of robotics are known factors driving centralization. AimsThe aim of the present study is to analyze the distribution of colorectal cancer surgery by level of complexity and size / case numbers of hospitals involved. We sought to test whether a shift towards specialized cancer care with improved access to minimal-invasive techniques has occurred following political initiatives to centralize cancer care. MethodsThe national BFS (Swiss federal statistic office) database was queried including the years 2012-2022. Parameters of interest included case numbers per center, complexity of resections, patient age, cancer site, type of access and available outcome parameters including in-hospital mortality, morbidity, surgical site infections or reoperations. ResultsA total of 34’106 colorectal cancer resections (44.2% female) were performed during the study period. The majority of resections were performed in large, non-academic centers. Only three centers performed a median of more than 100 resections per year during the study period. The percentage of patients operated in smaller hospitals declined from 38% to less than 20%, with the greatest increase in oncologic resections noted in large cantonal hospitals (50% to 71%). 6.7% of resections were performed in patients <50 years of age (early-onset colorectal cancer) with a 30% increase in absolute terms over the analyzed period. A late but notable trend towards robotic access occurred on a national level. ConclusionDespite the previous acceptance of general surgery care for colorectal cancer patients, a paradigm shift towards centralized treatment has occurred in the past 10 years in Switzerland. This shift is accompanied by higher rates of robotic access and growing numbers of early-onset colorectal cancer, underscoring the increased complexity and contemporary expectance of specialized care in this frequent disease. |
||
|
15:36–15:44
The next step of surgical benchmarking: comparison of outcome data using the quality improvement cycle as shown in low anterior resections for rectal cancer
Michaela Ramser, Zürich
AbstractBackgroundThe aim of benchmarking is to compare one's own data with the published benchmark and to identify possible weaknesses in one's own practice. This comparison provides the basis for subsequent procedural changes to improve quality of outcomes, such as those in low anterior resections for rectal cancer. AimsThe aim of this project is to establish an algorithm to analyse and compare data with benchmark values and to systematically analyse deviations and initiate change within a quality improvement cycle (Fig1). We tested the methodology with the previously published benchmark for low anterior resections [doi:10.1093/bjs/znac300]. MethodsAll consecutive patients meeting inclusion criteria and treated surgically for a low and mid rectal adenocarcinoma in our department from January 2018 - December 2023 were analysed. The subgroups of ideal and non-ideal patients were formed according to the definitions. Each benchmark for ideal and non-ideal patients was displayed in a separate diagram. The moving median was calculated from our results for recurrent periods of 12 months with the calculation was repeated in intervals of 3 and 6 months resulting in 21 and 11 periods, respectively (Fig2). ResultsA total of 98 patients was analysed (16.3% ideal patients). For each of the 27 benchmarks in ideal and non-ideal patients, moving medians were calculated. The example of readmission rate within is shown in Fig3. Deviations from the benchmark (ideal patients: periods 8-11; non-ideal: 3-7 and 16-17) were highlighted for step 4 of the improvement cycle. Root cause analyses were carried out to understand the underlying problem when there were deviations observed. ConclusionThe methodology presented here enables surgeons to compare their data with published benchmarks in order to implement improvement initiatives where needed. Repeated cycles of comparison will ultimately lead to an optimization of outcome. 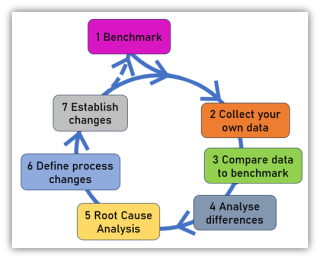
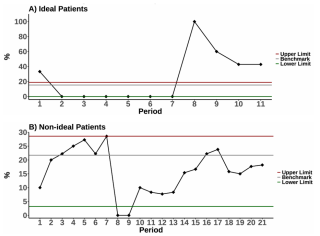
|
||
|
15:47–15:55
Long-Term Evolution of Skeletal Muscle Quantity and Quality After Curative-Intent Colorectal Surgery: A Retrospective Cohort Study
Argyri Papadimitriou, Genève / Sion
AbstractBackgroundComputed tomography-based sarcopenia is a predictor of complications and recovery after major surgery. Little is known about sarcopenia markers in the long term after oncological surgery and their predictive potential regarding long-term survival. AimsThe aim is to study the evolution of sarcopenia markers after colon cancer surgery. MethodsThis is a retrospective single-center cohort study including patients undergoing curative-intent surgery for colon cancer. Skeletal muscle attenuation (SMA), Skeletal muscle index (SMI), skeletal muscle radiation attenuation (SMRA), intermuscular adipose tissue (IMAT), and index (IMATI) were determined on axial CT slices at the level of the third lumbar space, before surgery and at 6, 12 and 24 months thereafter. Descriptive statistics were employed to describe the evolution of sarcopenia. Statistical correlation of sarcopenia markers and survival was analysed through Cox regression analysis. ResultsThe final cohort consisted of 102 patients, with a mean age of 66 years old (SD:13), 65.7% males and 34.3% females. The mean overall survival in the observation period of 24 months was 22 months. Eighty-five patients were alive at 24 months (83.3%), and forty-five (44.1%) had a CT scan at all times. Sarcopenia markers remained stable over time, except SMRA, which diminished: mean DSMRA at 24 months: -1.1 (SD:5.3, p-value: 0.549) and -3.5 (SD: 4.5, p-value 0.179), in males and females, respectively. Age (HR 1.07, 95% CI: 1.00 - 1.14) and ASA score (HR 2.4, 95% CI: 1.00 - 5.7) were independent factors correlated negatively with survival. A positive correlation was found with the DIMAT and DIMATI at 12 months, HR: 0.79 (95% CI: 0.67 - 0.93) and 0.49 (95% CI:0.30 - 0.80). ConclusionThe markers of muscle quantity (SMA/SMI) remained largely stable in the long-term follow-up after curative-intent colorectal surgery. SMRA, the marker of muscle quality, diminished in our cohort; Neither of the preoperative sarcopenia markers was predictive for survival. |
||
|
14:30 – 16:00
Auditorium B
|
Guardians of the Scalpel: Securing Excellence in Robotic Surgery
Lukas Brügger, Bern; Minoa Karin Jung, Geneva
|
|
|
Guardians of the Scalpel
|
||
|
14:30–14:45
Can a center survive without a robot?
Walter Brunner, St. Gallen
|
||
|
14:48–15:03
Which robotic platform is the best?
Fabian Grass, Lausanne
|
||
|
15:06–15:21
Which procedures should be performed robotically (where is the evidence)?
Matthias Turina, Zurich
|
||
|
15:24–15:39
How should a new robotic program be started?
Christian Toso, Geneva
|
||
|
15:42–15:57
When and how should robotic surgery be introduced in the surgical training?
David Fuks, Lausanne
|
||
|
14:30 – 16:00
Room 1C
|
Studies and Cases in Pediatric Sugery
Barbara Wildhaber, Geneva; Martina Frech-Dörfler, Basel
|
|
|
Free Communication
|
||
|
14:30–14:37
Save the Ovaries: Surgical Management of Simple Ovarian Cysts in Children and Adolescents
Rahel Moser, Zurich
AbstractBackgroundSimple ovarian cysts in girls are common and typically occur during phases of hormonal stimulation. While small cysts are treated conservatively, surgical intervention is required in cases of cyst growth or complications. The most common laparoscopic ovarian-sparing methods are laparoscopic cyst enucleation and cyst deroofing. Adult studies have shown low recurrence rates and a reduction in ovarian reserve following cyst enucleation compared to cyst deroofing. However, no studies have been found on this topic for girls. AimsWe aimed to compare laparoscopic cyst enucleation with laparoscopic cyst deroofing regarding postoperative recurrence rates and ovarian reserve in girls. MethodsWe conducted a retrospective multicenter study in two Swiss institutions. Pre- and postoperative demographic, clinical, and sonographic parameters were analyzed. Recurrence was defined as the presence of an ipsilateral ovarian cyst within 3 months postoperatively, while estimation of ovarian reserve was assessed using sonographic ovarian volume and the adnexal ratio. Descriptive statistics of demographic data were performed. Endpoints were analyzed using unadjusted risk differences, odds ratios, and linear regression models. ResultsFrom 2012 to 2022, 129 patients underwent surgery for simple ovarian cysts (enucleation: n=42, deroofing: n=65). The mean age at surgery was 13.6 years, and the mean preoperative cyst size was 53 mm. Postoperative recurrence rates were similar for both methods (deroofing: 9.5%, enucleation: 7.5%, p=0.786). However, ipsilateral ovarian volume and the adnexal ratio were lower after cyst enucleation, indicating a potential decrease in postoperative ovarian reserve. ConclusionWe demonstrated that laparoscopic cyst enucleation and cyst deroofing showed no difference in postoperative recurrence rates. Laparoscopic cyst enucleation appeared to have a more negative impact on postoperative ovarian volumes. The findings of our study will serve as basis for a planned prospective study and will help to standardize the surgical management of simple ovarian cysts in girls based on evidence, with the goal of preserving ovarian reserve. 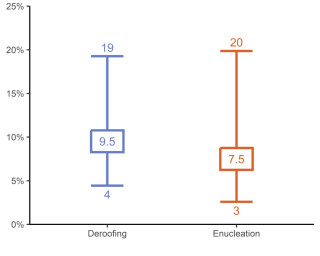
|
||
|
14:37–14:44
Pediatric Hepatic Alveolar Echinococcosis: Clinical Insights and the Need for a Centralized Database
Consuelo Maldonado, Geneva
AbstractBackgroundHepatic alveolar echinococcosis (HAE) is a rare, chronic, potentially life-threatening parasitic disease caused by Echinococcus multilocularis. Its clinical progression closely resembles that of a slow-growing malignant liver tumor. Symptoms typically emerge 10-15 years after infection, mostly leading to diagnoses in adulthood. However, pediatric HAE cases are being increasingly reported, presenting unique challenges in diagnosis and management due to limited awareness and available data. In Switzerland, the rising incidence of HAE highlights the need to improve understanding and refine management strategies in pediatric patients. AimsThis study aims to review the clinical characteristics and treatment outcomes of pediatric HAE through the analysis of four cases. MethodsWe retrospectively analyzed pediatric patients diagnosed with HAE between 12/2016 and 4/2023, treated in collaboration with the national Pediatric Liver Center. Data on clinical presentation, diagnostic approaches, treatment modalities, and outcomes were reviewed. ResultsFour pediatric patients (two male, two female), age at initial presentation 10 to 17 years, follow-up duration after diagnosis 18 to 95 months. Two underwent surgical R0-resection and antiparasitic therapy for two years postoperatively with no signs of relapse at the end of follow-up; the other two are receiving antiparasitic therapy alone, with regular follow-up imaging confirming lesion stability. Of the two patients managed conservatively, one declined surgical intervention despite it being offered, while the other is rescheduled for operability assessment at the two-year follow-up, as the current surgical approach carries a high morbidity risk. ConclusionPediatric HAE can be effectively managed with patient-tailored approaches based on disease severity and patient-specific factors, including a combination of surgery and time-limited antiparasitic therapy, or antiparasitic therapy alone. The creation of an international centralized pediatric HAE database will facilitate refining management strategies, and improving outcomes for this rare but serious condition. |
||
|
14:44–14:51
Autologous Blood Patch Pleurodesis as Treatment Option for children with Persistent Air Leaks (PAL) – an indicative Case Series
Sophie Güsewell, Luzern
AbstractBackgroundAutologous Blood Patch Pleurodesis (ABP) represents an established treatment method of PAL in the adult population. However, despite its low complication rate, the role of ABP among the pediatric population remains unclear regarding evidence of success. Case presentationOver the course of 5 months, we treated two children with persistent air leak (PAL) due to complicated pleuropneumonia. Case 1: Four-year-old boy, diagnosed with complicated pleuropneumonia and septated pleural empyema in the right chest. VATS was performed, a chest drain was placed, and intravenous antibiotic treatment was initiated. On POD 15, radiological diagnosis of a serous pneumothorax with mediastinal shift led to thoracic tube reinstallment. Due to recurrent unsuccessful attempts to reduce suction, tachypnea and persistent collapse of the right lung, ABP was performed. ABP was repeated once on POD 5. The postoperative course was uncomplicated, with gradual suction reduction and well-tolerated removal of the chest drain. The patient could be discharged on POD on oral antibiotic treatment. Case 2: Two-year-old girl with complicated pleural-pneumonia, underwent VATS, chest drain placement and intravenous antibiotic treatment. Despite improving symptoms, a septated pneumothorax was diagnosed on POD 5. Due to persistent air leak, ABP was performed on POD 12 and 15. The postoperative course was then uncomplicated, and the patient could be discharged on POD 10 on antibiotic treatment. ConclusionIn our presented case series, the effectiveness of ABP in children with PAL as complication for pleural pneumonia could be seen. Therefore, we consider ABP a safe and promising treatment option of persistent air leaks in children. |
||
|
14:51–14:58
Indocyanine Green-Enhanced Fluorescence in Pediatric Laparoscopic Palomo Varicocelectomy: A Lymphatic-Sparing Approach – Our Experience
Roberto Carulli, Bellinzona
AbstractBackgroundLaparoscopic Palomo varicocelectomy is a widely adopted surgical approach for treating pediatric varicocele. This study evaluates the use of indocyanine green (ICG)-enhanced fluorescence imaging to preserve lymphatic vessels during surgery. AimsTo describe our experience with ICG-guided laparoscopic varicocelectomy, focusing on its safety, feasibility, and outcomes. MethodsWe retrospectively reviewed the records of six patients who underwent laparoscopic left varicocelectomy at our unit between February 2022 and February 2024. The patients’ mean age was 16 years (range 14–17). All cases involved high-grade varicocele with left testicular hypotrophy or clinical symptoms. The procedure was performed laparoscopically with a 2 mL intratesticular injection of ICG. Fluorescence imaging allowed for clear identification and preservation of lymphatic vessels, followed by clipping of the spermatic bundle according to the Palomo technique. ResultsThe mean operative time was 55 minutes (range 43–65). No intraoperative complications, conversions to open surgery, or adverse reactions to ICG were reported. At a 6-month follow-up, no recurrences of varicocele or postoperative hydroceles were observed. The small sample size and retrospective design represent limitations, emphasizing the need for further validation in larger cohorts. ConclusionICG fluorescence imaging is a safe and effective tool for lymphatic-sparing laparoscopic Palomo varicocelectomy in pediatric and adolescent patients. This technique consistently allowed identification of lymphatic vessels with no reported complications. Future studies are recommended to validate these findings in broader populations |
||
|
14:58–15:05
The Role of Schede Casting Position in Pediatric Radial Fractures: Evidence from a Retrospective Analysis and Survey
Markus Denzinger, St. Gallen
AbstractBackgroundRadial fractures are among the most common fractures in children and adolescents. While surgical intervention is effective in correcting significant deformities, it is inherently invasive and associated with higher risks, including infection or anesthesia-related complications. Non-surgical approaches, such as immobilization in the Schede casting position, offer a potentially less invasive alternative, though evidence supporting its use remains limited. AimsThis study aimed to evaluate the effectiveness of the Schede casting position in improving deformity correction in pediatric radial fractures and to assess its acceptance and clinical experience among pediatric trauma surgeons. MethodsA survey was conducted among pediatric trauma surgeons to assess their experience with the Schede casting position. Additionally, a retrospective analysis compared radiographic outcomes between immobilization in the Schede casting position and standard casting positions in pediatric radial fractures. The primary outcome was the improvement in radiographic alignment, particularly in the sagittal plane. ResultsThe retrospective analysis demonstrated an improvement in fracture alignment with the Schede casting position compared to standard positioning, particularly in the sagittal plane on lateral radiographs. Survey responses revealed that many pediatric trauma surgeons reported positive clinical experiences with this technique, emphasizing its efficacy in reducing deformities and avoiding surgery in selected cases. ConclusionThe Schede casting position represents a promising, non-surgical approach for managing pediatric radial fractures, achieving significant deformity correction and potentially reducing the need for surgical intervention. These findings highlight the need for further prospective studies to validate these results and establish clear clinical guidelines. |
||
|
15:05–15:12
Responding to the Challenges of Global Children Surgery: An Implementation Program in Burkina Faso
Sophie Inglin, Geneva
AbstractBackgroundThe challenges are immense when it comes to enhancing the development of children surgery in low- and middle-income countries, in line with current recommendations for holistic and sustainable approaches. Our program, entitled Pediatric Surgery Development Plan in Burkina Faso, was specifically designed to respond to these challenges by tackling the pediatric surgical ecosystem, based on partnership, research and interventions at all levels of the healthcare system. AimsWe herein present our unique experience by reporting on the first four years of the program, focusing on the main actions and monitored indicators. MethodsThis program has been designed using the Global Initiative for Children's Surgery main pillars and preserving a fundamental health system strengthening approach. ResultsThe country's capacity for pediatric surgery has meaningfully been increased: i) A new infrastructure has relieved congestion in pediatric surgical care at the national level, ii) hundreds of professionals have benefited from skills enhancement, iii) the quality of care in the partner hospital has been optimized, iv) collaboration with traditional practitioners and families have been strengthened, v) research has enabled us to move forward in an evidence-based way, and vi) pediatric surgery in Burkina Faso has enjoyed a new impulse thanks to advocacy work. Quantitative results are summarized in Table 1. ConclusionThis program has not only helped to create a major impulse for the expansion of pediatric surgery in Burkina Faso, but also enriched the community of interest with a concrete implementation program to confirm the main challenge to overcome: integrating this most essential discipline into the wider framework of global health. 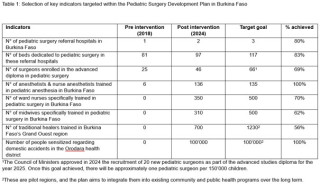
|
||
|
15:12–15:19
Management of Pediatric Pancreatic Trauma: Case Series and Review of Current Surgical Management
Miriam Luxenhofer, Luzern
AbstractBackgroundTraumatic injuries to the pancreas present a challenge in blunt abdominal trauma in children. The management include both surgical and non-surgical treatment options with an increasing preference towards non-operative management (NOM). Our aim is to illustrate the current concepts of surgical treatment for pancreatic injury in children. Case presentationWe present a case series of three pediatric patients with traumatic pancreatic injuries. Patient 1 (10-year-old male) presented with a proximal subtotal pancreatic rupture (grade IV, AAST) and acute hemorrhage, necessitating emergency laparotomy. Hemostasis was achieved, the proximal pancreatic duct was sutured, and a distal pancreatico-jejunostomy with a Roux-en-Y-anastomosis was performed. Patient 2 (8-year-old female) underwent emergency laparotomy for complete pancreatic rupture (grade IV, AAST) and acute hemorrhage. Hemostasis was achieved and a distal pancreatectomy was performed, with suture of the proximal pancreatic duct. Patient 3 (8-year-old male) sustained a traumatic pancreatic rupture (grade IV-V, AAST) and was transferred to our institution five days post-injury. Initially managed conservatively, the patient now presented with an acute abdomen. Emergency exploratory laparotomy was performed. Intraoperatively, a drain was placed in the Douglas pouch, and a chest tube was inserted to address pleural effusion. Subsequently, a functional duodenal stenosis due to a pancreatic pseudocyst developed, necessitating an upper gastrointestinal endoscopy with endoscopic ultrasound and endoscopic cystogastrostomy. All patients recovered quickly with full return to normal activities. ConclusionWhile NOM has demonstrated efficacy in select cases, early surgical intervention remains crucial in specific scenarios, particularly those with acute hemorrhage or involving pancreatic duct injuries, highlighting the necessity for individualized treatment concepts. 
|
||
|
15:19–15:26
Minimally Invasive Surgical Approach in Primary Fallopian Tubal Torsion: A Single-Center Experience
Marco Garatti, Bellinzona
AbstractBackgroundIsolated Fallopian tube torsion (IFTT) is a relatively rare condition affecting young female patients, presenting as nonspecific abdominal pain (acute or chronic), often associated with vomiting. Diagnosis through standard procedures is not always conclusive, and for most patients, the definitive diagnosis is achieved through minimally invasive surgical exploration. AimsTo share our experience in managing IFTT, focusing on the challenges of the diagnostic process and evaluating the role of minimally invasive surgery as a primary approach MethodsWe performed a retrospective case review series of pediatric patients with IFTT treated at our institution between 2021 and 2024. Clinical presentations, ultrasound efficacy, the utility of secondary imaging exams (CT and MRI), and types of surgical treatment were analyzed. ResultsFour cases of IFTT were included, all of whom with an associated paratubal cyst. Two patients underwent laparoscopic hemi-salpingectomy with ovarian preservation, while two required laparoscopic tubal de-rotation and fenestration of the cyst. MRI was used in all cases to complete the diagnostic process. ConclusionDue to its low frequency and the lack of clear guidelines, diagnosing IFTT remains challenging. MRI appears to facilitate the diagnostic process. A laparoscopic approach is safe, feasible, and remains the gold standard for treatment. We propose our protocol to enable prompt diagnosis and avoid extensive surgical interventions. |
||
|
15:30–15:33
Spigelian-Cryptorchidism Syndrome in a Preterm Infant: Management by Laparoscopic Assisted Orchidopexy and Open Herniorraphy.
Alberto Gubert, Lausanne
AbstractBackgroundSpigelian hernia (SH) is a rare abdominal wall defect in infants. SH can be associated with ipsilateral cryptorchidism, with the testis located within the hernia – referred to as Spigelian-cryptorchidism syndrome. Case presentationA male preterm infant born at 28 weeks of gestational age developed at 11 weeks of age a painless right abdominal wall swelling. The location was consistent with a SH. The right hemiscrotum was empty and an ectopic testis was palpable within the swelling. Abdominal ultrasound confirmed a SH containing a loop of small bowel and the right testis of appropriate size. At the time of diagnosis the infant was requiring respiratory support for bronchopulmonary dysplasia, therefore surgery was postponed. At 11 months of age, a laparoscopic assisted right orchidopexy and open hernia repair were performed. Laparoscopy allowed very good recognition of a 2 cm wall defect above a closed deep inguinal ring, lateral to the right rectus abdominis muscle. The right testis, with normal looking vas deferens and blood vessels, as well as the right colon were contained within the hernia sac. The SH was repaired by open herniorraphy. The recovery was uneventful, and the patient was discharged on postoperative day 1. Follow-up up to now (3 months) showed no complication. ConclusionA laparoscopic guided approach allows for better understanding of the location and the size of the wall defect, length of the testicular vessels and presence of inguinal canal and gubernaculum. To our knowledge, this is the first reported case of Spigelian-cryptorchidism syndrome in a preterm infant. In Spigelian-cryptorchidism syndrome, preoperative abdominal ultrasound can help assess the presence of the testis within the SH and guide surgical planning. 
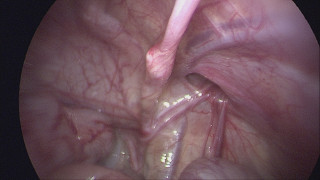

|
||
|
15:33–15:36
Robotic Transabdominal Preperitoneal Repair for Epigastric Hernia in a 16-Year-Old Patient: A Case Report
Marco Garatti, Bellinzona
AbstractBackgroundRobotic epigastric hernia repair using the transabdominal preperitoneal (rTAPP) approach is a well-established technique in adult patients. The robotic approach enhances precision, improves ergonomics, and reduces complication rates. However, there is limited evidence regarding its application in the pediatric field. This report describes the case of a 16-year-old female patient who underwent rTAPP surgery for an epigastric hernia. AimsTo highlight the feasibility and efficacy of robotic transabdominal preperitoneal repair in managing epigastric hernias in pediatric patients, particularly in the presence of obesity MethodsWe present the case of a 16-year-old Caucasian female with a history of chronic supraumbilical abdominal pain lasting over five years. The patient’s medical history included Cornelia de Lange syndrome with developmental delay, exogenous obesity, insulin resistance, and pilonidal disease. An ultrasound revealed an epigastric hernia defect. Robotic transabdominal preperitoneal repair was performed using standard rTAPP technique ResultsThe robotic repair successfully addressed the epigastric hernia, resulting in significant post-surgical pain relief. The approach was effective in overcoming the challenges posed by the patient’s obesity, demonstrating the precision and adaptability of robotic techniques in complex pediatric cases. ConclusionThe experience gained from rTAPP in adults can be effectively translated to the pediatric population. This case highlights the potential of robotic surgery to address complex pediatric hernias. Further research is needed to build a robust case series and establish appropriate criteria for surgical indications in pediatric patients |
||
|
15:36–15:39
Penetrating head injury after horse riding injury – a case report
Johanna Eber, Luzern / Lucerne
AbstractBackgroundPenetrating head injuries are not common in children but can represent major trauma. Case presentationWe present a 14-year-old girl with penetrating head injury after horse riding injury. During transportation she was always awake and responsive, however developed monocular hematoma. On arrival at our emergency department, we found a left frontal laceration, the frontal bone visible and horsehair contaminating the wound. A CT scan revealed a 2 cm depressed skull cap fracture involving the frontal sinus, the roof and floor of the orbita and the left maxillary sinus. The open fracture was explored through coronal incision. We performed a cranioplasty of the orbital roof, microsurgical dural plasty, reconstruction of the periorbita and osteosynthesis of the orbital roof and the frontal bone with lactosorb re-absorbable plates and screws. Postoperative transfer to the pediatric intensive care unit for one day, then transfer to the normal pediatric surgical ward. The patient received antibiotic treatment for five days, drains could be removed after three days. Glasgow-Coma-Scale (GCS) monitoring was always 15. Ophthalmologic examinations revealed regular findings both initially and during hospitalization. The patient could be discharged on postoperative day 8, outpatient rehabilitation was carried out. Two months postoperative, there are no postoperative complications, but the patient is still not able to attend school for a full day. ConclusionThe patient always revealed a GCS score of 15, however proved to have a significant open traumatic brain injury, whose true extent could only be seen in cCT. Scandinavian guidelines suggest a further subdivision of mild traumatic brain injury; in the presence of risk factors such as clinical signs of an impression fracture, CT imaging is primarily indicated. |
||
|
15:39–15:42
Biliary complication under nonoperative management in high-grade liver injury: a case report
Jonathan Lovis, St. Gallen
AbstractBackgroundNonoperative management (NOM) of isolated solid organ injury in pediatrics is an established way of treatment in hemodynamically stable patients. However, close monitoring and reevaluation are indicated, as complications may occur and may need diagnostic or therapeutic adjuncts. Among them, traumatic bile leak (TBL) requires a multidisciplinary approach. Case presentationWe report a 13-year-old male with AAST grade IV liver injury qualifying for NOM after initial hemodynamic stabilization. The clinical course was complicated with increasing amounts of intra-abdominal free fluids leading to laparoscopic exploration and later on diagnosis of biliary leak. The patient was then treated with biliary stenting and iterative ERCP procedures, documenting a successful management of the biliary leak. ConclusionA high index of suspicion of complications must be maintained in patients selected for nonoperative management, including TBL. ERCP may be considered as an adjunct in the NOM in appropriate cases. 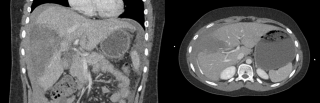
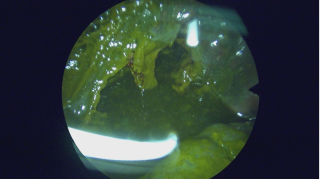

|
||
|
15:42–15:45
Full Thickness Genitoperineal Pressure Ulcer in a Female Pediatric Patient Undergoing Orthopedic Surgery on a Traction Table: A Case Report
Martina Bärtsch, Zürich
AbstractBackgroundTraction tables are widely used in orthopedic procedures. Although rare, potential complications include nerve injuries, fractures, and soft tissue damage. This case report documents the first reported case and management of extensive genitoperineal necrosis in a pediatric patient following femoral fracture fixation related to a traction table. This case report aims to describe the presentation, management, and long-term implications of genitoperineal necrosis related to the use of an orthopedic traction table as well as to raise awareness, and to propose strategies for prevention in the pediatric population. Case presentationA 10-year-old girl underwent closed reduction and intramedullary nail fixation of a femoral shaft fracture using a traction table with standard padding and positioning. Operative time was 183 minutes. At the end of the procedure an extensive full thickness pressure necrosis in the genitoperineal area was observed. Postoperatively, a multidisciplinary team involving plastic surgery, urogynecology and orthopedic surgery managed the wound conservatively including topical antiseptics, local steroids and estrogens. No surgical intervention was needed but several sedations for wound care. A transurethral catheter was left in place for 25 days for pain and wound management. The patient was hospitalized for 28 days. Full wound epithelialization was achieved after 44 days. At seven months follow-up, the patient did not exhibit any urinary complaints or pain, however synechiae involving the clitoral hood and labia minora had developed. Further follow-up is planned and surgical correction of synechiae will most likely be necessary during puberty. ConclusionThis case highlights the vulnerability of pediatric soft tissue to ischemic damage during prolonged traction table use. Preventative strategies should include increased awareness, team education, minimizing operating time, optimizing padding, and considering intraoperative tissue perfusion monitoring. Multidisciplinary care and long-term follow-up are essential to address such complications. Genitoperineal injuries usually respond well to conservative management without need for a primary surgical approach. |
||
|
15:45–15:48
Spondylodiscitis Following Button Battery Ingestion - A Rare, Severe Long-Term Complication
Benjamin Hasler, Luzern
AbstractBackgroundButton battery ingestion with esophageal impaction can result in severe, potentially life-threatening complications, including long-term sequelae. Case presentationA case of a 22-month-old boy with a button battery impacted in the upper esophagus, immediately removed after an impaction time of 4 hours is presented. The patient was treated with a naso-gastric tube, maintained npo, and given intravenous antibiotic treatment and a PPI. Subsequent MRI revealed reactive mediastinitis, which resolved within 8 days. On day 10, a fibrin patch persisted on the dorsal wall at the site of impaction. Antibiotic treatment were discontinued, oral liquids were started and well tolerated, and the patient was discharged on day 13. On day 17, the esophageal mucosa was fully restored. However, after 6 weeks a polypous structure was noted at the impaction site, limiting the patient to soft foods or small portions. An MRI at 10 weeks revealed spondylodiscitis of T1/T2, with a fistula between the esophagus and the intervertebral disc. However, the patient remained asymptomatic except for dietary limitations. He was treated with a 6-week course of antibiotic treatment, including 14 days of intravenous therapy at the beginning. Systemic inflammation markers became apparent only 6 days after initiating the antibiotic treatment. The spondylodiscitis resulted in a bony defect at the ventral edge T1/T2 accompanied by mild kyphosis. At 12 months post-ingestion, the patient recovered to full without clinical symptoms. ConclusionSpondylodiscitis is a rare but severe complication of button battery ingestion that can develop subclinically. While the immediate removal of an impacted button battery is crucial to minimizing severe and potentially life-threatening complications, such as for example esophageal-aortic fistulas, long-term follow-up is equally crucial. In cases of abnormal findings, endoscopic and magnetic resonance imaging is indicated to evaluate and manage these patients effectively. |
||
|
15:48–15:51
Acute on chronic decompensation of a Chiari I Malformation in a 5 y/o boy following traumatic c0/c1 instability.
Franziska Wunderlich, Luzern
AbstractBackgroundTrauma-related epidural haematoma dorsal to the clivus down to the level of C1 following sports related TBI in infants and children is a rare condition. Case presentationWe present a 5 ½ year old boy who presented with sub-febrile temperatures three days after traumatic brain injury with brief unconsciousness following a skiing accident. Initial clinical assessment showed a left abducens and hypoglossal palsy. There was also latent strabismus, persistent neck pain, as well as increased fatigue. A low dose CCT revealed an epidural haematoma with compression of the medulla oblongata and a cranio-cervical dissociation. A surgical cranio-cervical fixation and a suboccipital decompression of the foramen magnum was performed. Post-traumatic cerebrospinal fluid circularisation disorder later developed at the level of the posterior fossa potentially accentuated by the Chiari I malformation, therefore a ventricular-peritoneal shunt was placed. ConclusionThis case represents a rare and complex post-traumatic injury related to a previously not apparent and undiagnosed malformation. Children suffering from TBI with cranial nerve deficit should be carefully observed for clival fractures and hematomas and/or consecutive traumatic instability of the cranio-cervical junction respectively. |
||
|
14:30 – 16:00
Room 4BC
|
Surgery of the immunocompromised patients
Valentine Luzuy-Guarnero, Geneva; Fariba Abbassi, Zurich
|
|
|
Main Session
|
||
|
14:30–14:50
Which immunosuppressives need to be reduced preoperatively?In an elective setting
Giulia Piazza, Lausanne
|
||
|
14:52–15:12
Which immunosuppressives need to be reduced preoperatively?In the emergency situation
Lilian Salm, Bern / Calgary
|
||
|
15:14–15:34
How to handle patients with adrenal insufficiency perioperatively
Arnaud Rey, Lausanne
|
||
|
15:36–15:56
Main surgical strategy differences in immunocompromised patients
Eva Breuer, Zurich
|
||
|
14:30 – 16:00
Room 5B
|
Upper GI
Hugo Teixeira Farinha, Lausanne; Stefan Gutknecht, Zurich
|
|
|
Free Communication
|
||
|
14:30–14:37
The BARIREF Study: BARIatric Surgery Complications in Patients with Prior REFlux Surgery in a Large National Cohort.
Francesco Abboretti, Lausanne
AbstractBackgroundObesity and gastroesophageal reflux disease (GERD) often coexist, posing clinical challenges. Fundoplication is the standard treatment for GERD refractory to medical therapy. Managing obesity after fundoplication is complex and while RYGB is preferred for addressing both obesity and GERD, its use post-fundoplication requires further evaluation. AimsTo assess the outcomes of Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) in patients with prior fundoplication. MethodsRetrospective analysis of a national French database of patients undergoing RYGB and SG between 2013 and 2023. Patients were grouped according to prior fundoplication (PriorF) or no fundoplication (NoF). Baseline demographics and 90-day postoperative outcomes were assessed. Univariate and multivariate analyses identified risk factors; 1:5 matching was applied based on sex, age, body mass index, comorbidities, surgery year, and procedure type. ResultsAmong 372'464 patients, 337 (0.1%) had prior fundoplication. PriorF patients had higher rates of severe postoperative complications (Dindo ≥ IIIa: 8.9% vs. 3.7%, p < 0.001), longer hospital stays (4.5 ± 4.9 vs. 3.7 ± 2.9 days, p < 0.001), and higher readmission rates (17.8% vs. 9.9%, p < 0.001). Multivariate analysis for RYGB showed no significant association between prior fundoplication and complications (OR 1.66, 95% CI 0.98–2.62, p = 0.059). Prior fundoplication was independently associated with increased complications after SG (OR 2.83, 95% CI 1.59–4.66, p < 0.001). ConclusionPrior fundoplication increased postoperative complications after SG but not after RYGB. RYGB appears to be the a safer bariatric procedure in patients with prior fundoplication. Management should be performed in high-volume centers with bariatric expertise. |
||
|
14:50–14:57
Unveiling Gender Disparities in Postoperative Outcomes After Oncological Gastrectomy – A Global Multicenter Analysis
Elena Gantert, Zürich
AbstractBackgroundIn the past, studies have indicated a better prognosis in women with gastric cancer. Nevertheless, gender differences in gastric cancer treatment and survival, especially regarding postoperative outcomes, remain poorly investigated. AimsThe aim of this retrospective cohort study is to evaluate gender-related differences in patient characteristics and postoperative outcomes following oncological gastrectomy. MethodsWe analyzed 9351 oncological gastrectomies performed between January 1, 2017, and December 31, 2021, across 43 centers on five continents. The primary endpoints were gender-related differences in postoperative complications and morbidity, assessed using multivariable logistic regression. Propensity score matching was employed to balance baseline characteristics. ResultsThe cohort consisted of 3516 female and 5835 male patients. Male patients were older (66 (IQR 57-74) vs 64 (IQR 54-73)), had higher BMI, ASA scores and more advanced tumor stages, while females had more diffuse tumors and R+ resections (Table 1). Male patients had significantly more overall (27.3% vs. 22.4%) and major (15% vs. 10.8%) complications. Similarly, escalation of care, reoperations, readmissions and 90day mortality (2 vs 1.3%, Table 2) were decreased in women. In crude multivariate analysis, male gender was a risk factor for specific complications such as anastomotic leakage (3.4% vs. 2.0%) and pulmonary complications (6.0% vs. 4.1%). After matching 1685 patients of both genders, male gender remained a predictive factor for overall and major complications, anastomotic leakage, and pulmonary morbidity. In contrast, male gender was not associated with mortality, infectious complications and R+ status (Figure 1). ConclusionThis large, multicenter cohort study highlights significant gender-related disparities in postoperative outcomes after oncological gastrectomy. Male gender is an independent risk factor for major complications, anastomotic leakage, and pulmonary complications. These findings underscore the need for gender-specific risk stratification and tailored perioperative management strategies in gastric cancer surgery. 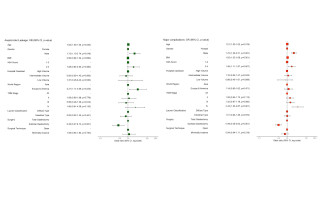
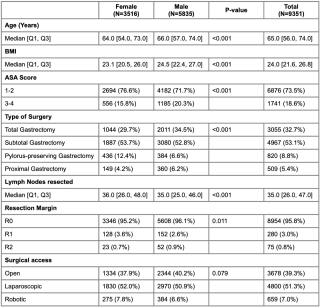
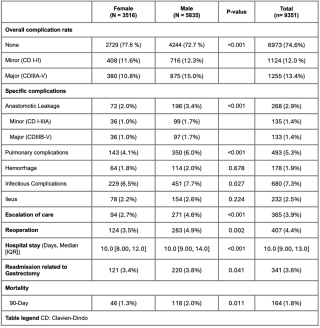
|
||
|
15:00–15:07
Outcomes of Minimally Invasive Median Arcuate Ligament Release: Symptom Improvement and Quality of Life Assessment
Pauline Aeschbacher, Bern
AbstractBackgroundMedian arcuate ligament syndrome (MALS) is a rare and complex condition with both vascular and neurologic components. Surgical repair is the treatment of choice; however, the proximity of the surgical field to the aorta and celiac trunk presents significant challenges. AimsThis study aims to evaluate symptom improvement and postoperative quality of life (QoL) in patients undergoing minimally-invasive median arcuate ligament release (MALR) at our institution. MethodsA retrospective analysis was conducted on patients undergoing minimally invasive MALR between 2017 and 2021. Patient characteristics, postoperative morbidity, symptoms before and after surgery, and postoperative quality of life using the 2-Item Short-Form Health Survey were assessed. ResultsThirty patients underwent laparoscopic MALR, with 80% (n=24) being female. The median age was 32 years (range: 18–63), and the median BMI was 20.3 kg/m² (range: 14.4–32.4). The predominant symptom at presentation was abdominal pain (29 of 30 patients). The median time from symptom onset to diagnosis was 12 months (range: 3–59 months). Laparoscopic MALR was performed without conversion, and no major postoperative morbidity was observed. Median follow-up was 24 months (range 6- 48 months). Symptom resolution or significant improvement was reported in 80% of patients (n=24). Postprandial symptoms showed a trend of reduction but were not statistically significant: nausea (50% to 33%), vomiting (17% to 7%), and diarrhea (30% to 13%). Bloating symptoms remained unchanged. Postoperative quality of life, assessed with the 2-Item Short-Form Health Survey, revealed generally positive outcomes across all domains (health change: 80(+/-18), pain:78(+/-20), emotional:82.7 (+/-24) and physical limitations:78(+/-32), and social functioning: 77(+/-24)). ConclusionMinimally invasive MALR is a safe procedure that results in symptom improvement in most patients. However, some gastrointestinal symptoms might persist at follow-up underscoring the importance of managing patient expectations and thoroughly excluding other gastrointestinal conditions. |
||
|
15:10–15:17
Superior polar gastrectomy
Hugo Teixeira Farinha, Lausanne
AbstractBackgroundSuperior polar gastrectomy is a technically demanding procedure typically reserved for tumors and lesions located near the esophagogastric junction. These cases pose significant challenges due to the anatomical complexity and the need to balance oncologic safety with functional preservation. Here, we report the case of a 38-year-old patient successfully treated with superior polar gastrectomy and jejunal interposition for a subcardial gastrointestinal stromal tumor (GIST). AimsTo present, through a detailed video, the feasibility and efficacy of laparoscopic superior polar gastrectomy with jejunal interposition using Roux-en-Y reconstruction for the management of a challenging GIST near the esophagogastric junction, while preserving functionality and minimizing morbidity. MethodsA 38-year-old female was diagnosed with a subcardial GIST measuring 7 cm near the esophagogastric junction. Following neoadjuvant therapy with Imatinib, the tumor size was reduced to 4 cm, achieving stable disease on radiological evaluation. During the laparoscopic procedure, the tumor's precise localization was confirmed intraoperatively using esophagogastroduodenoscopy, revealing that the lesion involved more than one-third of the esophagogastric junction circumference. A superior polar gastrectomy was then performed, resecting the esophagogastric junction. Reconstruction involved jejunal transposition with Roux-en-Y technique, including a circular end-to-side esophagojejunostomy, a side-to-side stapled jejunogastrostomy, and a manual side-to-side jejunojejunal anastomosis. ResultsThe procedure was completed laparoscopically without intraoperative complications. The patient was discharged on postoperative day 8, tolerating oral intake well and reporting no reflux symptoms. Pathological analysis confirmed a complete (R0) resection with clear margins, achieving both oncologic and functional success. ConclusionThis case highlights the successful application of laparoscopic superior polar gastrectomy with jejunal interposition, a rare but well-documented procedure for tumors near the esophagogastric junction. While technically demanding, this approach demonstrates the potential to achieve good oncologic and functional outcomes. Its successful execution underscores its value as a valuable option for carefully selected cases. |
||
|
15:20–15:27
Esophageal Perforation: Aggressive Nonoperative Treatment as a Viable Option
Pauline Aeschbacher, Bern
AbstractBackgroundEsophageal perforation (EP) is a rare but life-threatening emergency with high mortality, often due to mediastinal exposure to gastrointestinal contents, leading to severe inflammation and multiorgan failure. Historically, surgical intervention was the mainstay for EP management, particularly in patients with sepsis, non-contained perforations, or underlying esophageal disease. However, advancements in endoscopic and radiological drainage have increasingly enabled nonoperative (NONOP) approaches. AimsThis study aimed to evaluate management of EP at our institution in regards to surgical and nonoperative management. MethodsWe retrospectively analyzed patients treated for EP at our institution from 2003 to 2022. Exclusion criteria included esophageal lesions detected and repaired, chronic fistulas, or anastomotic insufficiencies. NONOP management comprised multidisciplinary approach with antibiotic and antifungal therapy, nutritional support, and endoscopic or radiological drainage of pleural and mediastinal collections. Surgical intervention (SURG) included oesophageal resection, surgical suture and drainage. ResultsAmong 172 patients, 146 (84.9%) underwent NONOP management (n=19 conservative therapy only), and 26 (15.1%) required surgery (n=7 esophageal resections, n=13 esophageal sutures). A trend toward increased use of NONOP was observed over time. Baseline characteristics were similar between groups. NONOP patients more frequently presented iatrogenic perforations and contained leaks (p=0.014) and had lower rate of septic shock (p=0.026), respiratory distress (p=0.018), or delays >24 hours (p=0.049). NONOP achieved a 94.5% healing rate and 5.5% mortality, comparable to SURG outcomes (92.3% healing, p=0.178; 11.5% mortality, p=0.375). NONOP had shorter length of ICU (p<0.001) and hospital stay (p=0.001). Successful NONOP treatment was associated with benign etiology, perforations in the proximal or distal esophagus, early diagnosis, and absence of empyema or sepsis. Importantly, NONOP was also effective in unstable patients with septic shock when drainage was feasible. ConclusionAggressive NONOP management is an effective alternative for EP, even in critically ill patients, provided septic foci are adequately drained. 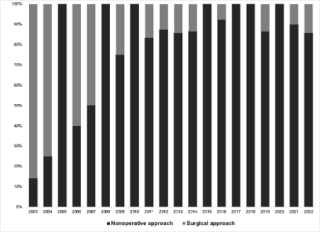
|
||
|
15:30–15:37
Hiatal hernia repair with the Dexter Robotic System™
Lisa Abry, Winterthur
AbstractBackgroundHiatal hernia repair is a challenging procedure requiring precision and meticulous surgical technique to achieve optimal outcomes. Robotic-assisted surgery provides enhanced dexterity and visualization, making it ideal for managing complex hernias. The Dexter Robotic System™ offers a compact, modular platform designed to optimize surgical efficiency and adaptability in minimally invasive procedures. AimsThis small case series aims to demonstrate feasibility, safety, and short-term outcomes of robotic-assisted hiatal hernia repair using the Dexter System. MethodsSeven patients underwent robotic-assisted hiatal hernia repair with or without mesh repair and fundoplication in one year (11/2023 – 11/2024) in a tertiary referral center, performed by one experienced hernia surgeon using Dexter. Indications included paraesophageal and hiatal hernia with or without gastroesophageal reflux disease. Detailed surgical steps are shown in the accompanying video. Perioperative data and short-term (6 weeks) patient outcomes were retrospectively reviewed. ResultsMedian age was 69 years (range 58-78). Median procedure time was 138 minutes (range 129-255 minutes) and decreased as experience grew. Meanwhile, the robotic console time increased during the period, with a median of 74 minutes (range 45-100 minutes). There were no intra-operative complications. The mean hospital stay was 3,4 days (range 2-4). There were no relevant post-operative complications (Clavien-Dindo Grade ≥ 2). Four patients experienced minor dysphagia in the first weeks after the operation. ConclusionThe initial learning curve appears relatively short for experienced minimally invasive hernia surgeons. The use of a lightweight, open and sterile robotic system makes the transition from laparoscopic to robotic operation easy. This video highlights the successful use of Dexter for hiatal hernia repair. The system’s design facilitates precise dissection and suturing, offering a reliable approach for managing anatomically complex cases. Further experience and training of different surgeons are needed to investigate advantages for patient outcome and implementing the robotic system further. |
||
|
15:40–15:47
All About Timing: Optimizing Surgery Intervals After Neoadjuvant Therapy in Esophageal Cancer
Sarah Gerber, Bern
AbstractBackgroundThe current standard of care for curative treatment of esophageal cancer consists of neoadjuvant therapy followed by resection. However, the interval between neoadjuvant therapy and esophagectomy has been widely debated. For both protocols – CROSS and FLOT - resection within 6 to 8 weeks is suggested. These recommendations aim to balance tumor control with perioperative recovery. However, prolonged intervals may offer patients critical recovery time to improve nutritional and physical status before surgery. AimsThis study investigates whether extending the interval beyond 8 weeks affects oncologic outcomes, focusing on tumor response and survival. MethodsWe conducted a retrospective analysis of 184 patients with esophageal adeno or squamous cell cancer treated with neoadjuvant radiochemotherapy (adapted CROSS protocol) or chemotherapy (FLOT) between 2014 and 2022. Patients were categorized into three groups based on the interval from completion of neoadjuvant therapy to surgery: early (≤8 weeks), intermediate (8–12 weeks), and late (>12 weeks). Outcomes included pathologic response (TNM/UICC staging) and overall survival (OS). Statistical analysis assessed differences between groups. ResultsBaseline characteristics, including demographic factors and tumor-related variables were comparable across the early (n=41), intermediate (n=80), and late (n=63) groups. Most common tumor type was adenocarcinoma (n=149), followed by squamous cell cancer (n=30). Pathologic tumor response (downstaging based on TNM/UICC criteria) was similar among the groups, with no significant differences in rates of complete or partial response. Survival analysis also revealed no statistically significant differences in overall survival (OS) between the groups with a median OS of 39 months (24.7-53.3) in the early, 62 months (29.3-94.7) in the intermediate and 45 months (22.7-67.3) in the late group (p=0.253). ConclusionThis study supports the safety of delaying esophagectomy beyond the traditionally recommended 4–8 weeks, particularly to an intermediate interval of 8–12 weeks. Allowing additional time may enhance patient recovery and preoperative fitness without adversely affecting oncologic outcomes. 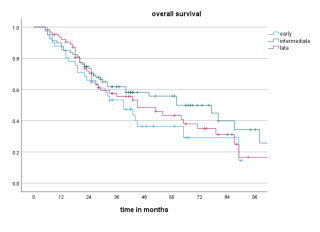
|
||
|
14:30 – 15:40
Room 1A
|
Young Residents Forum
Sébastien Déglise, Lausanne; Silvan Jungi, Bern
|
|
|
Main Session
|
||
|
14:30–14:40
Presentation of the new education program
Thomas Wolff, Basel
|
||
|
14:40–14:50
How and when to organize a fellowship in vascular surgery
Silvan Jungi, Bern
|
||
|
14:50–15:00
Work-life balance in vascular surgeryTrainee point of view
Camilla Schürmann, Bern
|
||
|
15:00–15:10
Work-life balance in vascular surgeryTeacher point of view
Arno Stellmes, Lucerne
|
||
|
15:10–15:20
How to improve skills in VS in 2025: what do I expect as a trainee?In the OR
Pietro Federico Ricciardi, Lausanne
|
||
|
15:20–15:40
Round table and discussion |








